Abstract
Anaphylaxis is an acute, life-threatening, multisystem syndrome resulting from the sudden release of mediators by mast cells and basophils. Although anaphylaxis is often under-communicated and thus underestimated, its incidence appears to have risen over recent decades. Drugs are among the most common triggers in adults, being analgesics and antibiotics the most common causal agents. Anaphylaxis can be caused by immunologic or non-immunologic mechanisms. Immunologic anaphylaxis can be mediated by IgE-dependent or -independent pathways. The former involves activation of Th2 cells and the cross-linking of two or more specific IgE (sIgE) antibodies on the surface of mast cells or basophils. The IgE-independent mechanism can be mediated by IgG, involving the release of platelet-activating factor, and/or complement activation. Non-immunological anaphylaxis can occur through the direct stimulation of mast cell degranulation by some drugs, inducing histamine release and leading to anaphylactic symptoms. Work-up of a suspected drug-induced anaphylaxis should include clinical history; however, this can be unreliable, and skin tests should also be used if available and validated. Drug provocation testing is not recommended due to the risk of inducing a harmful reaction. In vitro testing can help to confirm anaphylaxis by analyzing the release of mediators such as tryptase or histamine by mast cells. When immunologic mechanisms are suspected, serum-sIgE quantification or the use of the basophil activation test can help confirm the culprit drug. In this review, we will discuss multiple aspects of drug-induced anaphylaxis, including epidemiology, mechanisms, and diagnosis.
Keywords: anaphylaxis, drugs, IgE, MAS-related G protein-coupled receptor, IgG, in vivo diagnosis, in vitro tests
Introduction
Anaphylaxis is a severe, potentially life-threatening, generalized, or systemic hypersensitivity reaction that results from the sudden release of mediators derived from mast cells and basophils via degranulation (1–3). Drugs are the most common anaphylaxis triggers in adults (4–6), representing up to 10% of overall causes in outpatient studies (7), whereas for emergency department and hospitalized patients the proportion ranges from 27–60% (4, 8, 9).
While the symptoms of anaphylaxis can involve any organ, the most commonly affected are the cutaneous (affecting around 88% of cases), respiratory (76.1%), cardiovascular (41.9%), and gastrointestinal systems (12.8%) (10). Severe reactions (associated with hypotension) are more likely to be drug induced (4), representing up to 58% of fatal anaphylaxis (11).
Although anaphylaxis usually presents as an acute episode, mast cells can release mediators hours after the initial reaction causing a biphasic or late phase reaction. These biphasic and protracted cases can occur in up to 10% of drug-induced anaphylaxis instances (12).
In this paper, we will review the epidemiology, mechanisms, in vivo and in vitro diagnosis, and management of drug-induced anaphylaxis.
Epidemiology of Drug-Induced Anaphylaxis
Estimates of the prevalence of anaphylaxis can vary, mainly due to a lack of consensus on the definition of anaphylaxis, the source of data, and populations evaluated. One study calculated an overall incidence of 3–50 per 100,000 person years and a lifetime prevalence of 0.05–2% (8). The incidence of drug-induced anaphylaxis has been estimated to range from 0.04 to 3.1% (13–15) and to be responsible for one case in every 4,000 emergency department visits (16), with a fatality rate of 0.65% (17). In terms of changes over time, drug-induced anaphylaxis has increased by 150% and mortality rates by 300% in parallel with an increasing incidence of overall anaphylaxis from 1997 to 2005 (4).
Drugs Causing Anaphylaxis
Anaphylaxis can be induced by a range of drugs, being analgesics and antibiotics the most commonly involved, which may be partly explained by their frequent use in current medical practice (9, 10, 18).
Non-Steroidal Anti-inflammatory Drugs (NSAIDs)
Non-Steroidal Anti-inflammatory Drugs are the most frequent triggers of drug-induced anaphylaxis, being responsible for 48.7–57.8% of incidents (10, 18). These are typically immunological reactions (19) that can be driven by an IgE-dependent mechanism with sufferers showing tolerance to other strong COX-1 inhibitors (19, 20). However, anaphylaxis induced by cross hypersensitivity to NSAIDs, driven by an IgE-independent mechanism, has also been described (21–23). The most common culprits are pyrazolones, propionic acid derivatives, diclofenac, and paracetamol (10, 19, 22, 24). The incidence of NSAID-induced anaphylaxis with concomitant asthma, rhinosinusitis, and nasal polyps ranges from 2%, in children, to 97%, in adults (25). The prevalence ranges from 0.06 to 0.9% (26), with acetyl salicylic acid accounting for approximately 3% of all instances of anaphylaxis (27).
Beta-Lactam Antibiotics
Beta-lactams represent the second most frequent cause of drug-induced anaphylaxis, accounting for 14.3% of cases (18), with amoxicillin being the most common trigger (5). Recently, clavulanic acid, usually prescribed in combination with amoxicillin, has also been implicated (28, 29). Cases with cephalosporins, carbapenems, and monobactams are rare (30–32). The rate of anaphylactic reactions to beta-lactams has been estimated to be between 1 and 5 per 10,000 patient courses of treatment (33) and these drugs account for 75% of all fatal anaphylactic episodes in the US each year (34).
Non-Beta-Lactam Antibiotics
Up to 75% of patients with immediate hypersensitivity to fluoroquinolones develop anaphylaxis, with moxifloxacin being the most common culprit, followed by ciprofloxacin (35). As a whole, fluoroquinolones are responsible for 9% of severe antibiotic anaphylaxis (31).
Anaphylaxis to sulfonamides, trimethoprim, and macrolides are rare (36, 37). Cases of vancomycin IgE-mediated anaphylaxis have been occasionally reported (38); however, this drug more commonly induces direct mast cell stimulation, associated with rapid intravenous administration, and characterized by flushing and pruritus, known as “red man syndrome” (24). In addition, this drug may lead to more severe reactions including hypotension and muscle spasms (24).
Radiocontrast Media (RCM)
Reactions to RCM with systemic symptoms have decreased with the introduction of non-ionic, low osmolar agents, down from 12.1 to 0.04% of patients receiving RCM (39, 40). Although these reactions have historically been deemed non-IgE mediated, it should be noted that both ionic and non-ionic RCM may trigger IgE-mediated anaphylaxis (35, 41–43). Anaphylaxis to gadolinium agents is much less frequent with an incidence of 0.004–0.01% (44, 45). Older age and multiple previous exposures to RCM increase the risk of having anaphylaxis associated with hypotension. Fatalities have been reported even after the introduction of non-ionic RCM, with most cases lacking predictable risk factors (46). RCM accounted for 27% of fatal drug-induced anaphylaxis (11).
Proton Pump Inhibitors (PPIs)
Anaphylaxis to PPIs is also becoming more common, representing 36–80% of all hypersensitivity reactions to these drugs (47–50). Lansoprazole is the most commonly involved agent (68.3–26.41%), followed by esomeprazole (30.18–10.0%), pantoprazole (20.0%), omeprazole (18.86–1.7%), and rabeprazole (6.7–3.77%) (51).
Neuromuscular Blocking Agents (NMBAs)
Neuromuscular blocking agents are often considered one of the group of drugs that most frequently cause allergic reactions during the perioperative period (52–54). Reactions may be IgE mediated or due to the non-specific release of histamine (52). There are geographical differences and changes over time in the epidemiology of perioperative anaphylaxis. The incidence of intraoperative anaphylactic reactions has been estimated to be 1 in 1,250–10,000 anesthetics in France (54, 55), being lower in Australia and New Zealand (1 in 10,000–20,000) (56). Although mortality from perioperative anaphylaxis has been previously reported between 3 and 9% (54), a more recent study put it in the range of 0–1.4% (56). A study from France reported that for 59% of intraoperative anaphylactic reactions, the etiological agent was an NMBA, more specifically suxamethonium, vecuronium, pancuronium, alcuronium, atracurium, or gallamine (57). More recent studies report rocuronium and succinylcholine at higher risk of anaphylaxis, whereas pancuronium and cis-atracurium are reported to be the NMBAs associated with the lowest incidence of anaphylaxis (53, 58–62).
Sugammadex
Sugammadex is a synthetic g-dextrin derivative designed to selectively bind to steroidal NMBAs. Cases of anaphylaxis to sugammadex have been recently reported (63–65) being an IgE-mediated mechanism suggested in several cases as patients gave positive skin tests and flow cytometry results (66, 67). It has been suggested that treatment of rocuronium-induced anaphylaxis should include the administration of sugammadex (68, 69). However, other studies have concluded that sugammadex is unlikely to modify the clinical course of an established allergic reaction (70).
