Abstract
Objectives:
To assess the benefit of using the flash glucose monitoring system (FGMS) in children and adolescents with type 1 diabetes mellitus (T1DM) during Ramadan fasting.
Methods:
A prospective pilot study of 51 participants visited the pediatric diabetes clinic at King Abdulaziz University Hospital, Jeddah, Kingdom of Saudi Arabia from between June until and July 2016. The FreeStyle® Libre™ FGMS (Abbott Diabetes Care, Alameda, CA, USA) was used. Hypoglycemia was defined as glucose values of less than 70 mg/dL, while hyperglycemia as glucose values of more than 150 mg/dL for all participants based on our institute’s protocol.
Results:
Participants were able to fast for 67.0% of the total days eligible for fasting, whereas they did not fast on 33% of the days due to either hypoglycemia (15.4%) or non-diabetes-related reasons (17.6 %). None of the participants developed severe hypoglycemia. The mean number of hyperglycemic episodes during fasting hours was 1.29, per day, which was higher than that of hypoglycemic episodes (0.7). None of the participants developed diabetic ketoacidosis (DKA). Glycemic control with mean of estimated hemoglobin A1C reading during Ramadan (8.16 ± 1.64% [pre study]) to 8.2 ± 1.63% [post study] p=0.932.
Conclusions:
Children and adolescents with T1DM who use the FGMS could fast without the risk of life-threatening episodes of severe hypoglycemia (namely seizure, coma), or DKA during Ramadan. Adequate education and good glycemic control prior to Ramadan are important strategies in combination with the use of an FGMS to achieve better outcome.
Fasting during the month of Ramadan is the fourth of Islam’s 5 pillars of faith; Ramadan is the ninth month of the Hijri calendar.1 Fasting is obligatory for all pubertal Muslims and consists of abstaining from eating and drinking from dawn to sunset.1,2 People with chronic diseases, such as type 1 diabetes mellitus (T1DM), who are on insulin therapy by either multiple daily injections (MDIs) or continuous subcutaneous insulin infusion (CSII) regimens, need to monitor their glucose more frequently to fast safely and avoid the risk of developing episodes of symptomatic or asymptomatic hypoglycemia and/or hyperglycemia.1 Self-monitoring of blood glucose with glucometers, which measure capillary blood glucose values, has been used worldwide for many years. This invasive method can cause pain to children and adolescents with diabetes,3 especially if they have to monitor their blood glucose several times a day during fasting hours, which was 15 hours per day in the year of 2016 at Jeddah city, to reduce the potential risk of hypoglycemia, hyperglycemia, dehydration, and ketoacidosis.2,4 Blood glucose level after Suhoor (last meal before dawn time) and Iftar (meal that breaks the fast) should be checked to avoid postprandial hyperglycemia or hypoglycemia.5 The flash glucose monitoring system (FGMS), by Abbott Diabetes Care, Alameda, CA, USA, is a system where patients can use a meter to non-invasively scan a subcutaneously inserted sensor, providing both a sensor glucose value, and a trend arrow. The FGMS, by virtue of the ease of frequent non-invasive testing, could guide patients and physicians to achieve better diabetes management by facilitating easier adjustment of insulin daily doses, changing dietary habits, and encouraging more physical activities, with consequence better glycemic control by continuous observation of glucose reading by participants and parents.6 This technology could also help diabetic patients to fast in a safer manner, as it has the capability to show changes in glucose levels at any time throughout the day and night.7 Moreover, the FGMS could guide patients and physicians to achieve better diabetes management by facilitating easier adjustment of insulin daily doses, changing dietary habits, and encouraging more physical activities.6 Limited studies are available on the use of different non-invasive glucose monitoring technologies by children and adolescents with T1DM who fast during Ramadan.8,10 In this study, we aimed to assess the beneficial effects of using the FreeStyle® Libre™ FGMS (Abbott Diabetes Care, Alameda, CA, USA) in children and adolescents with T1DM during Ramadan.
