Abstract
Background:
Hypertension (HTN) is a major cause of noncommunicable diseases. In this study, we report the prevalence rate of HTN in Birjand population.
Methods:
This cross-sectional study was conducted on 1286 individuals in Birjand in 2014. Individuals with systolic blood pressure (SBP) ≥140 mmHg and/or diastolic blood pressure (DBP) ≥90 mmHg were considered as hypertensive. Data were analyzed using Chi-square test, independent t-test, and one-way ANOVA. P < 0.05 was considered as statistically significant.
Results:
Among the 1286 participants, 659 were women (51.2%). Prevalence of HTN was 20.1% (10.3% systolic HTN and 6.9% diastolic HTN). Prevalence self-reported HTN was 12.3%. SBP and DBP means were higher in men (P < 0.001). Mean scores of SBP and DBP increased by aging and body mass index (P < 0.001). Diabetic individuals had higher SBP scores (P < 0.001). Dyslipidemic patients had greater SBP and DBP (P < 0.001).
Conclusions:
Prevalence of HTN in our study is high. About one-fifth of the participants had HTN. In addition, BP is higher in men, elderly, and diabetic individual. Therefore, it is necessary to control BP regularly in different groups in society.
Keywords: Diastolic blood pressure, hypertension, Iran, prevalence, systolic blood pressure
Introduction
According to the global burden of disease study 2010, prevalence of hypertension (HTN) in both economically developed and developing countries is high. It is also highlighted that high blood pressure (BP) has a huge impact on the burden of heart disease and stroke worldwide.[1,2] Accordingly, the World Health Organization (WHO) aimed to decrease the prevalence of HTN by 25%.[3] Yazdanpanah et al. indicated that the prevalence of HTN was 17.58% in Ahwaz, Southwest of Iran.[4] Malekzadeh et al. revealed that female sex, increased body mass index (BMI) values, and lack of physical activity were the risk factors for HTN in North of Iran.[5]
In the present study, we report the prevalence and associated risk factors of HTN among Iranian adults in Birjand in 2014.
Methods
Participants
This cross-sectional study was conducted on 1286 individuals (627 men and 659 women) aged 15–70 years. According to the Iranian Statistics Center, the population of Birjand is 259,506 which includes 132,247 men, 127,259 women, and 71,384 families.[6] Multistage cluster sampling was used as the sampling method, holding 250 cluster heads and 20 samples from each cluster.
The height and weight of participants were measured by standard methods. BMI was calculated by dividing weight (kg)/height (m2). BP was measured from the right arm in the sitting position with a mercury sphygmomanometer (ALPK2). At least two measurements were performed, and the average was recorded.
Individuals with systolic BP (SBP) ≥140 mmHg and/or diastolic BP (DBP) ≥90 mmHg and/or those on treatment with antihypertensive drugs were considered as hypertensive individuals. Based on the JNC 7 report,[7] the participants were classified as normal HTN (BP <120/80 mmHg), pre-HTN (120–139/80–89) Stage I (119/90–99), and Stage II HTN (≥160/100). Blood sugar and lipid profile were measured after 12 h of fasting by the standard enzymatic method (Pars Azmon Kit, Iran). According to WHO criteria, fasting blood sugar (FBS) <110 mg/dl is normal, 110 ≤ FBS <126 mg/dl is prediabetic, and FBS ≥ 126 is diabetic.[8]
Individuals were classified as underweight (<18.5 kg/m2), healthy weight (18.5–24.9 kg/m2), overweight (25–29.9 kg/m2), and obese (≥30 kg/m2) according to WHO classification.[9] If a patient had at least one criteria such as high cholesterol (>240), non-HDL-C (>160), high triglyceride (>200), high LDL (>130), or low HDL (<40 for men and < 50 for female), s/he can be considered dyslipidemic (DLP) patient.[10]
Statistical methods
The data were analyzed using SPSS software for Windows release 22.0 (SPSS, Chicago, IL, USA). Descriptive analysis was used to determine the percentage, mean, and standard error of patients’ clinical and characteristics variables. Moreover, Chi-square test was used to investigate association between demographic variables and HTN. Normality test was performed by Kolmogorov–Smirnov test, and Leven test was performed to evaluate homogeneity of variances. Student's t-test and ANOVA test were used to evaluate differences of continues variables such as SBP and DBP among demographic variable groups with Tukey's post hoc. P < 0.05 was considered as statistically significant.
Results
From among 1286 participants, 51.2% were women and 37.1% were overweight. Prevalence of diabetes mellitus (DM), DLP, and smoking was 5.8%, 88.9%, and 5.4%, respectively. Prevalence of self-reported HTN and HTN was 12.3% and 20.1%, respectively. Demographic and other characteristics of participants are reported in Table 1.