Hypnotics
Barbiturates induce frequent reactions due to the ability to elicit direct histamine release, although IgE-mediated anaphylaxis has also been described (71, 72). Reactions were also frequent with hypnotics using Cremophor EL as solubilizer; however, since propofol was formulated in soybean oil emulsion, the rate of reactions decreased (54, 73, 74). It has been suggested that allergic patients to eggs or soy should avoid propofol because of the presence of lecithins in the propofol vehicle; however, this has not been confirmed (75, 76) and currently is not recommended (77).
Opioids
Hypersensitivity reactions to opioids are rare, and most cases are due to the non-immunologic induction of histamine release, being pruritus the most frequent symptom. Although rare, isolated episodes of IgE-mediated anaphylaxis to opioids have been described (78–80). The most common offenders inducing non-imnunologic reactions are the low-potency opiates (meperidine, codeine, and morphine); interestingly, high-potency opioids such as fentanyl and hydromorphone are less likely to cause histamine release (81).
Chlorhexidine
Chlorhexidine is a skin antiseptic widely used in surgical settings. Perioperative anaphylaxis induced by chlorhexidine is quite frequent in UK or Denmark (82, 83) but rare in France maybe due to its limited use (84). Sensitization to chlorhexidine can occur from home products such as mouthwash, toothpaste, dressings, ointments, and over the counter disinfectant solutions (85).
Dyes
Triarylmethane dyes, methylene blue, patent blue V, and isosulfan blue induce a relatively frequent rate of perioperative anaphylaxis due to their wide use in sentinel lymph node mapping in cancer surgery. Reactions may be induced by direct mast cell and/or basophil activation and specific IgE (sIgE) sensitization (86–88).
Colloids
The incidence of anaphylaxis to colloids has been estimated to range from 0.033 to 0.22% (89). Gelatins and dextrans are more commonly associated with reactions than albumin and hetastarch (90).
Factors Increasing the Risk of Drug-Induced Anaphylaxis
Clinical Factors
Older age and intravenous administration have been shown to be associated with higher rates of drug-induced anaphylaxis (11) and an increased risk of severe reaction (91, 92). Other factors associated with the prevalence of fatal drug-induced anaphylaxis include race, with African-Americans being shown to have higher prevalence (11), the interruption of prior therapy creating gaps in administration (93) and decreased platelet-activating factor (PAF) acetylhydrolase activity (92). The role of atopy in predisposing an individual to drug-induced anaphylaxis is controversial (94) and underlying mast cell disease has not been described as a predisposing factor (95). Further research is needed to better identify patients at risk and to design preventive strategies to reduce the frequency of drug-induced anaphylaxis.
Cofactors
The presence of several cofactors can increase the risk of suffering anaphylaxis and are reported to be relevant in up to 30% of anaphylaxis episodes (96). They include treatment with drugs such as NSAIDs, PPIs, or angiotensin-converting enzyme inhibitors; the presence of concomitant diseases (asthma, mastocytosis, and cardiovascular diseases); and other factors such as alcohol, emotional stress, or menstruation (96, 97).
Anaphylaxis Mechanisms
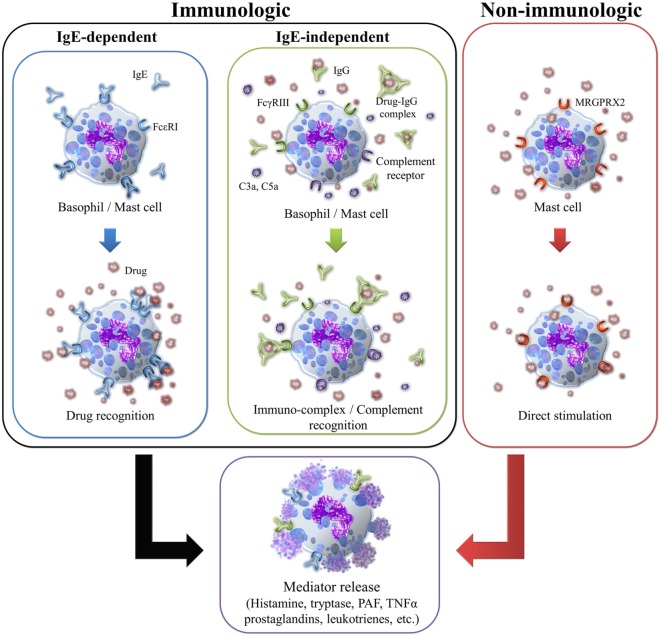
Anaphylaxis can be classified as immunologic and non-immunologic depending on the underlying mechanism; either type of reaction can be induced by drugs (98, 99). In some cases, the trigger cannot be identified; such reactions are classified as idiopathic anaphylaxis (100). Different mechanisms and pathways may be involved as illustrated in Figure 1. Immunologic anaphylaxis can be mediated by an IgE-dependent or -independent mechanism (101), whereas non-immunologic anaphylaxis involves direct mast cell activation (102–104). Independent of the underlying mechanism, allergic symptoms are similar and caused by the release of mediators such as histamine, tryptase, PAF, cysteinyl leukotrienes, and others (1). Histamine is responsible for flushing, pruritus, rhinorrhea, tachycardia, and bronchospasm via the induction of smooth muscle constriction and the increase of vascular permeability. Tryptase activates several pathways, including the complement cascade, coagulation pathway, and the kallikrein–kinin system, contributing to the development of hypotension and angioedema. PAF and cysteinyl leukotrienes also enhance vascular permeability and the development of hypotension (101).
Figure 1.
Different mechanisms of mast cell or basophil activation induced by drugs.
Immunologic Anaphylaxis
This can be induced by IgE-dependent or -independent mechanisms and mediated by the production of antibodies or the activation of the complement pathway (97).
The IgE-dependent mechanism or classical pathway involves a sensitization process including the activation of Th2 cells by the drug, inducing sIgE. This IgE binds to the FcεRI receptor on mast cells, basophils, or both. The cross-linking of two or more of these receptors by the hapten upon subsequent contact, initiates a complex intracellular signaling cascade that leads to degranulation and the release of preformed mediators such as histamine and tryptase. These cause the allergic symptoms and activate other inflammatory cells that can in turn release additional mediators and stimulate the production of others such as prostaglandin D2 and cysteinyl leukotrienes, which serve to amplify the allergic reaction. Two main mechanisms of degranulation have been recently proposed that may be related to reaction severity: piecemeal and anaphylactic degranulation (105). The former is associated with the upregulation of CD203c on basophils (106) by the formation of small vesicles from the histamine-containing granules, which are rapidly shuttled to the plasma membrane (107, 108). This process may be linked to stimulation by certain drugs and the development of more severe reactions like anaphylactic shock (105, 109). In the second mechanism, the main histamine-containing granules are fused to the plasma membrane, releasing the entire contents to the extracellular space and exposing CD63 on the surface of basophils (106). This second process is slower than piecemeal degranulation and could be related to the development of anaphylaxis (110). Penicillins and NMBA are considered the main triggers of IgE-mediated anaphylaxis induced by drugs (54, 111, 112).
The IgE-independent mechanisms can be mediated by IgG antibodies or by complement (97, 113). IgG-mediated anaphylaxis has been demonstrated in mouse models and involves the release of PAF by basophils, macrophages, or neutrophils after the interaction of the drug with specific IgG (sIgG) bound to FcγRIII. Although this mechanism has not been fully established in humans, some studies have shown that PAF is an essential mediator in anaphylaxis (92, 114). Biological agents have been shown to induce anaphylaxis without the presence of detectable sIgE but with high levels of sIgG, as occurs with patients transfused with IgA (115, 116), treated with infliximab or adalimimab (117, 118), and other biological factors (119–121). Complement activation can be induced through the presence of IgG immunocomplex, but also with drugs solubilized in therapeutic liposomes and lipid-based excipients under physiological conditions. This mechanism leads to the release of C3a, C5a, and C5b-9, which trigger activation of mast cells, basophils, and other cells via their specific receptors, causing degranulation and mediator release (97).
IgE-independent mechanism is clinically indistinguishable from IgE-mediated anaphylaxis. Among the most common causes of IgE-independent anaphylaxis are RCM, dextran, and some NSAIDs (20, 122, 123).
Non-Immunologic Anaphylaxis
This type of anaphylaxis does not involve the activation of the immune system, rather the direct stimulation of mast cell degranulation, as has been shown for some drugs (104). This process can be mediated through the MAS-related G protein-coupled receptor-X2 (MRGPRX2) (102–104). The interaction of certain drugs with this mast cell receptor can induce the release of histamine, β-hexosaminidase, TNFα, and PGD2 among others, potentially leading to non-allergic anaphylactic reactions. Medications such as quinolones, opioids, vancomycin, RCM, dextrans, and NMBA have been found to directly stimulate mast cells (104, 124). Whether certain factors may predispose individuals to this type of anaphylaxis needs further research.