Methods
Study design
A prospective single-armed pilot study included 51 pubertal children and adolescents aged 10-20 years (mean age, 14.2 ± 2.6 years; 43.1% male, 56.8% female). Selected participants were religiously obliged to fast during Ramadan. All participants were on intensive insulin therapies by either MDI or insulin pump regimens. They were recruited to participate in the study from the pediatric diabetes outpatient clinic at King Abdulaziz University Hospital, Jeddah, Kingdom of Saudi Arabia.
Participants
Participants were under 1-month clinical follow-up (from 6 June to 5 July 2016). All together with their parents had 3 (20 minutes) educational sessions prior to participation in the study, on how to use the FGMS FreeStyle® Libre™ (Abbott Diabetes Care) and how to interpret the information on the device screen prior to the start of the study. The parents of young children and adolescents with diabetes were taught to administer correction boluses of fast/short acting insulin in hyperglycemic episodes of fasting or non-fasting hours. Participants were discouraged to do physical activities while fasting, and advised to do them in non-fasting hours of Ramadan month. The parents were provided with all contact details of the study team in case of any technical or medical concerns. Each participant received 2 sensors (additional one was given as an extra in case of sensors detachment), as most of patches have been staying for period of 10-14 days unless participants were using frequent bathing, diary to be filled up and a flash reader device, all were free of charge. Participants were requested to visit the clinic twice a month, in order to change the sensor and to download the data stored in the reader into a FreeStyle® Libre™ application on a computer to assess ambulatory glucose profile, median glucose profile, hypoglycemic and hyperglycemic events. The estimated hemoglobin A1C (HbA1C) values of both pre and post month of Ramadan were calculated electronically by the device. Participants were asked to measure the glucose level with a glucometer whenever hypoglycemic or hyperglycemic episodes occurred to confirm the accuracy of the device.
Glycemic data
All stored data were reviewed, including the mean blood glucose values, minimum and maximum glucose values, and area above and under the curve for glucose readings. For the purpose of the study, we selected glucose values of <70 mg/dL as the lower target reading and >150 mg/dL as the higher target reading for all participants based on our institute protocol.11 Estimated HbA1C values calculated by the device software program were determined at 0, 2, and 4 weeks of the study.
Flash glucose monitoring system
Freestyle® Libre™ sensor measures the interstitial fluid glucose values. The sensor is small, water-resistant and designed to be fixed on the lateral aspects of the upper arm for duration of 14 days. Sensor’s users could perform their usual daily activities such as showering, swimming, and exercising. Frequent scanning of the sensor by a reader could help the participants to obtain their glucose data for the last 8 hours. The accuracy of FreeStyle® Libre™ sensor‘s numerical readings and clinical accuracy has been reported as 11.4% compared with glucometers.12
Sensor’s arrows system
Various directions of arrows system were provided with FGMS sensor to observe glucose changes. Straight upward direction indicates, if mean glucose value increased by more than 2 mg/dL per minute; oblique upward direction, if mean glucose value increased between 1 and 2 mg/dL per minute; flat arrow direction, if mean glucose value is less than 1 mg/dL per minute; oblique downward direction, if mean glucose value decreased between 1 and 2 mg/dL per minute; and straight downward direction, if mean glucose value decreased by more than 2 mg/dL per minute. All participants were taught on how to manage glucose levels changes at home depending on various arrows’ directions. For example, if the arrow is straight upward, the participant has to do a physical activity or administer an extra correction dose of insulin. If the direction is flat, no action should be taken, and if the direction is downward, participants should break their fast by having an extra small snack to avoid hypoglycemia.
Participants’ diary
A detailed diary was provided to be filled up by the participants during Ramadan. The diary contained a schedule of all the days of Ramadan. On each day, the participants had to indicate whether they fasted, and if not, the reason was to be provided. Every hypoglycemic or hyperglycemic event detected by both the glucometer and FreeStyle® Libre™ readings had to be reported and whether these episodes occurred during fasting or non-fasting hours. Participants were requested to test for the presence of ketones whenever they had high glucose readings.