Table 1.
Demographic and other characteristics of participants in the study

Table 2 shows distribution of different BP categories. Based on the results, most of the individuals in all age categories had normal BP. However, most of the obese and diabetic patients had pre-HTN. Figure 1 shows that prevalence of pre-HTN, Stage I HTN, and Stage II HTN were higher in men than in women.
Table 2.
Distribution of different blood pressure categories according to age and cardiac risk factors
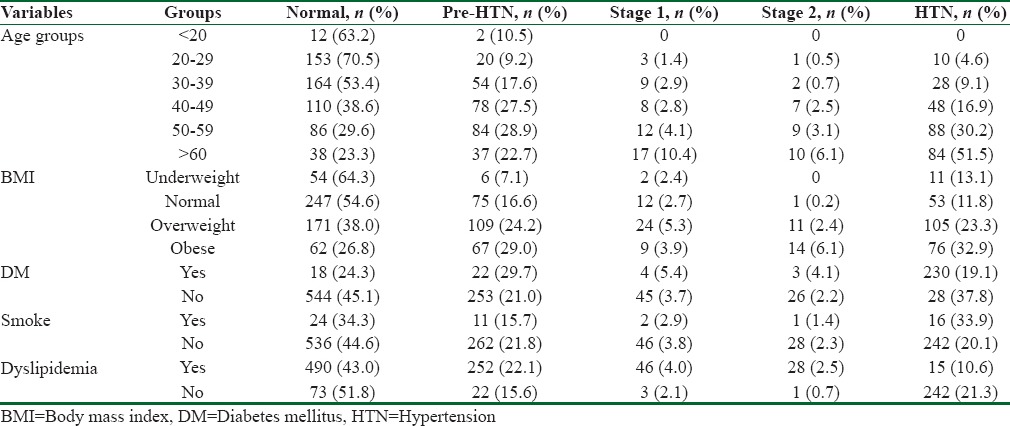
Figure 1.
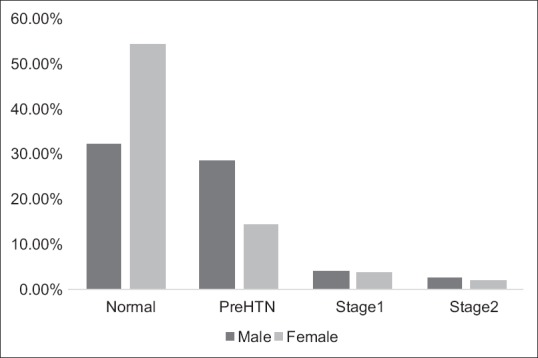
Percent of different HTN categories in both sex
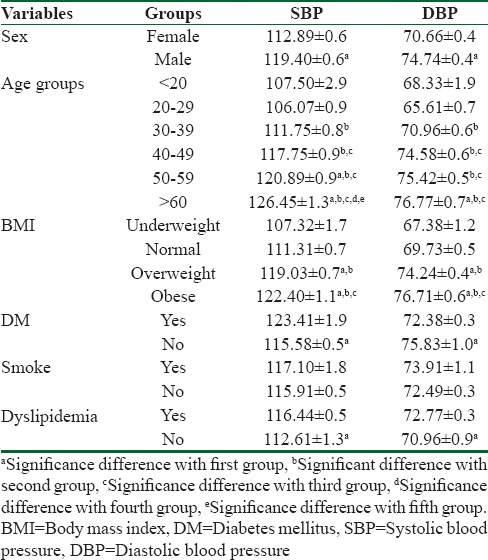
According to Table 3, mean SBP and DBP values increased with age and higher BMI values (P < 0.001) and they increased with age and higher BMI values in a significant manner (P < 0.001). Individuals with DM had higher SBP values (P < 0.001). DLP patients had higher SBP and DBP values (P < 0.001). Diabetic patients had higher mean SBP values than nondiabetic ones (P < 0.001). Patients with DLP displayed higher SBP and DBP values than others (P < 0.001).
Table 3.