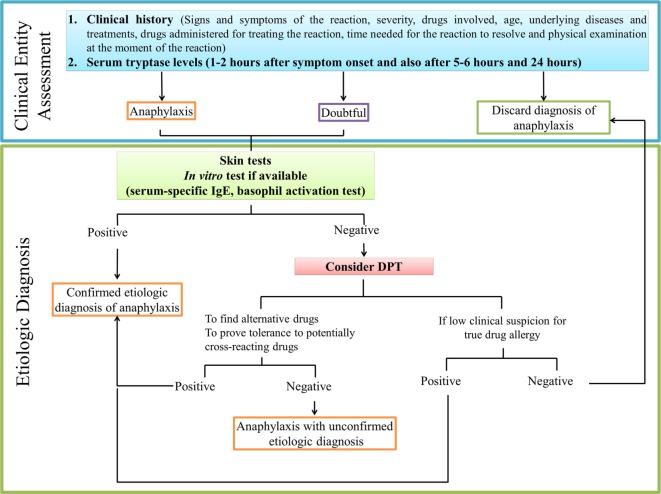
Diagnosis of Anaphylaxis and Identification of the Culprit Drug
The diagnosis of anaphylaxis is based on a thorough examination of patient history and physical evaluation (125). It is important to evaluate various aspects: clinical signs and symptoms of the reaction, grade of severity, drugs administered for treating the reaction, the time needed for the reaction to resolve, age, underlying diseases, and ongoing treatments, such as beta-blockers and angiotensin-converting enzyme inhibitors, and all possible drugs involved in the episode. An accurate identification of the responsible agent is crucial for avoiding anaphylaxis in future treatments (126). The temporal relation of anaphylaxis after the intake of the drug should be ascertained, as most reactions occur within minutes to hours after exposure. However, different drugs are often taken simultaneously, so clinical history is often inconclusive, in which case the work-up of a suspected drug-induced anaphylaxis should also include skin tests, when available and well validated, and in some cases, although not recommended, drug provocation tests (DPTs) (126). In vitro tests can complement the diagnosis confirming clinical suspicions of a severe systemic reaction and avoiding the need to conduct DPTs, potentially saving the patient from suffering another reaction. Moreover, they may help to identify the culprit drug and the underlying mechanism (127). We provide a flowchart for diagnosing drug-induced anaphylaxis in Figure 2.
Figure 2.
Recommended practice flowchart for allergy diagnostic work-up in drug-induced anaphylaxis.
In Vivo Diagnosis
To assess IgE-mediated anaphylaxis, skin testing including skin prick tests (SPT) and intradermal testing (IDT) should be performed. For drug-induced anaphylaxis, SPT are typically performed with the undiluted drug. If negative, IDT is performed sequentially with increasing concentrations of the drug, due to the potential risk of inducing systemic symptoms (128). A positive skin test response is defined by the size of the wheal, which should be 3 mm or greater than that of the negative control (129). Testing should be performed as soon as possible to avoid loss of test sensitivity over time reported for IgE-mediated reactions to drugs (130, 131); although it should not be performed less than 6 weeks after the episode, to avoid any possible refractory period in which testing may give a false negative (24) The rate of negativization depends on the drug, ranging from 60% after 6 months for dipyrone (131) to 47% within 4 years for NBMAs (132).
For most drugs, a negative skin test does not rule out allergy. Therefore, DPT is generally accepted as the gold standard; however, it is not recommended in anaphylaxis due to the high risk of inducing another reaction. It is primarily indicated for patients where clinical suspicion is low, and for patients where it is essential that alternatives to an implicated drug are found (24). It can also be recommended for assessing tolerance to potentially cross-reactive drugs (24). It must be performed under expert supervision, where resuscitation facilities are available and early signs of disorders arising from DPT can be detected (133). Although the traditional drug challenge consists of stepwise graduations, one-step and two-step test dose strategies have been suggested recently (134). Nevertheless, since crucial cofactors might be absent during the procedure, its sensitivity may be not optimal.
In Vitro Diagnosis
Mast cell mediator release can be analyzed immediately after symptom onset and can be considered useful for diagnosis. Tryptase is among the early mediators released by mast cells during an acute allergic reaction, often showing elevated serum levels (>11.5 ng/mL) in anaphylaxis. The measure of total serum tryptase is the most widely used laboratory test to confirm anaphylaxis. As its levels peak 1–2 h after symptom onset and normalize after 5–6 h (101), the optimal timing for drawing a tryptase concentration is 1–2 h after the event (24). However, a normal tryptase level does not rule out anaphylaxis, and values obtained at the time of the event should always be compared with a recent baseline serum tryptase (135, 136). Indeed, a relative increase greater than 135% of the baseline value (even below 11.4 ng/mL) has been suggested to improve diagnosis (137).
Histamine is the first mediator released by mast cells; any elevation in plasma or urine is consistent with anaphylaxis. However, normal levels do not exclude diagnosis and, like tryptase, the acute level must be compared with baseline (127). However, plasma histamine has short half-life (20 min), which limits the utility of this measurement in the clinical setting (101, 138). An indirect method for the determination of histamine consists of measurement of its metabolites, N-methylhistamine or N-methylimidazoleacetic acid, in urine. These appear within 30–60 min of the event and stay detectable for a 24-h period (98, 139, 140).
In addition, levels of chymase, mast cell carboxypeptidase A3, PFA, and other mast cell products may prove to be useful as biomarkers for anaphylaxis (141).
When immunologic mechanisms are involved in the reaction, additional laboratory assays, such as serum-sIgE quantification or the basophil activation test, can be useful to confirm the culprit drug. Immunoassays for drug-sIgE determination using ImmunoCAP are available for a handful of drugs, including five beta-lactams, NMBAs, chlorhexidine, and a few other biological agents (127). Although immunoCAP is the most widely used method, custom-made radioimmunoassays can also be used for a wider variety of drugs including quinolones and other beta-lactams (127). The basophil activation test, which can be performed with any suspected drug, measures the activation of basophils after stimulation and is suitable for both IgE-mediated and non-IgE-mediated hypersensitivity (24).
Management
Adrenaline is the first-line treatment for anaphylaxis and should be administered as soon as possible by intramuscular injection into the middle of the outer thigh (142). The patient may require the repeated administration of adrenaline at 5-min intervals if improvement is not observed or symptoms reoccur. Following adrenaline treatment, the trigger should be removed if possible, for example, stopping i.v. medication. The administration of other drugs such as corticosteroids and beta-2 agonists may reduce other features of anaphylaxis and the risk of biphasic and protracted reactions (143, 144). Parenteral administration of glucagon may be useful for treating patients who are unresponsive to adrenaline, particularly in those taking beta-blockers (145).
Conclusion
Drug-induced anaphylaxis is a potentially life-threatening reaction that appears to be increasing in both prevalence and incidence, likely due in part to the introduction of new medications. An accurate and prompt diagnosis is necessary to a correct management of this acute reaction, and the identification of the culprit drug is crucial to avoid new future reactions. Further research about mechanisms and risk factors is needed to try to prevent the development of this reaction and to orient therapeutic approaches to patient, based on the culprit drug and the clinical reactions, which should target the underlying specific mechanisms.
Author Contributions
All authors have made substantial intellectual contributions to the preparation of the manuscript and approved it for publication.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
We would like to thank James R. Perkins for his help in language editing.
Footnotes
Funding. The present study has been supported by Institute of Health “Carlos III” of the Ministry of Economy and Competitiveness (grants cofunded by European Regional Development Fund (ERDF): PI12/02529, PI15/01206, CP15/00103, RETICs RIRAAF RD12/0013/0001, RETIC ARADYAL RD16/0006/0001, and RD16/0006/0033); Andalusian Regional Ministry of Economy and Knowledge (grants cofunded by European Regional Development Fund (ERDF): CTS-06603); Andalusian Regional Ministry Health (grants: PI-0699-2011, PI-0179-2014, and PI-0241-2016); Premio UNICAJA a la innovación en biomedicina y salud; and Merck-Serono Research Grant from Fundación Salud 2000. MM holds a “Miguel Servet I” research contract (CP15/00103), GB holds a Rio Hortega contract (CM16/00057) and ID holds a Juan Rodes contract (JR15/00036), all funded by Institute of Health “Carlos III” of the Ministry of Economy and Competitiveness [grants cofunded by European Social Fund (ESF)]. CM holds a “Nicolas Monardes” research contract by Andalusian Regional Ministry Health: C-0044-2012 SAS 2013. TF holds a “Ramon y Cajal” research contract from Ministry of Economy and Competitiveness (RYC-2013-13138).
