Abstract
Aims and Objective:
To find out and compare peri implant strain developed in four different types of implant supported prostheses i.e., cement retained splinted, cement retained non splinted, screw retained splinted, screw retained non splinted.
Methodology:
Four implant analogues were placed in a polyurethane mandibular model at the position of left and right first and second molar. Abutments were fixed to the implant at a torque of 25Ncm. Two such models were made. Four different prostheses were placed on abutment of each model i.e screw retained splinted, screw retained nonsplinted, cement retained splinted, cement retained non splinted. Four strain gauges were attached on the model, two on the buccal and two on the lingual aspect of each implant. Static load of 400N was applied on the prosthesis using universal testing machine. Load application was done ten times for each model and peri implant strain was measured.
Results:
The mean peri implant strain (±SD) generated was found to be highest in non-splinted screw retained (1397.70 ± 44.47 microstrains and 1265.90 ± 42.76 microstrains) and least in splinted cement retained (630.70 ± 31.98 microstrains and 519.60 ± 32.48 microstrains) in both 1st and 2nd molars respectively.
Conclusions:
Splinted crowns produce less peri implant strain when compared to non splinted crowns. Cement retained prosthesis produce less peri implant strain when compared to screw retained prosthesis. Least strain was observed in cement retained splinted crowns.
Keywords: Cement retained, non splinted, peri implant strain, screw retained, splinted
INTRODUCTION
Implant supported prosthesis provides the best form of functional and aesthetic replacement for missing teeth. Implant supported prosthesis have achieved popularity and also have become the standard of care. A lot of optimization has happened in the selection of materials, design and the related techniques.[1] Clinical implant prosthodontics presently focuses on the prognostification of individual and splinted crowns, as well as cemented and screw retained crowns. Specific superiority of each is not explored in detail, especially in the strain profile.
Minimum peri-implant strain is one of the criteria for long term survival of any implant prosthesis. Peri-implant strain more than 4000 microstrain leads to pathologic fracture of the bone.[2] Therefore, while selecting the type of prosthesis for a given clinical situation, along with the esthetics and function, peri implant strain generated in the surrounding bone should also be considered to ensure the long term success of the prosthesis.[3]
Occlusal overload is a primary factor for generation of peri implant strain, peri implant bone loss as well as loss of implant supported prosthesis.[4] Transfer of occlusal load is related to several factors one of which is type of prosthesis (splinted or non splinted) and the type of retention. Compared to implant-supported total fixed prostheses, implant-supported partial fixed prostheses are more susceptible to the moment generated by occlusal loads, since they lack the benefit of cross-arch stabilization.[4]
The implant supported prosthesis can be broadly classified into screw retained and cement retained.[5] In the case of multiple implants, both splinted and non splinted prosthesis designs have been used. Theoretically, splinting of crowns show better distribution of occlusal loads between the implants and thereby reduces the peri-implant strain.[6] Well distributed forces reduces potential overloading of crestal bone which may lead to loosening of prosthesis, implant fractures and eventually implant failure.[7] However splinted prosthesis is not always preferred for reasons of constraints experienced in the maintenance of hygiene.[8]
The decision whether or not to splint adjacent implants in partially edentulous situation has diversified opinion amongst the clinicians. Investigators have studied this question with various methods including finite element analysis, photoelastic model analysis and clinical investigations.[6] However, there remains no consensus regarding which prosthetic design (splinted or non-splinted) is superior.
The purpose of this study was to find out and compare peri implant strain developed in four different types of prosthesis cement retained splinted, cement retained non splinted, screw retained splinted, screw retained non splinted. The null hypothesis for this study was that there is no difference in the peri implant strain generated in four different types of implant supported prostheses.
