Abstract
Objective
The aim of this study was to examine the challenges confronting surgeons performing basic science research in today’s academic surgery environment.
Summary of Background Data
Multiple studies have identified challenges confronting surgeon-scientists and impacting their ability to be successful. Although these threats have been known for decades, the downward trend in the number of successful surgeon-scientists continues. Clinical demands, funding challenges, and other factors play important roles, but a rigorous analysis of academic surgeons and their experiences regarding these issues has not previously been performed.
Methods
An online survey was distributed to 2504 members of the Association for Academic Surgery and Society of University Surgeons to determine factors impacting success. Survey results were subjected to statistical analyses. We also reviewed publicly available data regarding funding from the National Institutes of Health (NIH).
Results
NIH data revealed a 27% decline in the proportion of NIH funding to surgical departments relative to total NIH funding from 2007 to 2014. A total of 1033 (41%) members responded to our survey, making this the largest survey of academic surgeons to date. Surgeons most often cited the following factors as major impediments to pursuing basic investigation: pressure to be clinically productive, excessive administrative responsibilities, difficulty obtaining extramural funding, and desire for work-life balance. Surprisingly, a majority (68%) did not believe surgeons can be successful basic scientists in today’s environment, including departmental leadership.
Conclusions
We have identified important barriers that confront academic surgeons pursuing basic research and a perception that success in basic science may no longer be achievable. These barriers need to be addressed to ensure the continued development of future surgeon-scientists.
Keywords: academic surgery, basic science, surgeon-scientist, translational research
Surgeons have a long legacy of important contributions in basic and translational research, and advancing the fundamental understanding of surgical diseases remains a priority in academic surgery.1 However, despite the importance of basic investigation, academic surgeons are expected to participate in clinical care, administrative duties, education, and mentoring. Those who wish to develop a successful research career must also manage laboratory personnel, write manuscripts, obtain funding, and mentor students and fellows. When added to the importance of achieving work-life balance, the challenges facing surgeon-scientists are seemingly insurmountable. Recent pressures have compounded these challenges, including increased difficulty obtaining federal funding, mounting administrative burden, and ever-growing pressure for clinical productivity.2 It is not surprising that evidence suggests that the continued existence and development of surgeon-scientists is threatened.
Several studies have noted that surgeon-scientists have been falling behind in basic research compared to other disciplines in medicine. Examining National Institutes of Health (NIH) funding from 1995 to 2001 to the 5 most active clinical departments at US medical schools, Rangel et al3 found that success rates for surgical proposals were significantly lower than for the other departments for all years studied. A similar study of NIH funding from 1982 to 2004 showed that although total grant applications to NIH increased by 124% during that period, applications from surgical departments increased by only 67%.4 Commensurate with this, total NIH awards went up by 71%, but surgical awards increased only by 41%. Looking specifically at the pipeline of surgeon-scientists, Rangel and Moss5 compared funding success for career development K-awards between surgical and nonsurgical faculty. Non-surgeons were 2.5 fold more likely to apply for a K-award, and significantly more likely to receive one. Departments of surgery also fare poorly compared to nonsurgical departments with respect to funding from other agencies, such as the American Cancer Society.6
Motivated by the uncertain future of basic science in surgery, this study was designed to identify challenges confronting surgeon-scientists to inform academic leaders and to define opportunities for improving the success of the future academic surgical workforce. With over 1000 academic surgeons and trainees responding, this study represents the largest survey to date addressing this important question regarding the future of academic surgery.
METHODS
Data from Blue Ridge Institute for Medical Research were gathered regarding NIH funding at surgical departments in the top 25 funded institutions from 2006 to 2014. Additionally, the number of total and basic science abstracts submitted to the Academic Surgical Congress (ASC) annual meeting was determined for 2011 to 2015.
Survey and Sample Population
A questionnaire was developed to obtain demographic data, assess perceptions regarding challenges facing surgeon-scientists, and address potential barriers to research productivity. Survey topics included the funding environment, perceptions about basic research, external factors impacting ability to pursue research, training, mentorship, and protected time. The questions were developed by a group of 5 active and experienced surgeon-scientists, and validated for clarity, content, and adequacy through a presurvey test on a group of 8 surgeon-scientists representing each of the 4 subgroups (trainees, junior faculty, senior faculty, and chairman/division chiefs). The survey was distributed via e-mail on January 30, 2015 to 2504 members of the Association of Academic Surgery (AAS) and the Society of University Surgeons (SUS). Data were collected anonymously through SurveyMonkey until April, 2015. The expected response rate was approximately 50% based on past surveys. However, we recognized that there is no scientifically proven minimally acceptable response rate, and the surveys were more focused on obtaining a representative sample. Identifiable information was omitted to ensure anonymity. Seniority of respondents was categorized as follows: trainee (medical student, resident, fellow), junior faculty (1–5 years post-training), senior faculty (>5 years post-training), and division chief or department chair.