References
- 1.Simons FE. 9. Anaphylaxis. J Allergy Clin Immunol (2008) 121(2 Suppl):S402–7; quiz S20. 10.1016/j.jaci.2007.08.061 [DOI] [PubMed] [Google Scholar]
- 2.Johansson SG, Bieber T, Dahl R, Friedmann PS, Lanier BQ, Lockey RF, et al. Revised nomenclature for allergy for global use: report of the nomenclature review committee of the World Allergy Organization, October 2003. J Allergy Clin Immunol (2004) 113(5):832–6. 10.1016/j.jaci.2003.12.591 [DOI] [PubMed] [Google Scholar]
- 3.Sampson HA, Munoz-Furlong A, Campbell RL, Adkinson NF, Jr, Bock SA, Branum A, et al. Second symposium on the definition and management of anaphylaxis: summary report – second national institute of allergy and infectious disease/food allergy and anaphylaxis network symposium. J Allergy Clin Immunol (2006) 117(2):391–7. 10.1016/j.jaci.2005.12.1303 [DOI] [PubMed] [Google Scholar]
- 4.Liew WK, Williamson E, Tang ML. Anaphylaxis fatalities and admissions in Australia. J Allergy Clin Immunol (2009) 123(2):434–42. 10.1016/j.jaci.2008.10.049 [DOI] [PubMed] [Google Scholar]
- 5.Gonzalez-Perez A, Aponte Z, Vidaurre CF, Rodriguez LA. Anaphylaxis epidemiology in patients with and patients without asthma: a United Kingdom database review. J Allergy Clin Immunol (2010) 125(5):1098–104.e1. 10.1016/j.jaci.2010.02.009 [DOI] [PubMed] [Google Scholar]
- 6.Wood RA, Camargo CA, Jr, Lieberman P, Sampson HA, Schwartz LB, Zitt M, et al. Anaphylaxis in America: the prevalence and characteristics of anaphylaxis in the United States. J Allergy Clin Immunol (2014) 133(2):461–7. 10.1016/j.jaci.2013.08.016 [DOI] [PubMed] [Google Scholar]
- 7.Huang F, Chawla K, Jarvinen KM, Nowak-Wegrzyn A. Anaphylaxis in a New York City pediatric emergency department: triggers, treatments, and outcomes. J Allergy Clin Immunol (2012) 129(1):162–8.e1–3. 10.1016/j.jaci.2011.09.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Techapornroong M, Akrawinthawong K, Cheungpasitporn W, Ruxrungtham K. Anaphylaxis: a ten years inpatient retrospective study. Asian Pac J Allergy Immunol (2010) 28(4):262–9. [PubMed] [Google Scholar]
- 9.Beyer K, Eckermann O, Hompes S, Grabenhenrich L, Worm M. Anaphylaxis in an emergency setting – elicitors, therapy and incidence of severe allergic reactions. Allergy (2012) 67(11):1451–6. 10.1111/all.12012 [DOI] [PubMed] [Google Scholar]
- 10.Aun MV, Blanca M, Garro LS, Ribeiro MR, Kalil J, Motta AA, et al. Nonsteroidal anti-inflammatory drugs are major causes of drug-induced anaphylaxis. J Allergy Clin Immunol Pract (2014) 2(4):414–20. 10.1016/j.jaip.2014.03.014 [DOI] [PubMed] [Google Scholar]
- 11.Jerschow E, Lin RY, Scaperotti MM, McGinn AP. Fatal anaphylaxis in the United States, 1999–2010: temporal patterns and demographic associations. J Allergy Clin Immunol (2014) 134(6):1318–28.e7. 10.1016/j.jaci.2014.08.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lee S, Bellolio MF, Hess EP, Campbell RL. Predictors of biphasic reactions in the emergency department for patients with anaphylaxis. J Allergy Clin Immunol Pract (2014) 2(3):281–7. 10.1016/j.jaip.2014.01.012 [DOI] [PubMed] [Google Scholar]
- 13.Amornmarn LBL, Kumar N. Anaphylaxis admissions to a university hospital. J Allergy Clin Immunol (1992) 89:349. [Google Scholar]
- 14.Klein JS, Yocum MW. Underreporting of anaphylaxis in a community emergency room. J Allergy Clin Immunol (1995) 95(2):637–8. 10.1016/S0091-6749(95)70329-2 [DOI] [PubMed] [Google Scholar]
- 15.International Collaborative Study of Severe Anaphylaxis. Risk of anaphylaxis in a hospital population in relation to the use of various drugs: an international study. Pharmacoepidemiol Drug Saf (2003) 12:195–202. 10.1002/pds.822 [DOI] [PubMed] [Google Scholar]
- 16.Moro Moro M, Tejedor Alonso MA, Esteban Hernandez J, Mugica Garcia MV, Rosado Ingelmo A, Vila Albelda C. Incidence of anaphylaxis and subtypes of anaphylaxis in a general hospital emergency department. J Investig Allergol Clin Immunol (2011) 21(2):142–9. [PubMed] [Google Scholar]
- 17.Yocum MW, Butterfield JH, Klein JS, Volcheck GW, Schroeder DR, Silverstein MD. Epidemiology of anaphylaxis in Olmsted County: a population-based study. J Allergy Clin Immunol (1999) 104(2 Pt 1):452–6. 10.1016/S0091-6749(99)70392-1 [DOI] [PubMed] [Google Scholar]
- 18.Jares EJ, Baena-Cagnani CE, Sanchez-Borges M, Ensina LF, Arias-Cruz A, Gomez M, et al. Drug-induced anaphylaxis in Latin American countries. J Allergy Clin Immunol Pract (2015) 3(5):780–8. 10.1016/j.jaip.2015.05.012 [DOI] [PubMed] [Google Scholar]
- 19.Canto MG, Andreu I, Fernandez J, Blanca M. Selective immediate hypersensitivity reactions to NSAIDs. Curr Opin Allergy Clin Immunol (2009) 9(4):293–7. 10.1097/ACI.0b013e32832db943 [DOI] [PubMed] [Google Scholar]
- 20.Kowalski ML, Asero R, Bavbek S, Blanca M, Blanca-Lopez N, Bochenek G, et al. Classification and practical approach to the diagnosis and management of hypersensitivity to nonsteroidal anti-inflammatory drugs. Allergy (2013) 68(10):1219–32. 10.1111/all.12260 [DOI] [PubMed] [Google Scholar]
- 21.Stevenson DD, Sanchez-Borges M, Szczeklik A. Classification of allergic and pseudoallergic reactions to drugs that inhibit cyclooxygenase enzymes. Ann Allergy Asthma Immunol (2001) 87(3):177–80. 10.1016/S1081-1206(10)62221-1 [DOI] [PubMed] [Google Scholar]
- 22.Dona I, Blanca-Lopez N, Cornejo-Garcia JA, Torres MJ, Laguna JJ, Fernandez J, et al. Characteristics of subjects experiencing hypersensitivity to non-steroidal anti-inflammatory drugs: patterns of response. Clin Exp Allergy (2011) 41(1):86–95. 10.1111/j.1365-2222.2010.03651.x [DOI] [PubMed] [Google Scholar]
- 23.Quiralte J, Blanco C, Castillo R, Delgado J, Carrillo T. Intolerance to nonsteroidal antiinflammatory drugs: results of controlled drug challenges in 98 patients. J Allergy Clin Immunol (1996) 98(3):678–85. 10.1016/S0091-6749(96)70102-1 [DOI] [PubMed] [Google Scholar]
- 24.Kuruvilla M, Khan DA. Anaphylaxis to drugs. Immunol Allergy Clin North Am (2015) 35(2):303–19. 10.1016/j.iac.2015.01.008 [DOI] [PubMed] [Google Scholar]
- 25.Makowska J, Lewandowska-Polak A, Kowalski ML. Hypersensitivity to aspirin and other NSAIDs: diagnostic approach in patients with chronic rhinosinusitis. Curr Allergy Asthma Rep (2015) 15(8):47. 10.1007/s11882-015-0552-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Drain KL, Volcheck GW. Preventing and managing drug-induced anaphylaxis. Drug Saf (2001) 24(11):843–53. 10.2165/00002018-200124110-00005 [DOI] [PubMed] [Google Scholar]
- 27.Kemp SF, Lockey RF, Wolf BL, Lieberman P. Anaphylaxis. A review of 266 cases. Arch Intern Med (1995) 155(16):1749–54. 10.1001/archinte.1995.00430160077008 [DOI] [PubMed] [Google Scholar]
- 28.Torres MJ, Ariza A, Mayorga C, Dona I, Blanca-Lopez N, Rondon C, et al. Clavulanic acid can be the component in amoxicillin-clavulanic acid responsible for immediate hypersensitivity reactions. J Allergy Clin Immunol (2010) 125(2):502–5.e2. 10.1016/j.jaci.2009.11.032 [DOI] [PubMed] [Google Scholar]