Inclusion and exclusion criteria
Inclusion criteria were children and adolescents with T1DM who were all religiously eligible for Ramadan fasting and on intensive insulin therapy. Exclusion criteria were those with T2DM, or diabetes complications, namely; nephropathies, retinopathies, or other associations, such as malnutrition and celiac disease.
Statistical analysis
Data were entered, coded, and analyzed using Microsoft Office Excel (version 2010; Microsoft, Redmond, Washington, USA) and the Statistical Package for Social Science (SPSS Inc., Chicago, IL, USA) version 16. Descriptive statistics were reported as proportions for qualitative variables and as maximum, minimum, mean, and standard deviation for quantitative variables. The mean of hyperglycemic versus hypoglycemic episode during fasting and non-fasting hours and their percentages among participants on MDI versus insulin pump therapy were determined. The frequency of hypoglycemic symptoms and the percentages of hypoglycemic awareness were also reported. Paired sample t-test used to test the mean difference of (high and low glucose level among before and after fasting), after we have assumed that the data followed a normal distribution to examine the significant difference of mean estimated HbA1C values at the beginning and end of the study. A P value of < 0.05 was considered statistically significant.
Results
Clinical characteristics
Fifty-one participants (22 male [43.1%] and 29 female [56.9%]) were recruited. Their mean age was 14.2 ± 2.6 years. The participants comprised of 34 Saudis (66.7%) and 17 (33.3%) non-Saudis. All of them were on intensive insulin therapies; 33 (65%) were on MDIs and 18 (35%) were on insulin pump therapy.
Fasting days and related events
The total days eligible for fasting in the month of Ramadan for 51 participants in 2016 were 1530. Complete participants data were available in 1123 days; 752 (67%) days during fasting for 1123 days, and the remaining 371 (33.0%) days of not fasted. The causes of non-fasting were hypoglycemia, 173/1123 days (15.4%) and non-diabetes-related reasons, 198/1123 days (17.6%) The hyper/hypoglycemic episodes were arranged according to fasting hours (5:00 a.m. to 7:00 p.m.) and non-fasting hours (7:01 p.m. to 4:59 a.m.).
The mean of hyperglycemic episodes was 1.24 ± 0.8 (range, 0.07-3.6) in fasting hours and 0.7± 0.44 (range, 0-2.69) in non-fasting hours (p=0.0001). The mean of hypoglycemic episodes was 0.56 ± 0.35 (range, 0-7) in fasting hours and 0.18 ± 0.16 (range, 0-0.85) in non-fasting hours (p=0.0001). During hypoglycemic episodes, 90% of subjects developed symptomatic hypoglycemia, whereas 5 (10%) were asymptomatic. The participants listed a number of symptoms as shown in Figure 1. Fasting and non-fasting days according to the type of treatment (pump versus MDI) are represented in (Table 1). In the month of Ramadan, hypoglycemic episodes with total of 273 episodes (pump) and 354 (MDI) in addition to hyperglycemic episodes with total 459 (pump) and 682 (MDI), which are shown in (Table 2). The mean result of estimated HbA1C at the beginning of the study was 8.16 ± 1.6, whereas the estimated HbA1C at the end of the study was 8.20 ± 1.6% (p=0.932). A comparison between the mean of estimated HbA1C values calculated by the FreeStyle® Libre™ device at the beginning and end of the study with mean changes of (8.16 ± 1.64% to 8.2 ± 1.63%) p=0.932.The mean blood glucose reading, minimum and maximum glucose values, and area above and under the curve for glucose readings are shown in (Table 3).
Figure 1.