Statistical Analysis
Filter and compare rules were used to identify subsets of the population. Filter rules allow data analysis for a group based on defined criteria. Compare rules are a joint distribution between 2 discrete variables, for example, participants conducting basic versus clinical research. SurveyMonkey has a feature that determines statistically significant differences between response groups when the compare rule is applied to a survey question. Raw data were exported Microsoft Excel, and Student t test and N-1 Two Proportion test were used for statistical analysis, with significance defined as P < 0.05. Trainees were excluded, unless specified.
RESULTS
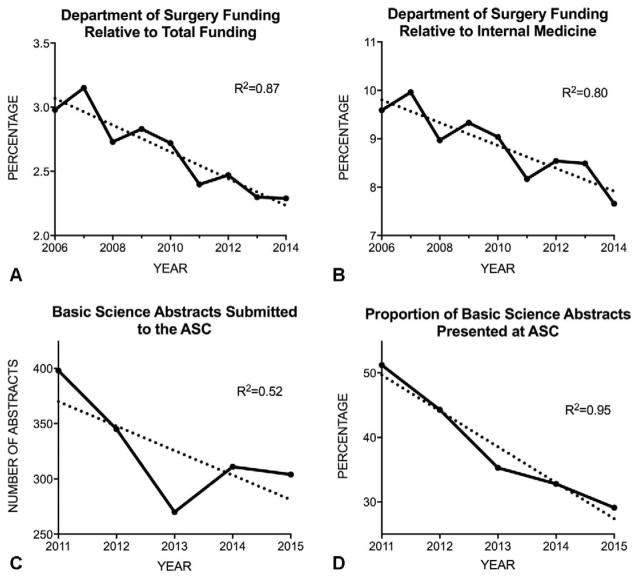
Blue Ridge Institute for Medical Research compiles data from NIH on funding to US medical schools and their departments (www.brimr.org). Annual NIH funding to surgery departments was compared to total NIH funding from 2006 to 2014. In 2006, 3.0% of NIH funding to the 25 top-funded institutions went to their surgery departments. This proportion decreased to just 2.3% in 2014 (Fig. 1A), a 23% linear decline (R2 = 0.87; Fig. 1A). The absolute amount of funding to surgical departments over that period declined from $185,418,928 in 2006 to $157,808,838 in 2014. In contrast, total NIH funding increased from $6,223,850,681 to $6,882,730,545 over the same period. A similar trend was observed when surgery funding was compared to departments of medicine. Surgery departments had 9.6% of the level of funding of medicine departments in 2006, and this decreased to 7.7% in 2014 (Fig. 1B), a drop of 20%, again in a linear fashion (R2 = 0.80).
FIGURE 1.
Steady decline in National Institutes of Health (NIH) funding of surgical research and in the prevalence of basic science in academic surgery. NIH award data for fiscal years 2006 to 2014 were obtained from the Blue Ridge Institute for Medical Research. Values include direct and indirect costs, but exclude research and development contracts. Values represent the top 25 US medical schools that receive the most NIH funding. Departments of Surgery funding relative to total institutional funding (A) and to Departments of Medicine (B) are shown. The number of basic science abstracts submitted to the ASC from 2011 to 2015 is shown (C), as well as the proportion of accepted basic science abstracts relative to all abstracts presented each year (D). Values are presented as percentages for (A), (B), and (D), as well as the number of abstracts in (C).
We analyzed data on the number of abstracts presented at the annual ASC from 2011 to 2015. In 2011, 832 abstracts were submitted, with 398 categorized as basic science. By comparison, 1128 total abstracts were submitted to the 2015 conference, of which 304 were basic science (Fig. 1C). Thus, despite a 36% increase in the total number of abstracts, there was a 24% drop in the basic science abstracts. We also identified a significant decline in the proportion of presented abstracts classified as basic science, with the percentage dropping from 51% in 2011 to 29% in 2015 (Fig. 1D; R2 = 0.95). These data reveal a significant decline in the absolute number of basic science abstracts submitted and in the proportion presented at this academic surgical meeting. Although these results reflect trends only at the ASC, when combined with the Blue Ridge Institute for Medical Research data above, the evidence suggests a national decline in basic research by surgeons.