METHODOLOGY
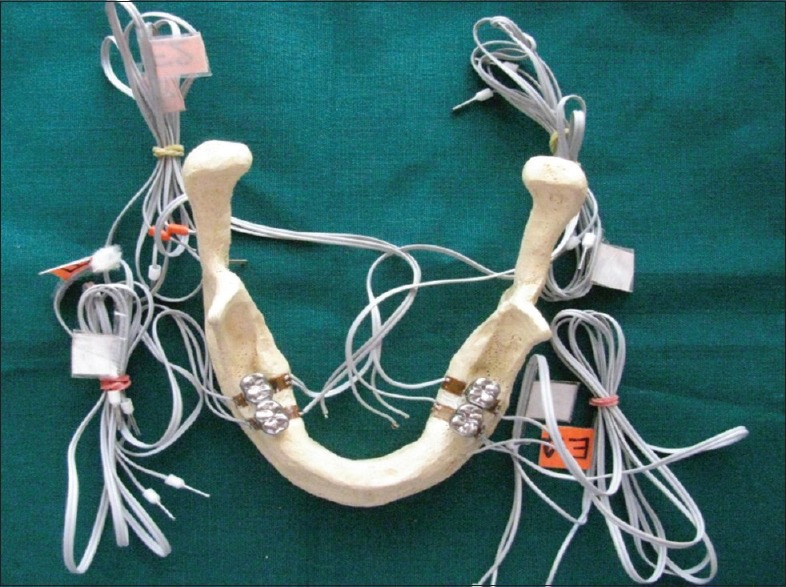
In a polyurethane mandibular model (soft, Polyol: diisocyanate 1:1) four implant analogs (Make it simple (MIS), wide (3.75 mm × 11 mm,) were placed at the position of first and second molar (Tooth number 36,37,46,47) [Figure 1].[9] First and second molar region was selected for implant placement as maximum occlusal forces act on the posterior part of the ridge and therefore maximum peri implant strain is generated in that region of the arch.[10] The distance between the two analogs was 10 mm. Strain gauges (unitec automation, reistance 350 ohms, length 3 mm, factor 2.01) were attached on the buccal and lingual side of each implant on both the models for the measurement of peri implant strain [Figure 2].[4]
Figure 1.

Polyurethane mandibular model with implants and abutments
Figure 2.

Polyurethane mandibular model with strain gauges
Strain gauge analysis is a technique for measuring microstrains, which involves the use of electrical resistance or strain gauges.[11] Strain gauges are based on the principle that certain materials undergo changes in their electrical resistivity when subjected to a force. Materials have different resistivities, which can be measured accurately at the site where the strain gauge is attached, using a Wheatstone's bridge circuit. This technique has been proposed to evaluate strains in implant-supported prostheses in vitro, in vivo and under static and/or dynamic loads.[11]
Two such models were made. One model was prepared for cement retained prosthesis and the other was prepared for screw retained prosthesis. Regular abutments (3.75 mm × 6 mm) were fixed on the implants for cement retained prosthesis and UCLA abutments (3.75 mm × 6 mm) were fixed on the implants for screw retained prosthesis[9]. University of California, Los Angeles (UCLA) is a prefabricated abutment made up of plastic like material. Plastic can be burnt out and casted with any alloy making a provision for prosthetic screw of the screw retained prosthesis and also providing a passive fit to the prostheses. All the abutments were screw tightened at the torque of 25 Ncm. Four different types of prosthesis were fabricated; Screw retained splinted, screw retained individual, cement retained splinted, cement retained individual.
For the fabrication of cement retained prostheses, closed tray impression technique was used. Impression was poured with die stone material and a working die was fabricated. The wax patterns were invested and wax burn out was done. The casting was completed using nickel chromium alloy. For the non splinted crowns wax pattern was fabricated for 1st and 2nd molar separately whereas for splinted crowns the wax pattern for 1st and 2nd molar was made as a single unit [Figures 3 and 4].
Figure 3.

Nonsplinted crowns
Figure 4.

Splinted crowns
For the fabrication of screw retained prostheses, wax pattern was directly fabricated around the UCLA abutment on the model.[12] For the non splinted crowns wax pattern was fabricated for 1st and 2nd molar separately whereas for splinted crowns the wax pattern for 1st and 2nd molar was made as a single unit. The wax patterns along with UCLA abutment were invested and wax burn out was done. The casting was completed using nickel chromium alloy. On both the models, splinted crowns were placed at the position of 36,37 and individual crowns were placed at the position of 46,47 [Figures 5 and 6]. Zinc polycarbonate cement was used for the luting of cement retained prostheses.
Figure 5.
Model with splinted and nonsplinted cement-retained crown
Figure 6.