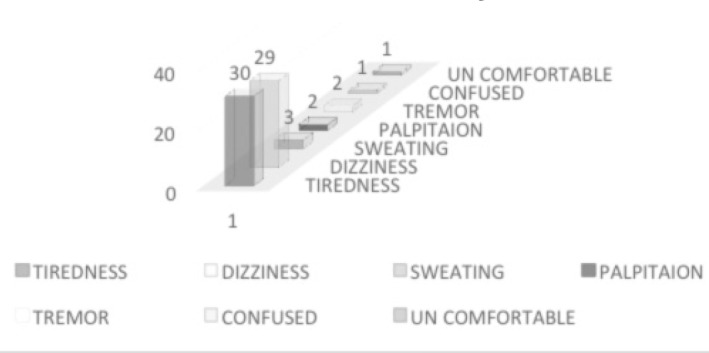
Frequency of hypoglycemic symptoms
Table 1.
Fasting and non-fasting days according to type of treatment.
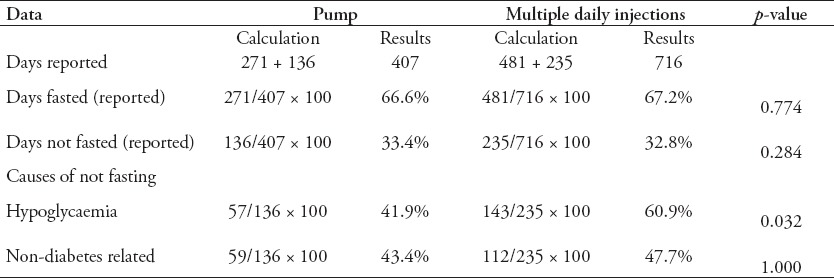
Table 2.
Hypoglycemia and hyperglycemia during fasting and non-fasting hours with type of treatment.
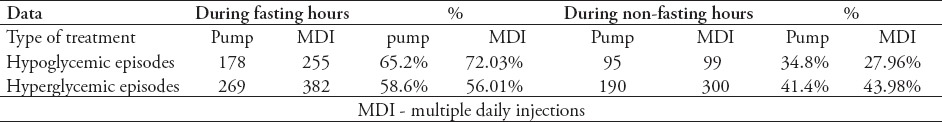
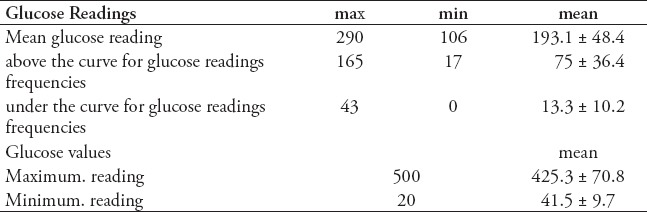
Table 3.
The mean blood glucose reading, minimum and maximum glucose values (mg/dl), and area above and under the curve for glucose readings.
Discussion
Fasting Ramadan is a religious activity. Many Muslim adolescents start their fasting upon completion of their pubertal development (namely, onset of menarche in girls and spermarche in boys), which is usually a new challenge and interesting experience for them. However, the challenge is greater for adolescents with T1DM, as they do not want to feel different from the healthy adolescent peers while they need to maintain their blood glucose levels within a safe range as much as possible. The unwanted adverse effects of fasting in these patients are a huge concern, particularly for their parents, colleagues, and treating physicians. During fasting, these adolescents are at risk of having hypoglycemia, either symptomatic or asymptomatic, in addition to the risk of hyperglycemia with/without ketosis and acidosis.
Hyperglycemic episodes during fasting hours of the day could be due to the release of certain counterregulatory hormones (for example, catecholamine, growth hormone, and cortisone) to overcome the fasting process and overcompensation after treating hypoglycemia. In the current study, the frequency of these events was higher than that of hypoglycemic events. This result could indicate that adolescents with T1DM are at a higher risk of experiencing hyperglycemic events than hypoglycemic events during fasting hours and days.11 All participants have been taught in pre-fasting educational session to have correction polices in order to avoid risk of developing DKA. Hyperglycemic episodes that occur during non-fasting hours could be due to the large amount of consumed carbohydrates, which is a common non-healthy habit that is frequently observed in most community members, whether they have diabetes mellitus or not. No single episode of hyperglycemia was associated with ketoacidosis in the current study.