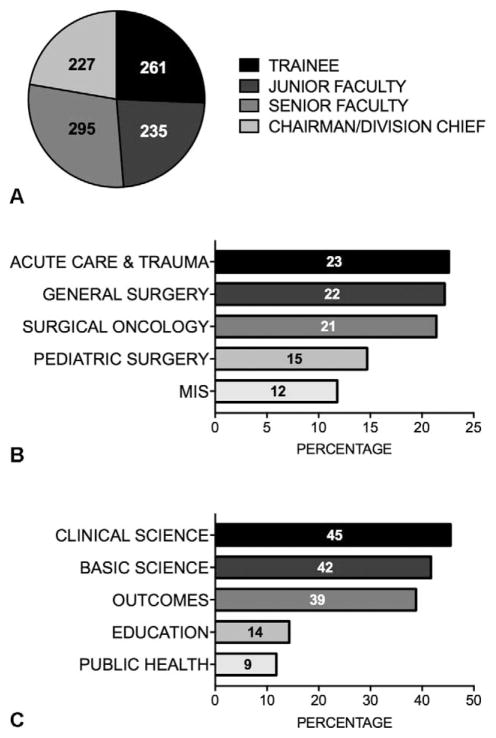
To understand the factors negatively impacting basic science in surgery, we conducted a survey of the AAS and SUS membership. Of the 2504 individuals who received the survey, 1033 (41.3%) academic surgeons responded, 6 (0.2%) opted out, 33 (1.3%) bounced back, and 1433 (57.2%) did not respond. The Northeast and Midwest had the highest reporting percentages with 303 (29%) and 289 (28%) responses, respectively. In total, 261 trainees (26%), 235 junior faculty (23%), 295 senior faculty (29%), and 227 division chiefs or department chairs (22%) completed the questionnaire (Fig. 2A). The most common specialties included acute care and trauma (23%), general (22%), oncology (21%), pediatrics (15%), and minimally invasive surgery (12%) (Fig. 2B). Of participants currently engaged in research, 45% indicated their primary research focus as clinical and 42% indicated basic science. Values are self-reported and individuals could choose >1 answer (Fig. 2C).
FIGURE 2.
Demographic characteristics of respondents. The career stage of respondents was classified as trainee, junior faculty (5 years or less out of training), senior faculty, or division/department chiefs (A). Values reflect absolute numbers for 1018 participants that answered the question “What is your current academic position?” Of note, 1033 respondents participated in this survey, but 15 individuals elected to skip this question. Faculty participants were classified based on their surgical specialty (B) and type of research performed (C). (B and C) Data shown represent reporting percentages of the 757 faculty members that participated in the survey.
Perceptions About Basic Science Research
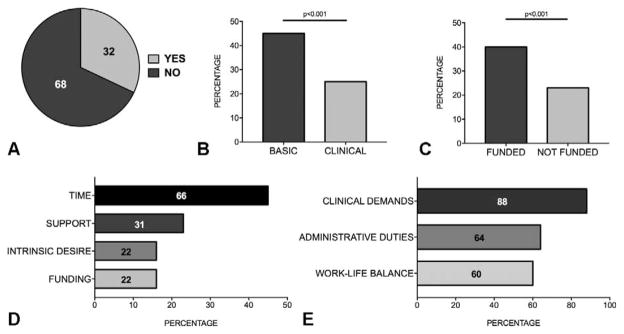
Respondents were asked whether they believe that it is realistic for surgeons to be successful in basic science in today’s environment. Only 32% of faculty answered “yes” (Fig. 3A). When the respondents were stratified by primary research focus, surgeons in basic science were more likely to hold this positive outlook as compared to clinical researchers (44% vs. 24%, P < 0.001; Fig. 3B). 5723%, P < 0.001; Fig. 3C). Analyzing only the basic science cohort, funded versus non-funded faculty responded positively in 47% versus 38%, though this did not reach statistical significance (not shown). Remarkably, analysis based on academic seniority revealed that only 35% of division/department chiefs responded that it is realistic to expect surgeons to succeed in basic research, with 29% of junior faculty responding positively.
FIGURE 3.
Perceptions and pressures reflect a negative outlook on the ability of surgeons to succeed in basic research. Survey participants were asked: “Do you believe it is realistic to expect surgeons to be successful basic scientists in today’s hospital environment?” Responses were tabulated for all faculty (A), those doing basic vs. clinical research (B), and those with and without funding (C). A total of 53 editorial comments were provided by the 130 basic researchers with extramural funding who answered “no” to this question, and their primary reasons are shown graphically in (D). Focusing on this specific subgroup, data were analyzed from the following 3 questions: “Do considerations around work-life balance impact your desire/commitment to pursue research?”, “Do excessive hospital administrative duties have an impact on your ability to do research?”, and “Do you feel pressure to be clinically productive and generate revenue, so much so that it impacts your ability to do research?” Values represent the percentage of that subgroup responding “yes” (E).