- 29.Sanchez-Morillas L, Perez-Ezquerra PR, Reano-Martos M, Laguna-Martinez JJ, Sanz ML, Martinez LM. Selective allergic reactions to clavulanic acid: a report of 9 cases. J Allergy Clin Immunol (2010) 126(1):177–9. 10.1016/j.jaci.2010.03.012 [DOI] [PubMed] [Google Scholar]
- 30.Macy E, Contreras R. Adverse reactions associated with oral and parenteral use of cephalosporins: a retrospective population-based analysis. J Allergy Clin Immunol (2015) 135(3):745–52.e5. 10.1016/j.jaci.2014.07.062 [DOI] [PubMed] [Google Scholar]
- 31.Renaudin JM, Beaudouin E, Ponvert C, Demoly P, Moneret-Vautrin DA. Severe drug-induced anaphylaxis: analysis of 333 cases recorded by the allergy vigilance network from 2002 to 2010. Allergy (2013) 68(7):929–37. 10.1111/all.12168 [DOI] [PubMed] [Google Scholar]
- 32.Iglesias Cadarso A, Saez Jimenez SA, Vidal Pan C, Rodriguez Mosquera M. Aztreonam-induced anaphylaxis. Lancet (1990) 336(8717):746–7. 10.1016/0140-6736(90)92238-D [DOI] [PubMed] [Google Scholar]
- 33.Weiss ME, Adkinson NF. Immediate hypersensitivity reactions to penicillin and related antibiotics. Clin Allergy (1988) 18(6):515–40. 10.1111/j.1365-2222.1988.tb02904.x [DOI] [PubMed] [Google Scholar]
- 34.Neugut AI, Ghatak AT, Miller RL. Anaphylaxis in the United States: an investigation into its epidemiology. Arch Intern Med (2001) 161(1):15–21. 10.1001/archinte.161.1.15 [DOI] [PubMed] [Google Scholar]
- 35.Salas M, Gomez F, Fernandez TD, Dona I, Aranda A, Ariza A, et al. Diagnosis of immediate hypersensitivity reactions to radiocontrast media. Allergy (2013) 68(9):1203–6. 10.1111/all.12214 [DOI] [PubMed] [Google Scholar]
- 36.Bijl AM, Van der Klauw MM, Van Vliet AC, Stricker BH. Anaphylactic reactions associated with trimethoprim. Clin Exp Allergy (1998) 28(4):510–2. 10.1046/j.1365-2222.1998.00258.x [DOI] [PubMed] [Google Scholar]
- 37.Swamy N, Laurie SA, Ruiz-Huidobro E, Khan DA. Successful clarithromycin desensitization in a multiple macrolide-allergic patient. Ann Allergy Asthma Immunol (2010) 105(6):489–90. 10.1016/j.anai.2010.08.018 [DOI] [PubMed] [Google Scholar]
- 38.Knudsen JD, Pedersen M. IgE-mediated reaction to vancomycin and teicoplanin after treatment with vancomycin. Scand J Infect Dis (1992) 24(3):395–6. 10.3109/00365549209061350 [DOI] [PubMed] [Google Scholar]
- 39.Kim MH, Lee SY, Lee SE, Yang MS, Jung JW, Park CM, et al. Anaphylaxis to iodinated contrast media: clinical characteristics related with development of anaphylactic shock. PLoS One (2014) 9(6):e100154. 10.1371/journal.pone.0100154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Katayama H, Yamaguchi K, Kozuka T, Takashima T, Seez P, Matsuura K. Adverse reactions to ionic and nonionic contrast media. A report from the Japanese committee on the safety of contrast media. Radiology (1990) 175(3):621–8. 10.1148/radiology.175.3.2343107 [DOI] [PubMed] [Google Scholar]
- 41.Laroche D, Aimone-Gastin I, Dubois F, Huet H, Gerard P, Vergnaud MC, et al. Mechanisms of severe, immediate reactions to iodinated contrast material. Radiology (1998) 209(1):183–90. 10.1148/radiology.209.1.9769830 [DOI] [PubMed] [Google Scholar]
- 42.Mita H, Tadokoro K, Akiyama K. Detection of IgE antibody to a radiocontrast medium. Allergy (1998) 53(12):1133–40. 10.1111/j.1398-9995.1998.tb03832.x [DOI] [PubMed] [Google Scholar]
- 43.Brockow K, Romano A, Aberer W, Bircher AJ, Barbaud A, Bonadonna P, et al. Skin testing in patients with hypersensitivity reactions to iodinated contrast media – a European multicenter study. Allergy (2009) 64(2):234–41. 10.1111/j.1398-9995.2008.01832.x [DOI] [PubMed] [Google Scholar]
- 44.Li A, Wong CS, Wong MK, Lee CM, Au Yeung MC. Acute adverse reactions to magnetic resonance contrast media – gadolinium chelates. Br J Radiol (2006) 79(941):368–71. 10.1259/bjr/88469693 [DOI] [PubMed] [Google Scholar]
- 45.Jung JW, Kang HR, Kim MH, Lee W, Min KU, Han MH, et al. Immediate hypersensitivity reaction to gadolinium-based MR contrast media. Radiology (2012) 264(2):414–22. 10.1148/radiol.12112025 [DOI] [PubMed] [Google Scholar]
- 46.Palmiere C, Reggiani Bonetti L. Risk factors in fatal cases of anaphylaxis due to contrast media: a forensic evaluation. Int Arch Allergy Immunol (2014) 164(4):280–8. 10.1159/000366204 [DOI] [PubMed] [Google Scholar]
- 47.Dona I, Blanca-Lopez N, Torres MJ, Garcia-Campos J, Garcia-Nunez I, Gomez F, et al. Drug hypersensitivity reactions: response patterns, drug involved, and temporal variations in a large series of patients. J Investig Allergol Clin Immunol (2012) 22(5):363–71. [PubMed] [Google Scholar]
- 48.Kepil Ozdemir S, Oner Erkekol F, Unal D, Buyukozturk S, Gelincik A, Dursun AB, et al. Management of hypersensitivity reactions to proton pump inhibitors: a retrospective experience. Int Arch Allergy Immunol (2016) 171(1):54–60. 10.1159/000450952 [DOI] [PubMed] [Google Scholar]
- 49.Abdul Razzak E, Tomas M, Tornero P, Herrero T. Nine cases of allergy to omeprazole. J Investig Allergol Clin Immunol (2012) 22(3):228–30. [PubMed] [Google Scholar]
- 50.Sobrevia Elfau MT, Garces Sotillos M, Ferrer Claveria L, Segura Arazuri N, Monzon Ballarin S, Colas Sanz C. Study of cross-reactivity between proton pump inhibitors. J Investig Allergol Clin Immunol (2010) 20(2):157–61. [PubMed] [Google Scholar]
- 51.Bonadonna P, Lombardo C, Bortolami O, Bircher A, Scherer K, Barbaud A, et al. Hypersensitivity to proton pump inhibitors: diagnostic accuracy of skin tests compared to oral provocation test. J Allergy Clin Immunol (2012) 130(2):547–9. 10.1016/j.jaci.2012.04.048 [DOI] [PubMed] [Google Scholar]
- 52.Ewan PW, Dugue P, Mirakian R, Dixon TA, Harper JN, Nasser SM, et al. BSACI guidelines for the investigation of suspected anaphylaxis during general anaesthesia. Clin Exp Allergy (2010) 40(1):15–31. 10.1111/j.1365-2222.2009.03404.x [DOI] [PubMed] [Google Scholar]
- 53.Meng J, Rotiroti G, Burdett E, Lukawska JJ. Anaphylaxis during general anaesthesia: experience from a drug allergy centre in the UK. Acta Anaesthesiol Scand (2017) 61(3):281–9. 10.1111/aas.12858 [DOI] [PubMed] [Google Scholar]
- 54.Mertes PM, Alla F, Trechot P, Auroy Y, Jougla E, Groupe d’Etudes des Réactions Anaphylactoïdes Peranesthésiques . Anaphylaxis during anesthesia in France: an 8 year national survey. J Allergy Clin Immunol (2011) 128(2):366–73. 10.1016/j.jaci.2011.03.003 [DOI] [PubMed] [Google Scholar]
- 55.Laxenaire MC. [Epidemiology of anesthetic anaphylactoid reactions. Fourth multicenter survey (July 1994–December 1996)]. Ann Fr Anesth Reanim (1999) 18(7):796–809. 10.1016/S0750-7658(00)88460-9 [DOI] [PubMed] [Google Scholar]
- 56.Gibbs NM, Sadleir PH, Clarke RC, Platt PR. Survival from perioperative anaphylaxis in Western Australia 2000–2009. Br J Anaesth (2013) 111(4):589–93. 10.1093/bja/aet117 [DOI] [PubMed] [Google Scholar]
- 57.Laxenaire MC. [Substances responsible for peranesthetic anaphylactic shock. A third French multicenter study (1992–94)]. Ann Fr Anesth Reanim (1996) 15(8):1211–8. 10.1016/S0750-7658(97)85882-0 [DOI] [PubMed] [Google Scholar]