Mean±standard error of systolic blood pressure and diastolic blood pressure in age, body mass index, diabetes mellitus, smoke, and dyslipidemia groups
Discussion
This is the first report on HTN prevalence and its risk factors among general population of Birjand, Center of South Khorasan, East of Iran. In our study, the prevalence of HTN was 20.1%. HTN prevalence in Birjand has previously been investigated in two studies, one among nurses and the other in Imam Khomeini Relief Committee (IKRF). Kazemi et al. indicated that one-fifth of IKRF had HTN while 40% of those subjects were unaware of their problem; the prevalence of HTN among nurses in Birjand in 2011 was 9.1%.[11,12]
Prevalence of HTN was reported 25.6% in Yazd Healthy Heart Project,[13] and 17.58% in Ahwaz, Southwest of Iran.[4] Khosravi et al. indicated that the prevalence rates of HTN and pre-HTN were 38.2% and 33.6% in Shahrood, North of Iran.[14] Compared to other studies our study showed that prevalence of HTN in Birjand population was similar to Ahwaz but lower than in other areas of Iran. As for other countries, Joffres et al. indicated that HTN prevalence is 19.5% in Canada, 29% in the USA, and 30% in England.[15]
Based on the results, women's SBP and DBP mean were 112.89 ± 0.6 mmHg and 70.66 ± 0.4 mmHg, while the same values in men were 119.40 ± 0.6 mmHg and 74.74 ± 0.4 mmHg, respectively (P < 0.001). As in our study, most of the studies showed that HTN prevalence was higher among men than women.[14,16,17]
Our findings also showed that mean SBP and DBP values at age subgroup <20 years were 107.50 ± 2.9 mmHg and 68.33 ± 1.9 mmHg and increased significantly with increasing age, so mean SBP was 126.45 ± 1.3 mmHg and mean DBP was 76.77 ± 0.7 mmHg at age ≥60 years. Other studies have found similar results to those of our study.[14,16,18] HTN is a highly prevalent disorder in the elderly. Due to structural alterations of arterial wall occurring with aging, arterial stiffness increases and in turn SBP increases in old people.[19]
Mean of SBP and DBP increased also by increasing BMI values in our study. Khosravi et al. revealed that gender, BMI, and age have significant impacts on prevalence of HTN.[14] The most important identified risk factor for HTN is obesity. Obese individuals have a significantly higher risk of HTN. It is associated with hyperinsulinemia, activated renin-angiotensin system, increased sympathetic tone, increased renal sodium retention, and structural changes in the kidney. All of these factors are considered responsible for obesity-related HTN.[20]
In our study, mean SBP and DBP values were higher in DLP patients. Ostovar et al. reported that the 6-year risk of HTN was associated with overweight and obesity, age, and hyperlipidemia but not with sex in Bushehr, South of Iran.[21] HTN and DLP are often seen together. This coexistence can increase risk of cardiovascular disease exponentially. Therefore, it is necessary to control DLP and HTN to prevent premature atherosclerosis.
Mean of SBP was higher in diabetic patients in our study. Do et al. showed that the prevalence of HTN was 20.7% in Vietnamese adults and was higher among men than women; HTN was also associated with increasing age, weight, and diabetes.[22] Diabetes and HTN are commonly found together, often cluster with other cardiovascular risk factors, as described in metabolic syndrome.
Conclusions
Our findings show that prevalence of HTN among diabetic, elderly, men, and people with DLP in Birjand, Iran, is high. Therefore, it is necessary to plan screening strategies to discover new cases as well as educational programs to raise awareness in both medical and patient communities, for early detection and treatment of these important conditions.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
We would like to thank Deputy of Research and Technology of Birjand University of Medical Sciences for their financial support for this study.
References
- 1.Bromfield S, Muntner P. High blood pressure: The leading global burden of disease risk factor and the need for worldwide prevention programs. Curr Hypertens Rep. 2013;15:134–6. doi: 10.1007/s11906-013-0340-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lotfaliany M, Akbarpour S, Mozafary A, Boloukat RR, Azizi F, Hadaegh F. Hypertension phenotypes and incident cardiovascular disease and mortality events in a decade follow-up of a middle East cohort. J Hypertens. 2015;33:1153–61. doi: 10.1097/HJH.0000000000000540. [DOI] [PubMed] [Google Scholar]