We specifically analyzed responses of those with extramurally funded basic science programs, as this reflects a successful cohort of investigators. Surprisingly, of 213 faculty in this category, 113 (53%) believe it is unrealistic for a surgeon to be successful in basic research. This group provided 47 comments to explain their response, and these fell into 4 common themes (Fig. 3D). The themes include (1) insufficient time, (2) inadequate departmental support, (3) poor intrinsic desire (ie, lack of motivation), and (4) difficulty in obtaining funding. Further analysis to determine the causes of pessimism among this subgroup was performed by analyzing their responses to questions regarding extrinsic pressures often cited as major challenges to surgeon-scientists. As shown in Figure 3E, a majority of this subgroup felt that the following factors represent the major barriers to success: work-life balance, administrative responsibilities, and clinical demands.
Among respondents, 57% felt that basic science research was a priority in their department. The percentage was greatest among surgeons conducting basic science as compared to clinical research (62% vs. 53%; P <0.05). Respondents with extramural funding were more likely to perceive basic science as a departmental priority compared to nonfunded respondents (65% vs. 47%; P < 0.001). Further stratified by academic position, 61% of division chiefs and chairs with funding responded that basic science was a priority, compared to 41% of senior leaders without funding (P < 0.005). Notably, division chiefs and department chairs (54%) were more likely to believe that the amount of basic science research carried out by their surgical department was too little compared to senior (47%; P = NS) and junior faculty (44%; P < 0.05).
Since junior faculty represents the future of academic surgery, we asked “What do you think is the number one reason junior faculty members have difficulty achieving extramural funding?” Perceptions were similar among basic and clinical researchers, with both groups identifying the funding environment as a major obstacle to success (35% for basic science vs. 32% for clinical research; P = NS). Both also cited excessive clinical demands as a major challenge, with clinical researchers pointing to this more often than their peers in basic science (47% vs. 40%; P < 0.05). Additionally, responses were stratified by academic position. Junior faculty most often cited the challenging funding environment (34%) and “excessive clinical demands or insufficient protected time” (44%).
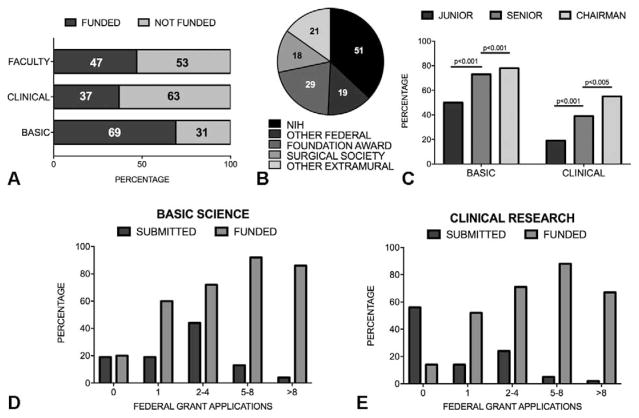
Funding Environment
Of all faculty participating in the survey (n = 757), 47% had extramural funding (Fig. 4A). The proportion of funded faculty was greater among basic scientists (69%) than among clinical researchers (37%) (Fig. 4A). Among faculty with extramural funding (n = 352), those conducting basic science comprised a significantly greater percent (61%) than those conducting clinical research (36%, P < 0.001). Among funded faculty conducting basic research, the sources of funding included NIH (51%), other federal sources (19%), foundations (29%), surgical societies (18%), and other extramural sources (21%) (Fig. 4B). Of note, the likelihood of having extramural funding for both basic and clinical investigators increased with seniority, as shown in Figure 4C.
FIGURE 4.
Extramural funding among academic surgeons. Faculty were asked “Do you currently have research funding awarded from outside your institution?” and the results are shown for all faculty and for the clinical and basic research subgroups (A). Sources of funding for basic researchers are shown in (B). Faculty with funding are stratified by basic vs. clinical research and by career stage, showing lower funding rates among younger faculty and consistently among clinical researchers (C). Respondents were asked “Approximately how many applications have you submitted for National Institutes of Health/federal funding in the last 3 years?” The response is shown by the dark bars, with the number of submissions along the x axis, and represents the percentage of respondents who submitted the specified number of grants. Submission number was correlated with a respondent’s funding status, shown by the light bars, which represent the proportion of individuals who are actively funded for each of the groups of grant submission numbers. The results are shown for both basic science (D) and clinical research (E).