- 58.Reddy JI, Cooke PJ, van Schalkwyk JM, Hannam JA, Fitzharris P, Mitchell SJ. Anaphylaxis is more common with rocuronium and succinylcholine than with atracurium. Anesthesiology (2015) 122(1):39–45. 10.1097/ALN.0000000000000512 [DOI] [PubMed] [Google Scholar]
- 59.Sadleir PH, Clarke RC, Bunning DL, Platt PR. Anaphylaxis to neuromuscular blocking drugs: incidence and cross-reactivity in Western Australia from 2002 to 2011. Br J Anaesth (2013) 110(6):981–7. 10.1093/bja/aes506 [DOI] [PubMed] [Google Scholar]
- 60.Fisher M, Baldo BA. Anaphylaxis during anaesthesia: current aspects of diagnosis and prevention. Eur J Anaesthesiol (1994) 11(4):263–84. [PubMed] [Google Scholar]
- 61.Mertes PM, Laxenaire MC, Alla F, Groupe d’Etudes des reactions anaphylactoides Peranesthésiques Anaphylactic and anaphylactoid reactions occurring during anesthesia in France in 1999–2000. Anesthesiology (2003) 99(3):536–45. 10.1097/00000542-200309000-00007 [DOI] [PubMed] [Google Scholar]
- 62.Guttormsen AB. Allergic reactions during anaesthesia – increased attention to the problem in Denmark and Norway. Acta Anaesthesiol Scand (2001) 45(10):1189–90. 10.1034/j.1399-6576.2001.451001.x [DOI] [PubMed] [Google Scholar]
- 63.Baldo BA. Sugammadex and hypersensitivity. Anaesth Intensive Care (2014) 42(4):525–7. [PubMed] [Google Scholar]
- 64.Tsur A, Kalansky A. Hypersensitivity associated with sugammadex administration: a systematic review. Anaesthesia (2014) 69(11):1251–7. 10.1111/anae.12736 [DOI] [PubMed] [Google Scholar]
- 65.Takazawa T, Tomita Y, Yoshida N, Tomioka A, Horiuchi T, Nagata C, et al. Three suspected cases of sugammadex-induced anaphylactic shock. BMC Anesthesiol (2014) 14:92. 10.1186/1471-2253-14-92 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Sadleir PH, Russell T, Clarke RC, Maycock E, Platt PR. Intraoperative anaphylaxis to sugammadex and a protocol for intradermal skin testing. Anaesth Intensive Care (2014) 42(1):93–6. [DOI] [PubMed] [Google Scholar]
- 67.Takazawa T, Horiuchi T, Yoshida N, Yokohama A, Saito S. Flow cytometric investigation of sugammadex-induced anaphylaxis. Br J Anaesth (2015) 114(5):858–9. 10.1093/bja/aev093 [DOI] [PubMed] [Google Scholar]
- 68.Baldo B. Sugammadex and rocuronium-induced anaphylaxis. Anaesthesia (2012) 67(10):1174–5; author reply 5. 10.1111/j.1365-2044.2012.07289.x [DOI] [PubMed] [Google Scholar]
- 69.Leysen J, Bridts CH, De Clerck LS, Ebo DG. Rocuronium-induced anaphylaxis is probably not mitigated by sugammadex: evidence from an in vitro experiment. Anaesthesia (2011) 66(6):526–7. 10.1111/j.1365-2044.2011.06729.x [DOI] [PubMed] [Google Scholar]
- 70.Clarke RC, Sadleir PH, Platt PR. The role of sugammadex in the development and modification of an allergic response to rocuronium: evidence from a cutaneous model. Anaesthesia (2012) 67(3):266–73. 10.1111/j.1365-2044.2011.06995.x [DOI] [PubMed] [Google Scholar]
- 71.Baldo BA, Fisher MM, Harle DG. Allergy to thiopentone. Clin Rev Allergy (1991) 9(3–4):295–308. 10.1007/BF02802309 [DOI] [PubMed] [Google Scholar]
- 72.Moscicki RA, Sockin SM, Corsello BF, Ostro MG, Bloch KJ. Anaphylaxis during induction of general anesthesia: subsequent evaluation and management. J Allergy Clin Immunol (1990) 86(3 Pt 1):325–32. 10.1016/S0091-6749(05)80095-8 [DOI] [PubMed] [Google Scholar]
- 73.Dong SW, Mertes PM, Petitpain N, Hasdenteufel F, Malinovsky JM. Hypersensitivity reactions during anesthesia. Results from the ninth French survey (2005–2007). Minerva Anestesiol (2012) 78(8):868–78. [PubMed] [Google Scholar]
- 74.Baker MT, Naguib M. Propofol: the challenges of formulation. Anesthesiology (2005) 103(4):860–76. 10.1097/00000542-200510000-00026 [DOI] [PubMed] [Google Scholar]
- 75.Murphy A, Campbell DE, Baines D, Mehr S. Allergic reactions to propofol in egg-allergic children. Anesth Analg (2011) 113(1):140–4. 10.1213/ANE.0b013e31821b450f [DOI] [PubMed] [Google Scholar]
- 76.Asserhoj LL, Mosbech H, Kroigaard M, Garvey LH. No evidence for contraindications to the use of propofol in adults allergic to egg, soy or peanut†. Br J Anaesth (2016) 116(1):77–82. 10.1093/bja/aev360 [DOI] [PubMed] [Google Scholar]
- 77.Mertes PM, Malinovsky JM, Jouffroy L, Working Group of the SFAR and SFA. Aberer W, Terreehorst I, et al. Reducing the risk of anaphylaxis during anesthesia: 2011 updated guidelines for clinical practice. J Investig Allergol Clin Immunol (2011) 21(6):442–53. [PubMed] [Google Scholar]
- 78.Dewachter P, Lefebvre D, Kalaboka S, Bloch-Morot E. An anaphylactic reaction to transdermal delivered fentanyl. Acta Anaesthesiol Scand (2009) 53(8):1092–3. 10.1111/j.1399-6576.2009.02022.x [DOI] [PubMed] [Google Scholar]
- 79.Anibarro B, Vila C, Seoane FJ. Urticaria induced by meperidine allergy. Allergy (2000) 55(3):305–6. 10.1034/j.1398-9995.2000.00542.x [DOI] [PubMed] [Google Scholar]
- 80.Harle DG, Baldo BA, Coroneos NJ, Fisher MM. Anaphylaxis following administration of papaveretum. Case report: implication of IgE antibodies that react with morphine and codeine, and identification of an allergenic determinant. Anesthesiology (1989) 71(4):489–94. 10.1097/00000542-198910000-00003 [DOI] [PubMed] [Google Scholar]
- 81.Baldo BA, Pham NH. Histamine-releasing and allergenic properties of opioid analgesic drugs: resolving the two. Anaesth Intensive Care (2012) 40(2):216–35. [DOI] [PubMed] [Google Scholar]
- 82.Garvey LH, Kroigaard M, Poulsen LK, Skov PS, Mosbech H, Venemalm L, et al. IgE-mediated allergy to chlorhexidine. J Allergy Clin Immunol (2007) 120(2):409–15. 10.1016/j.jaci.2007.04.029 [DOI] [PubMed] [Google Scholar]
- 83.Krishna MT, York M, Chin T, Gnanakumaran G, Heslegrave J, Derbridge C, et al. Multi-centre retrospective analysis of anaphylaxis during general anaesthesia in the United Kingdom: aetiology and diagnostic performance of acute serum tryptase. Clin Exp Immunol (2014) 178(2):399–404. 10.1111/cei.12424 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Dong S, Acouetey DS, Gueant-Rodriguez RM, Zmirou-Navier D, Remen T, Blanca M, et al. Prevalence of IgE against neuromuscular blocking agents in hairdressers and bakers. Clin Exp Allergy (2013) 43(11):1256–62. 10.1111/cea.12189 [DOI] [PubMed] [Google Scholar]
- 85.Opstrup MS, Johansen JD, Garvey LH. Chlorhexidine allergy: sources of exposure in the health-care setting. Br J Anaesth (2015) 114(4):704–5. 10.1093/bja/aev050 [DOI] [PubMed] [Google Scholar]
- 86.Giladi AM, Kasten SJ. Anaphylactic-like reaction to methylene blue: case report and review of perioperative hypersensitivity reactions. Plast Reconstr Surg (2012) 130(1):98e–105e. 10.1097/PRS.0b013e318254b2b8 [DOI] [PubMed] [Google Scholar]
- 87.Mertes PM, Demoly P, Alperovitch A, Bazin A, Bienvenu J, Caldani C, et al. Methylene blue-treated plasma: an increased allergy risk? J Allergy Clin Immunol (2012) 130(3):808–12. 10.1016/j.jaci.2012.03.050 [DOI] [PubMed] [Google Scholar]
- 88.Mertes PM, Malinovsky JM, Mouton-Faivre C, Bonnet-Boyer MC, Benhaijoub A, Lavaud F, et al. Anaphylaxis to dyes during the perioperative period: reports of 14 clinical cases. J Allergy Clin Immunol (2008) 122(2):348–52. 10.1016/j.jaci.2008.04.040 [DOI] [PubMed] [Google Scholar]