Model with splinted and nonsplinted screw-retained crown
A metal jig was fabricated to ensure simultaneous load application at the central fossae region of both the crowns. The jig was attached to the universal testing machine. A static load of 400 N was applied on each prosthesis for a period of 10 seconds using universal testing machine [Figures 7 and 8].[4] The load of 400 N was selected because in healthy, dentulous subjects, the total occlusal force in the molar region at maximum clenching strength was reported to be 400 N.[13,14,15,16] Load application was done ten times for each model and peri implant strain was measured in each strain gauge.
Figure 7.

Load application on the crowns using universal testing machine
Figure 8.

Load application on the crowns using universal testing machine
Statistical analysis
The Mean peri implant strain with four prostheses was compared using one way analysis of variance (ANOVA) technique adjusted for multiple comparisons using Tukey's method. P value less than 0.05 was considered to be statistically significant.
There was a statistically significant difference in mean peri implant strain between groups in first molar as determined by one-way ANOVA (F = 488.01, P = <0.001).
The mean strain with Non splinted cement (779.0 ± 51.27 Microstrains) was significantly lower compared to Splinted screw retained (1189.2 ± 68.79 Microstrains, P < 0.005) and Non Splinted screw retained prostheses (1397.7 ± 44.47 Microstrains, P < 0.005) [Tables 1 and 2].
Table 1.
Peri-implant strain in splinted cement-retained prosthesis (microstrain)
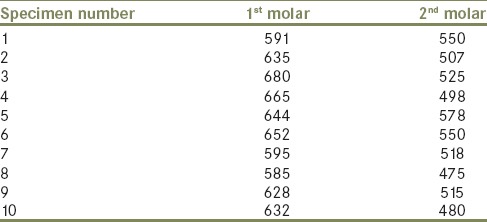
Table 2.
Peri-implant strain in nonsplinted cement-retained prosthesis (microstrain)
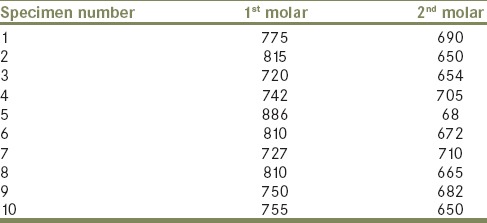
Mean strain with Splinted screw retained (1189.2 ± 68.79 Microstrains) was significantly lower compared to Non Splinted screw retained prosthesis (1397.7 ± 44.47 Microstrains, P < 0.005) [Tables 3–5] [Figure 9].
Table 3.
Peri-implant strain in splinted screw-retained prosthesis (microstrain)
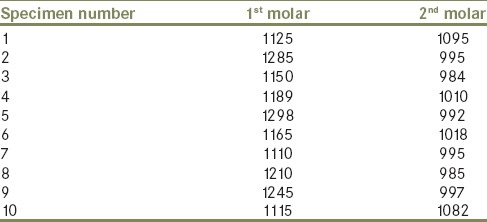
Table 5.
Mean peri-implant strain developed in first molar with four different types of prostheses (microstrains)

Figure 9.
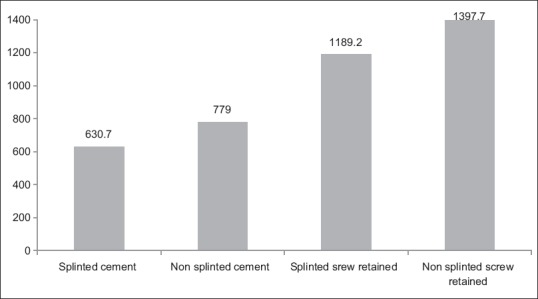
Mean peri-implant strain developed in the first molar with four different types of prostheses
Table 4.
Peri-implant strain in nonsplinted screw-retained prosthesis (microstrain)

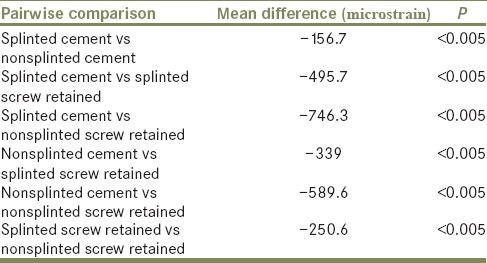
A Tukey post-hoc test revealed that mean peri implant strain in First molar was significantly lower with Splinted cement prostheses (630.7 ± 31.98 Microstrains) when compared to that with Non splinted cement (779.0 ± 51.27 Microstrains, P < 0.005) Splinted screw retained (1189.2 ± 68.79, P < 0.005) and Non Splinted screw retained prostheses (1397.7 ± 44.47 Microstrains, P < 0.005) [Table 6].