We examined the correlation between the number of federal grant applications submitted by academic surgeons and the likelihood of achieving funding. The results are shown in Figure 4D (basic researchers) and Figure 4E (clinical investigators). The “submitted” bars on the graph represent the percentage of respondents (y axis) reporting that they submitted the indicated federal grants (x axis) over the past 3 years. The “funded” bars show the proportion of individuals in each group who are actively funded. For example, 4.2% of all basic scientists reported they had submitted >8 grants, and 85% of that cohort is funded. Among basic scientists, 81% had submitted a federal grant in the last 3 years, compared to 44% of clinical researchers (P <0.0001; Fig. 4D). For both groups, there was a significant correlation between the number of applications submitted and the likelihood of achieving extramural funding. Only 60% of basic researchers who reported submitting only 1 federal grant over the past 3 years were funded, as compared to 92% of those who submitted 5 to 8 grants (Fig. 4D). A similar trend was observed among clinical investigators (Fig. 4E). However, the number of surgeon-scientists who submitted ≥5 grant applications over a 3-year period was small, accounting for only 17% of basic scientists (Fig. 4D) and 7% of clinical researchers (Fig. 4E).
External Pressures
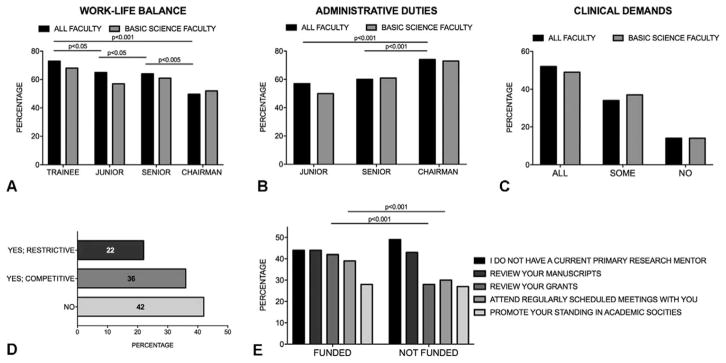
Multiple external pressures influence a surgeon’s likelihood of achieving a successful research career. Work-life balance, for example, was found to significantly impact their desire to pursue research (Fig. 5A). When stratified by academic position, the data show that 73% of trainees identify work-life balance as affecting their commitment to research. This was significantly higher than junior faculty (65%), senior faculty (64%), and division chiefs, and department chairs (50%; P < 0.05). Another factor impacting the ability of surgeons to conduct research is excessive administrative duties, as indicated by 62% of respondents, with a disproportionate influence on more senior surgeons (Fig. 5B). Although 74% of chiefs and chairs felt their research is adversely affected by administrative responsibilities, the numbers were significantly lower for senior faculty (60%) and junior faculty (57%; P < 0.001). Finally, the pressure to be clinically productive and generate revenue is felt by most surgeon-scientists. Of all academic faculty, 86% feel pressure either “all of the time” or “some of the time,” significantly impacting their ability to do research (Fig. 5C).
FIGURE 5.
External pressures impact academic surgeons’ desire and ability to pursue research in today’s environment. Faculty respondents were asked the following questions: “Do considerations around work-life balance impact your desire/commitment to pursue research?” (A); “Do excessive hospital administrative duties have an impact on your ability to do research?” (B); and “Do you feel pressure to be clinically productive and generate revenue, so much so that it impacts your ability to do research?” (C). In (C), responses include “Yes, ALL the time”, “Yes, but only SOMEtimes”, and “NO”, as shown in x axis. Values represent percentages responding affirmatively. Respondents were also asked whether the current National Institutes of Health (NIH) payline affects their interest in pursuing basic research (D). Options included “Yes, funding levels are so restrictive it is not worth submitting;” “Yes, but NIH funding has always been competitive and so you just have to try harder”; and “No, NIH paylines do not influence my decision to submit grants or do research.” The graph shows basic science faculty only. (E) To determine the relationship between mentoring and research funding, participants were asked to report activities of their primary research mentor, as shown in the figure. The responses are stratified by funding status and include trainees.
When queried “Is the current NIH pay line impacting your interest in pursuing basic science research?” 43% of all faculty responded “yes,” with 22% feeling that “funding levels are so restrictive that it is not worth submitting.” Among the 299 basic science faculty that responded to this question, 36% answered “Yes, but NIH funding has always been competitive and so you just have to try harder” (Fig. 5D), a perception more prevalent among basic scientists than among their peers in clinical research (36% vs. 16%; P < 0.0001).