- 3.Kontis V, Mathers CD, Bonita R, Stevens GA, Rehm J, Shield KD, et al. Regional contributions of six preventable risk factors to achieving the 25×25 non-communicable disease mortality reduction target: A modelling study. Lancet Glob Health. 2015;3:e746–57. doi: 10.1016/S2214-109X(15)00179-5. [DOI] [PubMed] [Google Scholar]
- 4.Yazdanpanah L, Shahbazian H, Shahbazian H, Latifi SM. Prevalence, awareness and risk factors of hypertension in Southwest of Iran. J Renal Inj Prev. 2015;4:51–6. doi: 10.12861/jrip.2015.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Malekzadeh MM, Etemadi A, Kamangar F, Khademi H, Golozar A, Islami F, et al. Prevalence, awareness and risk factors of hypertension in a large cohort of Iranian adult population. J Hypertens. 2013;31:1364–71. doi: 10.1097/HJH.0b013e3283613053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yearbook IS. Tehran, Iran: Statistical Center of Iran; 2013. [Google Scholar]
- 7.Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jr, et al. The seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure: The JNC 7 report. JAMA. 2003;289:2560–72. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- 8.Organization WH. Definition and diagnosis of diabetes mellitus and intermediate hyperglycemia: Report of a WHO consultation. Geneva: World Health Organization; 2006. [Google Scholar]
- 9.Organization WH. Global database on Body Mass Index: BMI Classification, 2006. World Health Organization; 2015. [Google Scholar]
- 10.Rodriguez CJ, Daviglus ML, Swett K, González HM, Gallo LC, Wassertheil-Smoller S, et al. Dyslipidemia patterns among hispanics/latinos of diverse background in the united states. Am J Med. 2014;127:1186–94. doi: 10.1016/j.amjmed.2014.07.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kazemi T, Rezvani MR, Sharifzadeh GR, Sadri A, Moghaddam M, Reza H, et al. The prevalence of traditional cardiovascular risk factors in low socioeconomic use individuals in Birjand 2008 (East Iran) J Cardiothorac Med. 2015;3:263–9. [Google Scholar]
- 12.Kazemi T, Sharifzadeh G, Javadinia SA, Salehiniya H. Prevalence of Cardiovascular Risk Factors among the Nurse Population in the East of Iran. Int J Travel Med Glob Health. 2015;3:133–6. [Google Scholar]
- 13.Namayandeh S, Sadr S, Ansari Z, Rafiei M. A cross-sectional study of the prevalence of coronary artery disease traditional risk factors in Yazd urban population, Yazd healthy heart project. Int Cardivasc Res J. 2011;5:7–13. [Google Scholar]
- 14.Khosravi A, Emamian MH, Shariati M, Hashemi H, Fotouhi A. The prevalence of pre-hypertension and hypertension in an Iranian urban population. High Blood Press Cardiovasc Prev. 2014;21:127–35. doi: 10.1007/s40292-013-0035-y. [DOI] [PubMed] [Google Scholar]
- 15.Joffres M, Falaschetti E, Gillespie C, Robitaille C, Loustalot F, Poulter N, et al. Hypertension prevalence, awareness, treatment and control in national surveys from England, the USA and Canada, and correlation with stroke and ischaemic heart disease mortality: A cross-sectional study. BMJ Open. 2013;3:e003423. doi: 10.1136/bmjopen-2013-003423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Aghaei Meybodi HR, Khashayar P, Rezai Homami M, Heshmat R, Larijani B. Prevalence of hypertension in an Iranian population. Ren Fail. 2014;36:87–91. doi: 10.3109/0886022X.2013.832315. [DOI] [PubMed] [Google Scholar]
- 17.Bhansali A, Dhandania VK, Deepa M, Anjana RM, Joshi SR, Joshi PP, et al. Prevalence of and risk factors for hypertension in urban and rural India: The icmr-indiab study. J Hum Hypertens. 2015;29:204–9. doi: 10.1038/jhh.2014.57. [DOI] [PubMed] [Google Scholar]
- 18.Najafipour H, Nasri HR, Afshari M, Moazenzadeh M, Shokoohi M, Foroud A, et al. Hypertension: Diagnosis, control status and its predictors in general population aged between 15 and 75 years: A community-based study in Southeastern Iran. Int J Public Health. 2014;59:999–1009. doi: 10.1007/s00038-014-0602-6. [DOI] [PubMed] [Google Scholar]
- 19.Logan AG. Hypertension in aging patients. Expert Rev Cardiovasc Ther. 2011;9:113–20. doi: 10.1586/erc.10.171. [DOI] [PubMed] [Google Scholar]
- 20.Re RN. Obesity-related hypertension. Ochsner J. 2009;9:133–6. [PMC free article] [PubMed] [Google Scholar]
- 21.Ostovar A, Vahdat K, Raiesi A, Purbehi M, Darabi H, Khajehian MM, et al. Hypertension risk and conventional risk factors in a prospective cohort study in Iran: The persian gulf healthy heart study. Int J Cardiol. 2014;172:620–1. doi: 10.1016/j.ijcard.2014.01.080. [DOI] [PubMed] [Google Scholar]
- 22.Do HT, Geleijnse JM, Le MB, Kok FJ, Feskens EJ. National prevalence and associated risk factors of hypertension and prehypertension among vietnamese adults. Am J Hypertens. 2015;28:89–97. doi: 10.1093/ajh/hpu092. [DOI] [PubMed] [Google Scholar]