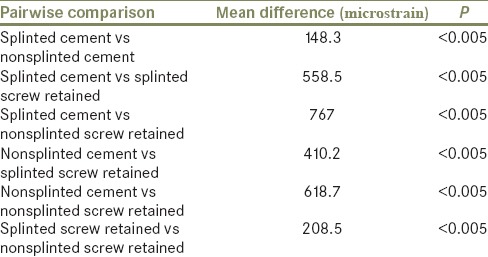
Table 6.
Post hoc pairwise comparison (Tukey's Honestly Significant Difference)
There was a statistically significant difference in mean peri implant strain between groups in Second molar as determined by one-way ANOVA (F = 908.44, P = <0.001).
The mean strain with Non splinted cement (676.3 ± 21.81 Microstrains) was significantly lower compared to Splinted screw retained (1015.3 ± 40.05 Microstrains, P < 0.005) and Non Splinted screw retained prostheses (1265.9 ± 42.76 Microstrains, P < 0.005) [Table 7] [Figure 10].
Table 7.
Mean peri-implant strain developed in the second molar with four different types of prostheses (microstrain)
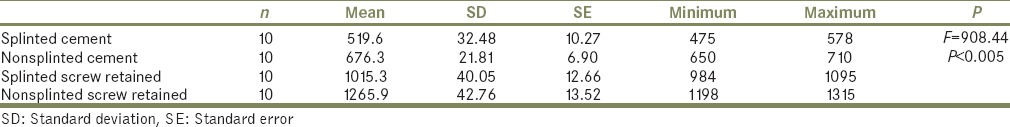
Figure 10.
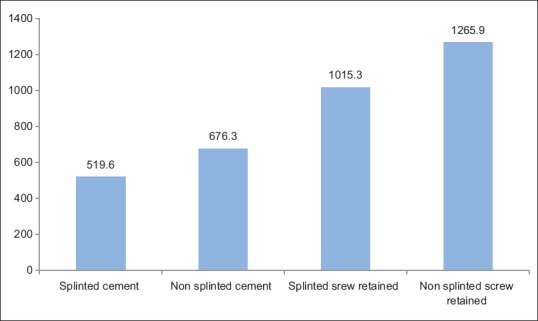
Mean peri-implant strain developed in the second molar with four different types of prostheses
In addition mean strain with Splinted screw retained (1015.3 ± 40.05 Microstrains) was significantly lower compared to Non Splinted screw retained prosthesis (1265.9 ± 42.76 Microstrains, P < 0.005). [Table 7] [Figure 10].
A Tukey post-hoc test revealed that mean peri implant strain in Second molar was significantly lower with Splinted cement prostheses (519.6 ± 32.48 Microstrains) when compared to that with Non splinted cement (676.3 ± 21.81 Microstrains, P < 0.005) Splinted screw retained (1015.3 ± 40.05 Microstrains, P < 0.005) and Non Splinted screw retained prostheses (1265.9 ± 42.76 Microstrains, P < 0.005) [Table 8].
Table 8.
Post hoc pairwise comparison (Tukey's Honestly Significant Difference)
DISCUSSION
Peri implant strain is the deformation in the bone around the implant in response to occlusal forces acting on the implant supported prosthesis.[3] According to Vasconcellos et al. when an occlusal load is applied on an implant supported prostheses, the load is partially transferred to bone, with the highest stress occurring in the peri-implant area.[4] Therefore, the cervical region of implant is the site where the greatest micro deformation occurs, and this is independent of the type of bone, the design of implant, the configuration of prosthesis and the type of load applied.[4] Himmlova et al. stated that bone strain above 3000 microstrains may be unfavourable for the bone leading to a hypertrophic response and bone strain above 4000 microstrains may cause overloading followed by bone loss.[17] The need for this study was to develop a clinical approach in selection of prosthesis design to reduce the stresses induced on the bone surrounding the implant, as these stresses on exceeding the physiological limit of the bone can cause crestal bone loss and loss of osseointegration. In the present study four implant analogues were placed in a polyurethane mandibular model at the position of left and right first and second molar.[10] Abutments were fixed to the implants at a torque of 25Ncm. Two such models were made. Four different prostheses were placed on abutment of each model i.e screw retained splinted, screw retained nonsplinted, cement retained splinted, cement retained non splinted. Four strain gauges were attached on the model, two on the buccal and two on the lingual aspect of each implant. Static load of 400N was applied on the prosthesis using universal testing machine.[13,14,15,16] Load application was done ten times for each model and peri implant strain was measured. Hence the objective of this study was to find out compare the peri implant strain in four different types of prosthesis i.e., splinted cement retained, non splinted cement retained, splinted screw retained, non splinted screw retained.