Mentorship has been suggested to play an important role for young surgeon-scientists. We analyzed whether surgeons had mentors, their role as mentors, and whether a correlation could be identified between mentorship and success. Including trainees, 47% of participants did not have a current research mentor. This was more common among clinical researchers than basic scientists (56% vs. 37%; P < 0.001). Interestingly, although having a mentor did not predict funding success (Fig. 5E), several attributes of mentoring were more often reported by funded investigators (Fig. 5E), including meeting regularly with their mentor (39% vs. 30%; P < 0.001) and having a mentor who reviewed their grant applications (42% vs. 28%; P < 0.001).
Training
Over 74% of participants reported performing research as a surgical resident because they were confident they wanted to pursue an academic career, and 54% did it to enhance fellowship opportunities. When asked to identify their primary research focus as a resident, 66% reported basic science and 39% indicated clinical research. Younger respondents were significantly less likely to have conducted basic science as a resident than more senior surgeons. Division chiefs and department chairs (76%) and senior faculty (75%), for example, were significantly more likely to have conducted basic research as a surgical resident than junior faculty (60%) or trainees (53%; P < 0.001).
When faculty were asked about their first research environment after completing training, 26% said they started their own laboratory, 34% joined an established investigator, and 32% initiated a clinical research program. Interestingly, 64% of those who started their own laboratory currently have extramural funding, significantly more than those who joined an established investigator (48%) or initiated a clinical research effort (36%; P < 0.001). Interestingly, 57% of surgeon-scientists remained in a scientific field similar to their research as trainees, and this was more pronounced among basic researchers (72%) than clinical researchers (59%; P < 0.005). To gauge the overall perception about surgical trainees pursuing basic research, we found that the majority (64%) of faculty believe “basic research among surgical trainees should be limited to a select few residents with the ambition and talent to be successful in future research activities.” This response did not vary significantly among trainees (66%), junior faculty (65%), senior faculty (61%), and chiefs/chairs (68%), nor did it vary between basic (64%) and clinical (65%) investigators.
DISCUSSION
Over the past several decades, federal funding to surgeon-scientists has been lagging,3–6 and our analysis suggests that this trend continues. Compounded by the current funding environment and its impact on research productivity, the future of basic research in academic surgery may be threatened. As the cost associated with conducting basic research continues to grow, the competition to obtain funding from the NIH and other extramural sources has become progressively difficult. This is especially true when considering the steady decline in the NIH payline since 2003.7,8 The federal budget sequestration in 2013 had a significant impact on the NIH and other agencies funding biomedical research, requiring the NIH to cut its budget by 5% ($1.6 billion) in 2013. NIH Director Francis Collins stated, “I worry desperately this means we will lose a generation of young scientists.”9 The NIH budget increased by only $150 million (0.5%) in 2015, significantly less than the $606 million increase approved by the Senate spending committee and $211 million requested by the White House. This increase still resulted in a budget level below that in 2012.10 In fact, in inflation-adjusted dollars, the NIH budget is >22% below the 2003 level.8
We found a strong positive correlation between the number of grant proposals submitted and the rate of achieving extramural funding support. This is an important observation that needs to be emphasized to young surgeons seeking to establish successful research careers. Historically, surgeons have not applied as often as their nonsurgical peers.4,5,11 This likely contributes to the fact that only 46% of all faculty surveyed, and 69% of basic scientists, had extramural funding. Although “success” in basic research is difficult to define, we use federal funding as a proxy, but accept that alternative revenue sources (private industry, philanthropy, clinical revenue) can sustain productive basic research programs. Nevertheless, achieving peer-reviewed federal funding is commonly accepted as indicative of a successful research effort. Based on this metric, and the data presented here and previously by others, surgeon-basic scientists are falling behind and the future of this important aspect of academic surgery is uncertain.
Recognizing that multiple challenges confront surgeon-scientists, the SUS formed a Basic Science Committee tasked with identifying the issues facing surgical investigators to inform potential solutions. Established in 1938, the SUS is one of the premier organizations dedicated to the advancement of the surgical sciences. Its members have held an essential role in the development of modern surgery, contributing scientific breakthroughs and technological advances.12 Formed in 1966 with a similar mission, the AAS promotes a vision of research and academic pursuits through the exchange of ideas between surgical residents, junior faculty, and established academic surgeons.13 The ASC is the annual academic meeting jointly sponsored by these 2 organizations, representing the largest cohort of academic surgeons in North America. Two previous studies surveyed academic surgeons on the topic of surgeon-scientists. Ko et al (2000)14 invited 850 senior members of the AAS, SUS, and the American Surgical Association to complete a questionnaire, achieving a 44% response rate. In this survey, conducted over 15 years ago, academic surgeons believed that basic science research is a valuable pursuit. However, clinical and administrative responsibilities represented significant barriers to their research success. What was notably absent was the issue of research funding, a problem that has become much more pressing since that publication. The second study, by Chokshi et al (2009),12 sent an online survey to 1381 SUS members, with 23% responding. In this study, the authors again noted the burden of clinical activities, with participants spending at least twice as much time on clinical care than in research, partly because of the pressure to be financially productive. The present study adds important new information to this body of knowledge. It includes results from >1000 respondents, representing the largest survey to date focused on scientific research among surgeons. Furthermore, this survey gauges the perceptions of surgeons with regard to basic science research in light of growing clinical and financial pressures, mounting administrative burden, and importantly increasingly challenging national funding environment.