Hypoglycemia could occur during fasting and non-fasting hours. During fasting hours, hypoglycemia could be attributed to abstaining any food for a long period of time (fasting was for 14 continuous hours a day). Hypoglycemic episodes during non-fasting hours are often due to insulin overdose or physical activity. Symptomatic hypoglycemia was present in 90% of hypoglycemic episodes, whereas asymptomatic hypoglycemia in 10%, which was detected by sensor readings and confirmed by glucometers. Therefore, the FGMS helped 10% of all participants in the current study to detect hypoglycemia and act earlier by breaking their fast immediately as indicated by the Islamic religion. This is one of the advantages of this device to prevent any further major acute comorbidity associated with hypoglycemia. Hypoglycemic symptoms were arranged according to their frequency (Figure 1). Interestingly, no single report of serious consequences of sever hypoglycemia (seizure or coma) occurred during the study, which may indicate the importance of FGMS in preventing life-threatening conditions in diabetic patients.
All of the participants were on intensive insulin therapy (pump/MDI). Children and adolescents on MDI fasted 481 days (67.2%) while on pump therapy 271 days (66.6%). The children and adolescents in the latter therapy broke their fast due to non-diabetes-related causes (43.4%) more frequently than due to hypoglycemia (41.9%). Moreover, those participants who were on MDI broke their fast due tohypoglycemia (60.9%) more frequently than because of non-diabetes-related causes (47.7%). Hyperglycemic episodes in participants on pump therapy were reported to be 58.6% during fasting hours compared with those in participants on MDI 56%. In non-fasting hours, the occurrence of these episodes in children and adolescents on pump therapy were 41.4% and that in participants on MDI were 43.98%. The frequency of hypoglycemic episodes in participants on pump therapy (65.2%) during fasting hours was lower compared with that in participants on MDI (72.03%).This finding indicates the advantages of using pump therapy instead of MDI, which is consistent with the results of previous studies.
A similar study conducted in the United Arab of Emirates reported that diabetic patients can fast safely during Ramadan as no life-threatening events occur, such as severe hypoglycemia and diabetic ketoacidosis (DKA).Participants who experienced hypoglycemia and hyperglycemia not only broke their fasting for diabetes-related issues, but also for other reasons such as menses, sickness, and traveling.8 In the current study, most of the participants with T1DM fasted more than half of the Ramadan period.13 Participants on insulin pump can easily adjust the basal rate during fasting hours compared to those on MDI. Participants on MDI broke their fast more frequently than those on insulin pump.14
The mean result of estimated HbA1C at the beginning of the study was 8.16 ± 1.64%, whereas the estimated HbA1C at the end of the study was 8.2 ± 1.63% (p=0.932).The diabetologist should adjust the basal rate of the insulin pump according to blood glucose variability, which is shown in the FreeStyle® Libre™ records.13 The FGMS as a non-invasive monitoring method during fasting and non-fasting hours may recognize hyperglycemic events, and even postprandial and asymptomatic hypoglycemia.15 The mean glucose reading was 193.1 ± 48.4 mg/dl. Regarding the area above and under the curve for glucose readings frequency, this shows a mean of 75 ± 36.4 mg/dl for above the curve and 13.3 ± 10.2 mg/dl for under the curve. The maximum glucose values were 500 mg represent a mean of 425.3 ± 70.8 mg/dl and minimum with 20 mg/dl represent a mean of 41.5 ± 9.7 mg/dl. No reported skin reactions of itchiness and skin sensitivity of the sensors, dislodgement problems, or catching the sensor on clothing.
Study limitations
The study design has no control group to compare with. Patient follow-up compliance was difficult to attain. The adhesive patches of the sensors were unstable with recurrent falls, and literature related to the current study with data for comparison is limited. Regarding data missing was 7.9 % per participants owing to either family travel or missing clinic appointment.
In conclusion, new diabetes technology such as FGMS could lead to better diabetes care. The usage of the FGMS by frequent scanning of the sensor could lead to earlier detection of hypoglycemic and hyperglycemic episodes. No DKA episodes were reported.