The mean peri implant strain (±SD) generated was found to be highest in non-splinted screw retained (1397.70 ± 44.47 microstrains and 1265.90 ± 42.76 microstrains) and least in splinted cement retained (630.70 ± 31.98 microstrains and 519.60 ± 32.48 microstrains) in both 1st and 2nd molars respectively. The result of the present study concided with the result of an in vitro study conducted by Yilmaz B et al. who evaluated the peri implant strain generated by splinted and non splinted cement retained implant crowns for two implants. The result showed less peri implant strain in splinted crowns when compared to non splinted crowns but the difference was found to be statistically insignificant.[6] In another study conducted by Yilmaz B et al. where the authors evaluated the peri implant strain for splinted and non splinted screw retained crowns on short implants it was concluded that splinting short implants may provide a more even strain distribution during functional loading.[18] Similar results were obtained by Nissan J et al., the results showed mean strain of 756.32 microstrains and 186.12 microstrains in non splinted and splinted cement retained prosthesis respectively.[5] Shigemitsu R et al. conducted a finite element analysis with invivo loading data and the results showed that splinted implant reduced stress in peri implant bone when compared to non splinted implants.[19] Koller et al. evaluated retrospectively the association among occlusal, periodontal and implant-prosthetic parameters and marginal bone loss (MBL) around implants after prosthetic loading. They concluded that inadequate occlusal pattern guide, presence of visible plaque, and cemented and splinted implant-supported restoration were associated with greater MBL around the implant.[20]
Based on results of this study, the null hypothesis was rejected. It was recommened to splint adjacent implants together wherever possible for the following reasons- Splinting improves force distribution around peri-implant bone which decreases the chance for microfractures and progressive bone resorption.[2] Splinted implant supported prosthesis may be retrieved, modified and salvaged in the event a non-strategic implant is lost in the future.[7] This benefits the patient with improved comfort and function in the event of an implant failure. Splinting implants together allows for long span prosthesis to be supported by fewer strategically placed implants, which is a financial benefit for the patient.[1]
CONCLUSIONS
Within the limitations of this study to replicate osseointegration, occlusal forces and modulus of elasticity of mandibular bone the results suggest that splinted crowns produce less peri implant strain when compared to non splinted crowns irrespective of type of retention of prostheses (cement or screw retained) and the mean difference was statistically significant. Cement retained prosthesis produce less peri implant strain when compared to screw retained prosthesis and the mean difference is statistically significant. Least strain was observed in cement retained splinted crowns. There is need to further evaluate the peri implant strain under oblique and cyclic loading. Also influence of different types of prosthetic materials should be evaluated on peri implant strain. Prospective clinical studies are needed to determine whether splinting implant supported crowns affects the clinical outcome.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Peri- implant mucositis and peri- implantitis: A current understanding of their diagnosis and clinical implication. J Periodontol. 2013;84(4):436–43. doi: 10.1902/jop.2013.134001. [DOI] [PubMed] [Google Scholar]
- 2.Vidyasagar L, Apse P. Biological response to dental implant loading\overloading. Implant overloading: Empiricism or science? Stomatologijia, Baltic dental and maxillofacial journal. 2003;5:83–9. [Google Scholar]
- 3.Misch C E. 3rd edition. india: Elsevier publishing; 2008. Dental implant prosthetics. [Google Scholar]