To formulate solutions to the challenges facing surgeon-scientists, identifying the external pressures that limit opportunities for success is a priority. These pressures impact a surgeon’s ability to succeed primarily by limiting the amount of time they can dedicate to their research. Pressure from department and hospital leadership to generate clinical revenue, often exacerbated by insufficient financial incentives for faculty to be academically productive, has previously been identified as one of the factors that adversely impact an investigator’s research effort.4,12,14,15 Increased administrative duties also impact research activities.4,6,12,14 We similarly found that surgeon-scientists feel that the pressure to be clinically productive and the burden of excessive administrative responsibilities both adversely affect their ability to be productive scientifically. We also identified a focus on the impact of basic research on work-life balance, especially among younger respondents, further limiting the time and motivation for research. Finally, the difficulty of obtaining funding has become a major impediment. These obstacles make basic/translational research increasingly difficult to pursue and ultimately cause not only current, but also aspiring, surgeon-scientists to question their motivation to pursue basic science.
One of the most surprising, and concerning, findings is that 68% of academic surgical faculty believe it is unrealistic for a surgeon to be a successful basic researcher. This is even more concerning when taking into consideration that this perception is prevalent even among those who consider themselves basic scientists. Furthermore, it is troubling that 65% of department leaders share this view. Changing this broad perception will be difficult without surgical chairmen/directors asserting the importance of basic investigation as integral to their programs.16 This negative perception may partly underlie the declining proportion of surgeons performing basic research during residency. Whereas 75% of division/department leaders did basic science during residency, only 60% of junior faculty and 53% of trainees did so. Given the finding that most academic surgeons remain in a research field similar to what they did during training, the decrease in basic research among our future surgeons and leaders is another reason for concern.
This study has several limitations owing to the nature of a survey and the inherent methodologic issues. There may have been potential bias in who responded. For example, 42% of respondents indicated basic science as their primary research focus, a relatively high proportion. Also, the responses are self-reported and therefore subject to variability and inconsistency. Nevertheless, this study reflects the opinions of a large cohort of academic surgeons and represents the prevailing perceptions and experiences of that group regarding critical barriers confronting surgeons pursuing basic/translational research. These barriers include the difficult funding environment, excessive clinical demands, and an overall belief that surgeons cannot succeed in basic science. Leaders in academic surgery need to be aware of these challenges so that an informed discussion can begin at the department, hospital, and national levels on how best to address them. Surgeon-scientists also need to do their part to enhance their likelihood of success. This includes increasing their frequency of grant applications and engaging more closely with appropriate mentors, both of which were found by our study to be associated with funding success; and both of which could be used as performance metrics by department leaders.
As mentioned above, the changing academic and hospital environment has contributed to a prevailing perception that it is unrealistic for surgeons to succeed as basic scientists, and may have surgeons wondering whether it is even worthwhile to maintain and develop links between basic science and surgery. If such attitudes permeate surgical leadership, it will influence the justification for making the investment required to encourage young faculty along a path toward basic science inquiry and research independence. Current models for surgical training need to be evaluated and possibly changed to develop surgeon-scientists prepared to succeed in today’s competitive scientific environment.17–19 If we agree that fundamental investigation into the pathophysiology and treatment of surgical disease needs to include the active participation of surgeons, then academic surgery must act to address these challenges and ensure the continued development of surgeon-scientists and an environment that promotes their success.
Acknowledgments
N.A. has grant funding from Astex and Cepheid Inc.
The authors are grateful to the members of the AAS and SUS who completed the survey.
Footnotes
Authors’ contributions: all authors approved the final manuscript; S.G.K., M.M., N.A., H.Z., and A.M.G. contributed to the conception, design, and data collection; C.M.M. performed data analysis; all authors contributed to data interpretation and writing and editing the manuscript.
The authors report no conflicts of interest.