Footnotes
References
- 1.Ibrahim MA. Managing diabetes during Ramadan. Diabetes Voice. 2007;52:19–22. [Google Scholar]
- 2.Al-Arouj M, Bouguerra R, Buse J, Hafez S, Hassanein M, Ibrahim MA, et al. Recommendations for management of diabetes during Ramadan. Diabetes Care. 2005;28:2305–2311. doi: 10.2337/diacare.28.9.2305. [DOI] [PubMed] [Google Scholar]
- 3.Ding S, Schumacher M. Sensor Monitoring of Physical Activity to Improve Glucose Management in Diabetic Patients: A Review. Sensors. 2016;16:589. doi: 10.3390/s16040589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Benaji B, Mounib N, Roky R, Aadil N, Houti IE, Moussamih S, et al. Diabetes and Ramadan: review of the literature. Diabetes Res Clin Pract. 2006;73:117–125. doi: 10.1016/j.diabres.2005.10.028. [DOI] [PubMed] [Google Scholar]
- 5.Elbarbary NS. Effectiveness of the Low Glucose Suspend Feature of Insulin Pump During Fasting in Ramadan in Type 1 Diabetes Mellitus. Diabetes Metab Res Rev. 2016;32:623–633. doi: 10.1002/dmrr.2781. [DOI] [PubMed] [Google Scholar]
- 6.Bailey T, Bode BW, Christiansen MP, Klaff LJ, Alva S. The Performance and Usability of a Factory-Calibrated Flash Glucose Monitoring System. Diabetes Technol Ther. 2015;17:787–794. doi: 10.1089/dia.2014.0378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.AbottDiabetes Care. AbottDiabetes Care 2017 in Witney. UK: Oxfordshire; 2016. Available from http://www.freestylelibre.co.uk/ [Google Scholar]
- 8.Musleh AS, Beshyah SA, Abu Awad SM, Kahwatih M, Al Jubeh JM. Experience with Diabetic Adolescents Observing Ramadan Fasting. Ibnosina J Med BS. 2015;7:223–227. [Google Scholar]
- 9.Beshyah SA, Haddad M. Impact of Socializing, Fasting and Feasting on Day to Day Blood Glucose Profiles in Diabetes Elucidated by the FreeStyle®Libre™System. Ibnosina J Med BS. 2016;8:114–119. [Google Scholar]
- 10.Lessan N, Hannoun Z, Hasan H, Barakat MT. Glucose excursions and glycaemic control during Ramadan fasting in diabetic patients: Insights from continuous glucose monitoring (CGM) Diabetes Metab. 2015;41:28–36. doi: 10.1016/j.diabet.2014.11.004. [DOI] [PubMed] [Google Scholar]
- 11.Al-Arouj M, Assaad-Khalil S, Buse J, Fahdil I, Fahmy M, Hafez S, et al. Recommendations for Management of Diabetes During Ramadan Update 2010. Diabetes Care. 2010;33:1895–1902. doi: 10.2337/dc10-0896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bailey T, Bode BW, Christiansen MP, Klaff LJ, Alva S. The Performance and Usability of a Factory-Calibrated Flash Glucose Monitoring System. Diabetes Technology and Therapeutics. 2015;17:787–794. doi: 10.1089/dia.2014.0378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kaplan W, Afandi B. Blood glucose fluctuation during Ramadan fasting in adolescents with type 1 diabetes: findings of continuous glucose monitoring. Diabetes Care. 2015;38:e162–e163. doi: 10.2337/dc15-1108. [DOI] [PubMed] [Google Scholar]
- 14.Alsahli M, Gerich JE. Hypoglycemia in patients with diabetes and renal disease. J Clin Med. 2015;4:948–964. doi: 10.3390/jcm4050948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Phillip M, Danne T, Shalitin S, Buckingham B, Laffel L, Tamborlane W, et al. Use of continuous glucose monitoring in children and adolescents. Pediatr Diabetes. 2012;13:215–228. doi: 10.1111/j.1399-5448.2011.00849.x. [DOI] [PubMed] [Google Scholar]