- 4.Vasconcellos L G O, Nishioka R S, Vasconcellos L M R, Nishioka L N B M. effect of axial loads on implant supported partial fixed prosthjesis by strain gauge analysis. J Appl Oral Sci. 2011;19(6):610–5. doi: 10.1590/S1678-77572011000600011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nissan J, Ghelfano O, Gross M, Chaushu G. Analysis of load transfer and stress distribution by splinted and unsplinted implant supported fixed cemented restorations. J oral rehab. 2010;37(9):101–222. doi: 10.1111/j.1365-2842.2010.02096.x. [DOI] [PubMed] [Google Scholar]
- 6.Yilmaz B, Mess J, Seidt J, Clelland N L. Strain comparision for splinted and non splinted cement retained implant crowns. Int J prosthodont. 2013;26(3):235–8. doi: 10.11607/ijp.3254. [DOI] [PubMed] [Google Scholar]
- 7.Bakke M. bite force and occlusion. Semin ortho. 2006;12:120–6. [Google Scholar]
- 8.Lindhe J, Meyle J. Peri-implant disease: Consensus report of the sixth European workshop on periodontology. J clin periodontal. 2008;35:282–5. doi: 10.1111/j.1600-051X.2008.01283.x. [DOI] [PubMed] [Google Scholar]
- 9.Goiato M C, Pesqueria A A, Santos D M D, Haddad M F, Moreno A. Photoelastic stress analysis in prosthetic implants of different diameter: Mini, narrow, standard, wide. Journal of clinical and diagnostic research. 2014;8(9):86–90. doi: 10.7860/JCDR/2014/8489.4902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Koc D, Dogan A, Bek B. Bite force and influential factors on bite force measurement: A literature review. Eur J dent. 2010;4:223–32. [PMC free article] [PubMed] [Google Scholar]
- 11.Nishioka R S, Vasconcellos L G O D, Soias R P, Rode S D M. Load application device: A comparative strain gauge analysis. Braz Dent J. 2015;23(3):220–5. doi: 10.1590/0103-6440201300321. [DOI] [PubMed] [Google Scholar]
- 12.Modi R, Mittal R, Kohli S, Singh A, Sefa I. Screw versus cement retained prosthesis: A review. Int J of advanced health sci. 2014;1(6):26–32. [Google Scholar]
- 13.Biswas BK, Bag S, Pal S. Biomechanical analysis of normal and implanted tooth using biting force measurement. Int J of eng and app sci. 2013;4(2):17–23. [Google Scholar]
- 14.Chio D S, Cha B K, Jang I, Kang KH, Kin SC. Three dimensional finite element analysis of occlusal stress distribution in human skull with premolar extraction. Angle orthod. 2013;83:204–11. doi: 10.2319/020112-89.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Okada y, Sato Y, Kitagawa N, Uchida K, Osawa T, Imamura Y, Terazawa M. Occlusal status of implant superstructure at mandibular first molar immediately after setting. Int J of imp dent. 2015;1(6):3–9. doi: 10.1186/s40729-015-0016-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kayumi S, Takayama Y, Yokoyama A, Ueda N. Effect of bite force in occlusal adjustment of dental implant on the distribution of occlusal pressure: Comparision among three bite forces in occlusal adjustment. Int J of Imp dentistry. 2015;1(14):120–6. doi: 10.1186/s40729-015-0014-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Himmlova L, Dostalova T, Kacovsky A, Konvickova S. Influence of implant length and diameter on stress distribution: A finite element analysis: A finite element analysis. J Prosthet Dent. 2004;91:20–5. doi: 10.1016/j.prosdent.2003.08.008. [DOI] [PubMed] [Google Scholar]
- 18.Yilmaz B, Seidt J, Mc Glumphy E A, Clelland N L. Comparision of strain for splinted and non splinted screw retained prostheses on short implants. Int J oral maxillofac implant. 2011;26(6):1176–82. [PubMed] [Google Scholar]
- 19.Shigemitsu R, Ogawa T, Matsumoto T, Yoda N, Gunji Y, Yamakawa Y, et al. Stress distribution in the peri implant bone with splinted and non splinted implants by in vivo loading data based finite elements analysis. Odontology. 2013:101–222. doi: 10.1007/s10266-012-0077-y. [DOI] [PubMed] [Google Scholar]
- 20.Koller C D, Cenci T P, Boscato N. Parameters associated with marginal bone loss around implant after prosthetic loading. Braz Dent J. 2016;27(3):115–9. doi: 10.1590/0103-6440201600874. [DOI] [PubMed] [Google Scholar]