References
- 1.Stein SL. Scholarship in academic surgery: history, challenges, and ideas for the future. Clin Colon Rectal Surg. 2013;26:207–211. doi: 10.1055/s-0033-1356718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rubio DM, Primack BA, Switzer GE, et al. A comprehensive career-success model for physician-scientists. Acad Med. 2011;86:1571–1576. doi: 10.1097/ACM.0b013e31823592fd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rangel SJ, Efron B, Moss RL. Recent trends in National Institutes of Health funding of surgical research. Ann Surg. 2002;236:277–287. doi: 10.1097/00000658-200209000-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mann M, Tendulkar A, Birger N, et al. National institutes of health funding for surgical research. Ann Surg. 2008;247:217–221. doi: 10.1097/SLA.0b013e3181568e26. [DOI] [PubMed] [Google Scholar]
- 5.Rangel SJ, Moss RL. Recent trends in the funding and utilization of NIH career development awards by surgical faculty. Surgery. 2004;136:232–239. doi: 10.1016/j.surg.2004.04.025. [DOI] [PubMed] [Google Scholar]
- 6.Wells SA. The surgical scientist. Ann Surg. 1996;224:239–254. doi: 10.1097/00000658-199609000-00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Garrison HH, Deschamps AM. NIH research funding and early career physician scientists: continuing challenges in the 21st century. FASEB J. 2014;28:1049–1058. doi: 10.1096/fj.13-241687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sequestration cuts biomedical research. [Accessed March 21, 2016];Federation of American Societies for Experimental Biology website. 2014 Available at: http://www.faseb.org/pdfviewer.aspx?loadthis=http%3A%2F%2Fwww.faseb.org%2FPortals%2F2%2FPDFs%2Fopa%2FSequestration%2520factsheet.pdf.
- 9.Vergano D. Science faces sequestration cuts. [Accessed March 20, 2016];USA Today web site. 2013 Feb 25; Available at: http://www.usatoday.com/story/tech/sciencefair/2013/02/25/budget-nih-collins/1947277/
- 10.Kaiser J. Within NIH’s flat 2015 budget, a few favorites. [Accessed March 20, 2016];Science Magazine website. 2014 Dec 10; Available at: http://www.sciencemag.org/news/2014/12/within-nih-s-flat-2015-budget-few-favorites.
- 11.Ratcliffe MB, Howard C, Mann M, et al. National Institutes of Health funding for cardiothoracic surgical research. J Thorac Cardiovasc Surg. 2008;136:392–397. doi: 10.1016/j.jtcvs.2008.04.009. [DOI] [PubMed] [Google Scholar]
- 12.Chokshi NK, Simeone DM, Chari RS, et al. A survey of academic surgeons: work, stress, and research. Surgery. 2009;146:462–468. doi: 10.1016/j.surg.2009.02.015. [DOI] [PubMed] [Google Scholar]
- 13.Donowitz M, Germino G, Cominelli F, et al. The attrition of young physician-scientists: problems and potential solutions. Gastroenterology. 2007;132:477–480. doi: 10.1053/j.gastro.2006.12.023. [DOI] [PubMed] [Google Scholar]
- 14.Ko CY, Whang EE, Longmire WP, Jr, et al. Improving the surgeon’s participation in research: is it a problem of training or priority? J Surg Res. 2000;91:5–8. doi: 10.1006/jsre.2000.5855. [DOI] [PubMed] [Google Scholar]
- 15.Homer-Vanniasinkam S, Tsui J. The continuing challenges of translational research: clinical-scientists’ perspective. Cardiol Res Pract. 2012;2012:246710. doi: 10.1155/2012/246710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Niederhuber JE. An old problem that may be getting worse (Editorial) Ann Surg. 2008;247:222–223. doi: 10.1097/SLA.0b013e318163ff78. [DOI] [PubMed] [Google Scholar]
- 17.Kirk AD, Feng S. Surgeons and research: talent, training, time, teachers and teams (Editorial) Am J Transplant. 2011;11:191–193. doi: 10.1111/j.1600-6143.2010.03399.x. [DOI] [PubMed] [Google Scholar]
- 18.Menger MD, Schilling MK, Schafers HJ, et al. How to ensure the survival of the surgeon-scientist? The Homburg Program. Langenbecks Arch Surg. 2012;397:619–622. doi: 10.1007/s00423-012-0925-9. [DOI] [PubMed] [Google Scholar]
- 19.Wan DC, Wang KC, Longaker MT. Training the contemporary surgeon-scientist (Editorial) Plast Reconstr Surg. 2012;129:1023–1025. doi: 10.1097/PRS.0b013e31824421e8. [DOI] [PubMed] [Google Scholar]