- 89.Laxenaire MC, Charpentier C, Feldman L. [Anaphylactoid reactions to colloid plasma substitutes: incidence, risk factors, mechanisms. A French multicenter prospective study]. Ann Fr Anesth Reanim (1994) 13(3):301–10. 10.1016/S0750-7658(94)80038-3 [DOI] [PubMed] [Google Scholar]
- 90.Volcheck GW, Mertes PM. Local and general anesthetics immediate hypersensitivity reactions. Immunol Allergy Clin North Am (2014) 34(3):525–46, viii. 10.1016/j.iac.2014.03.004 [DOI] [PubMed] [Google Scholar]
- 91.Clark S, Wei W, Rudders SA, Camargo CA, Jr. Risk factors for severe anaphylaxis in patients receiving anaphylaxis treatment in US emergency departments and hospitals. J Allergy Clin Immunol (2014) 134(5):1125–30. 10.1016/j.jaci.2014.05.018 [DOI] [PubMed] [Google Scholar]
- 92.Brown SG, Stone SF, Fatovich DM, Burrows SA, Holdgate A, Celenza A, et al. Anaphylaxis: clinical patterns, mediator release, and severity. J Allergy Clin Immunol (2013) 132(5):1141.e–9.e. 10.1016/j.jaci.2013.06.015 [DOI] [PubMed] [Google Scholar]
- 93.Lieberman P. Difficult allergic drug reactions. Immunol Allergy Clin North Am (1991) 11(1):331. [Google Scholar]
- 94.Idsoe O, Guthe T, Willcox RR, de Weck AL. Nature and extent of penicillin side-reactions, with particular reference to fatalities from anaphylactic shock. Bull World Health Organ (1968) 38(2):159–88. [PMC free article] [PubMed] [Google Scholar]
- 95.Brockow K, Bonadonna P. Drug allergy in mast cell disease. Curr Opin Allergy Clin Immunol (2012) 12(4):354–60. 10.1097/ACI.0b013e328355b7cb [DOI] [PubMed] [Google Scholar]
- 96.Wolbing F, Fischer J, Koberle M, Kaesler S, Biedermann T. About the role and underlying mechanisms of cofactors in anaphylaxis. Allergy (2013) 68(9):1085–92. 10.1111/all.12193 [DOI] [PubMed] [Google Scholar]
- 97.Munoz-Cano R, Picado C, Valero A, Bartra J. Mechanisms of anaphylaxis beyond IgE. J Investig Allergol Clin Immunol (2016) 26(2):73–82; quiz 2p following 3. 10.18176/jiaci.0046 [DOI] [PubMed] [Google Scholar]
- 98.Greenberger PA, Ditto AM. Chapter 24: anaphylaxis. Allergy Asthma Proc (2012) 33(Suppl 1):S80–3. 10.2500/aap.2012.33.3557 [DOI] [PubMed] [Google Scholar]
- 99.Simons FE. Anaphylaxis. J Allergy Clin Immunol (2010) 125(2 Suppl 2):S161–81. 10.1016/j.jaci.2009.12.981 [DOI] [PubMed] [Google Scholar]
- 100.Fenny N, Grammer LC. Idiopathic anaphylaxis. Immunol Allergy Clin North Am (2015) 35(2):349–62. 10.1016/j.iac.2015.01.004 [DOI] [PubMed] [Google Scholar]
- 101.Williams KW, Sharma HP. Anaphylaxis and urticaria. Immunol Allergy Clin North Am (2015) 35(1):199–219. 10.1016/j.iac.2014.09.010 [DOI] [PubMed] [Google Scholar]
- 102.Lieberman P, Garvey LH. Mast cells and anaphylaxis. Curr Allergy Asthma Rep (2016) 16(3):20. 10.1007/s11882-016-0598-5 [DOI] [PubMed] [Google Scholar]
- 103.McNeil BD, Pundir P, Meeker S, Han L, Undem BJ, Kulka M, et al. Identification of a mast-cell-specific receptor crucial for pseudo-allergic drug reactions. Nature (2015) 519(7542):237–41. 10.1038/nature14022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Subramanian H, Gupta K, Ali H. Roles of Mas-related G protein-coupled receptor X2 on mast cell-mediated host defense, pseudoallergic drug reactions, and chronic inflammatory diseases. J Allergy Clin Immunol (2016) 138(3):700–10. 10.1016/j.jaci.2016.04.051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Fernandez TD, Ariza A, Palomares F, Montanez MI, Salas M, Martin-Serrano A, et al. Hypersensitivity to fluoroquinolones: the expression of basophil activation markers depends on the clinical entity and the culprit fluoroquinolone. Medicine (Baltimore) (2016) 95(23):e3679. 10.1097/MD.0000000000003679 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.MacGlashan DW, Jr. Basophil activation testing. J Allergy Clin Immunol (2013) 132(4):777–87. 10.1016/j.jaci.2013.06.038 [DOI] [PubMed] [Google Scholar]
- 107.MacGlashan D, Jr. Expression of CD203c and CD63 in human basophils: relationship to differential regulation of piecemeal and anaphylactic degranulation processes. Clin Exp Allergy (2010) 40(9):1365–77. 10.1111/j.1365-2222.2010.03572.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.MacGlashan D, Jr. Marked differences in the signaling requirements for expression of CD203c and CD11b versus CD63 expression and histamine release in human basophils. Int Arch Allergy Immunol (2012) 159(3):243–52. 10.1159/000332150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Ben Said B, Berard F, Bienvenu J, Nicolas JF, Rozieres A. Usefulness of basophil activation tests for the diagnosis of IgE-mediated allergy to quinolones. Allergy (2010) 65(4):535–6. 10.1111/j.1398-9995.2009.02213.x [DOI] [PubMed] [Google Scholar]
- 110.Aranda A, Mayorga C, Ariza A, Dona I, Rosado A, Blanca-Lopez N, et al. In vitro evaluation of IgE-mediated hypersensitivity reactions to quinolones. Allergy (2011) 66(2):247–54. 10.1111/j.1398-9995.2010.02460.x [DOI] [PubMed] [Google Scholar]
- 111.Torres MJ, Blanca M. The complex clinical picture of beta-lactam hypersensitivity: penicillins, cephalosporins, monobactams, carbapenems, and clavams. Med Clin North Am (2010) 94(4):805–20, xii. 10.1016/j.mcna.2010.04.006 [DOI] [PubMed] [Google Scholar]
- 112.Antunez C, Fernandez T, Blanca-Lopez N, Torres MJ, Mayorga C, Canto G, et al. IgE antibodies to betalactams: relationship between the triggering hapten and the specificity of the immune response. Allergy (2006) 61(8):940–6. 10.1111/j.1398-9995.2006.01120.x [DOI] [PubMed] [Google Scholar]
- 113.Finkelman FD, Khodoun MV, Strait R. Human IgE-independent systemic anaphylaxis. J Allergy Clin Immunol (2016) 137(6):1674–80. 10.1016/j.jaci.2016.02.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Vadas P, Gold M, Perelman B, Liss GM, Lack G, Blyth T, et al. Platelet-activating factor, PAF acetylhydrolase, and severe anaphylaxis. N Engl J Med (2008) 358(1):28–35. 10.1056/NEJMoa070030 [DOI] [PubMed] [Google Scholar]
- 115.Vassallo RR. Review: IgA anaphylactic transfusion reactions. Part I. Laboratory diagnosis, incidence, and supply of IgA-deficient products. Immunohematology (2004) 20(4):226–33. [PubMed] [Google Scholar]
- 116.Schmidt AP, Taswell HF, Gleich GJ. Anaphylactic transfusion reactions associated with anti-IgA antibody. N Engl J Med (1969) 280(4):188–93. 10.1056/NEJM196901232800404 [DOI] [PubMed] [Google Scholar]
- 117.Steenholdt C, Svenson M, Bendtzen K, Thomsen OO, Brynskov J, Ainsworth MA. Acute and delayed hypersensitivity reactions to infliximab and adalimumab in a patient with Crohn’s disease. J Crohns Colitis (2012) 6(1):108–11. 10.1016/j.crohns.2011.08.001 [DOI] [PubMed] [Google Scholar]
- 118.Cheifetz A, Smedley M, Martin S, Reiter M, Leone G, Mayer L, et al. The incidence and management of infusion reactions to infliximab: a large center experience. Am J Gastroenterol (2003) 98(6):1315–24. 10.1111/j.1572-0241.2003.07457.x [DOI] [PubMed] [Google Scholar]
- 119.Hedin H, Richter W, Messmer K, Renck H, Ljungstrom KG, Laubenthal H. Incidence, pathomechanism and prevention of dextran-induced anaphylactoid/anaphylactic reactions in man. Dev Biol Stand (1980) 48:179–89. [PubMed] [Google Scholar]
- 120.Umeda Y, Fukumoto Y, Miyauchi T, Imaizumi M, Shimabukuro K, Mori Y, et al. [Anaphylactic shock related to aprotinin induced by anti-aprotinin immunoglobulin G antibody alone; report of a case]. Kyobu Geka (2007) 60(1):69–71. [PubMed] [Google Scholar]
- 121.Bergamaschini L, Mannucci PM, Federici AB, Coppola R, Guzzoni S, Agostoni A. Posttransfusion anaphylactic reactions in a patient with severe von Willebrand disease: role of complement and alloantibodies to von Willebrand factor. J Lab Clin Med (1995) 125(3):348–55. [PubMed] [Google Scholar]
- 122.Laroche D, Namour F, Lefrancois C, Aimone-Gastin I, Romano A, Sainte-Laudy J, et al. Anaphylactoid and anaphylactic reactions to iodinated contrast material. Allergy (1999) 54(Suppl 58):13–6. 10.1111/j.1398-9995.1999.tb04726.x [DOI] [PubMed] [Google Scholar]
- 123.Kishimoto TK, Viswanathan K, Ganguly T, Elankumaran S, Smith S, Pelzer K, et al. Contaminated heparin associated with adverse clinical events and activation of the contact system. N Engl J Med (2008) 358(23):2457–67. 10.1056/NEJMoa0803200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Atkinson TP, Kaliner MA. Anaphylaxis. Med Clin North Am (1992) 76(4):841–55. 10.1016/S0025-7125(16)30328-5 [DOI] [PubMed] [Google Scholar]
- 125.Simons FE, Ardusso LR, Bilo MB, El-Gamal YM, Ledford DK, Ring J, et al. World Allergy organization anaphylaxis guidelines: summary. J Allergy Clin Immunol (2011) 127(3):587–93.e1–22. 10.1016/j.jaci.2011.01.038 [DOI] [PubMed] [Google Scholar]
- 126.Demoly P, Adkinson NF, Brockow K, Castells M, Chiriac AM, Greenberger PA, et al. International consensus on drug allergy. Allergy (2014) 69(4):420–37. 10.1111/all.12350 [DOI] [PubMed] [Google Scholar]
- 127.Mayorga C, Celik G, Rouzaire P, Whitaker P, Bonadonna P, Cernadas JR, et al. In vitro tests for drug hypersensitivity reactions. An ENDA/EAACI drug allergy interest group position paper. Allergy (2016) 71(8):1103–34. 10.1111/all.12886 [DOI] [PubMed] [Google Scholar]
- 128.Brockow K, Garvey LH, Aberer W, Atanaskovic-Markovic M, Barbaud A, Bilo MB, et al. Skin test concentrations for systemically administered drugs – an ENDA/EAACI drug allergy interest group position paper. Allergy (2013) 68(6):702–12. 10.1111/all.12142 [DOI] [PubMed] [Google Scholar]
- 129.Joint Task Force on Practice Parameters, American Academy of Allergy, Asthma and Immunology, American College of Allergy, Asthma and Immunology, Joint Council of Allergy, Asthma and Immunology. Drug allergy: an updated practice parameter. Ann Allergy Asthma Immunol (2010) 105(4):259–73. 10.1016/j.anai.2010.08.002 [DOI] [PubMed] [Google Scholar]
- 130.Fernandez TD, Torres MJ, Blanca-Lopez N, Rodriguez-Bada JL, Gomez E, Canto G, et al. Negativization rates of IgE radioimmunoassay and basophil activation test in immediate reactions to penicillins. Allergy (2009) 64(2):242–8. 10.1111/j.1398-9995.2008.01713.x [DOI] [PubMed] [Google Scholar]
- 131.Gomez E, Blanca-Lopez N, Torres MJ, Requena G, Rondon C, Canto G, et al. Immunoglobulin E-mediated immediate allergic reactions to dipyrone: value of basophil activation test in the identification of patients. Clin Exp Allergy (2009) 39(8):1217–24. 10.1111/j.1365-2222.2009.03237.x [DOI] [PubMed] [Google Scholar]
- 132.Kvedariene V, Kamey S, Ryckwaert Y, Rongier M, Bousquet J, Demoly P, et al. Diagnosis of neuromuscular blocking agent hypersensitivity reactions using cytofluorimetric analysis of basophils. Allergy (2006) 61(3):311–5. 10.1111/j.1398-9995.2006.00978.x [DOI] [PubMed] [Google Scholar]
- 133.Aberer W, Bircher A, Romano A, Blanca M, Campi P, Fernandez J, et al. Drug provocation testing in the diagnosis of drug hypersensitivity reactions: general considerations. Allergy (2003) 58(9):854–63. 10.1034/j.1398-9995.2003.00279.x [DOI] [PubMed] [Google Scholar]
- 134.Iammatteo M, Blumenthal KG, Saff R, Long AA, Banerji A. Safety and outcomes of test doses for the evaluation of adverse drug reactions: a 5-year retrospective review. J Allergy Clin Immunol Pract (2014) 2(6):768–74. 10.1016/j.jaip.2014.08.001 [DOI] [PubMed] [Google Scholar]
- 135.Schwartz LB. Diagnostic value of tryptase in anaphylaxis and mastocytosis. Immunol Allergy Clin North Am (2006) 26(3):451–63. 10.1016/j.iac.2006.05.010 [DOI] [PubMed] [Google Scholar]
- 136.Garvey LH, Bech B, Mosbech H, Krøigaard M, Belhage B, Husum B, et al. Effect of general anesthesia and orthopedic surgery on serum tryptase. Anesthesiology (2010) 112(5):1184–9. 10.1097/ALN.0b013e3181d40383 [DOI] [PubMed] [Google Scholar]
- 137.Borer-Reinhold M, Haeberli G, Bitzenhofer M, Jandus P, Hausmann O, Fricker M, et al. An increase in serum tryptase even below 11.4 ng/mL may indicate a mast cell-mediated hypersensitivity reaction: a prospective study in hymenoptera venom allergic patients. Clin Exp Allergy (2011) 41(12):1777–83. 10.1111/j.1365-2222.2011.03848.x [DOI] [PubMed] [Google Scholar]
- 138.Lin RY, Schwartz LB, Curry A, Pesola GR, Knight RJ, Lee H-S, et al. Histamine and tryptase levels in patients with acute allergic reactions: an emergency department-based study. J Allergy Clin Immunol (2000) 106(1, Pt 1):65–71. 10.1067/mai.2000.107600 [DOI] [PubMed] [Google Scholar]
- 139.Keyzer JJ, de Monchy JG, van Doormaal JJ, van Voorst Vader PC. Improved diagnosis of mastocytosis by measurement of urinary histamine metabolites. N Engl J Med (1983) 309(26):1603–5. 10.1056/NEJM198312293092603 [DOI] [PubMed] [Google Scholar]
- 140.Stephan V, Zimmermann A, Kuhr J, Urbanek R. Determination of N-methylhistamine in urine as an indicator of histamine release in immediate allergic reactions. J Allergy Clin Immunol (1990) 86(6 Pt 1):862–8. 10.1016/S0091-6749(05)80147-2 [DOI] [PubMed] [Google Scholar]
- 141.Simons FE, Frew AJ, Ansotegui IJ, Bochner BS, Golden DB, Finkelman FD, et al. Risk assessment in anaphylaxis: current and future approaches. J Allergy Clin Immunol (2007) 120(1 Suppl):S2–24. 10.1016/j.jaci.2007.05.001 [DOI] [PubMed] [Google Scholar]
- 142.Alrasbi M, Sheikh A. Comparison of international guidelines for the emergency medical management of anaphylaxis. Allergy (2007) 62(8):838–41. 10.1111/j.1398-9995.2007.01434.x [DOI] [PubMed] [Google Scholar]
- 143.Sheikh A, Ten Broek V, Brown SG, Simons FE. H1-antihistamines for the treatment of anaphylaxis: Cochrane systematic review. Allergy (2007) 62(8):830–7. 10.1111/j.1398-9995.2007.01435.x [DOI] [PubMed] [Google Scholar]
- 144.Choo KJ, Simons E, Sheikh A. Glucocorticoids for the treatment of anaphylaxis: Cochrane systematic review. Allergy (2010) 65(10):1205–11. 10.1111/j.1398-9995.2010.02424.x [DOI] [PubMed] [Google Scholar]
- 145.Muraro A, Roberts G, Worm M, Bilo MB, Brockow K, Fernandez Rivas M, et al. Anaphylaxis: guidelines from the European Academy of Allergy and Clinical Immunology. Allergy (2014) 69(8):1026–45. 10.1111/all.12437 [DOI] [PubMed] [Google Scholar]