Abstract
The liver has marked regenerative capabilities, and numerous signaling pathways are involved in liver regeneration. The transforming growth factor-β (TGF-β)/Smad pathway, which is also involved in liver regeneration, regulates numerous biological processes. Krüppel-like factor 10 (KLF10) has been reported to activate the TGF-β/Smad signaling pathway; however, the exact functions of KLF10 under various pathophysiological conditions remain unclear. In the present study, the role of KLF10 in liver regeneration following partial hepatectomy (PH) was investigated using KLF10-knockout (KO) mice. KLF10-KO mice exhibited lower liver/body weight ratios and 5-bromo-2-deoxy-uridine labeling indices compared with wild-type (WT) mice, and significant differences (P=0.028) were obtained at 72 h after PH. To understand the causes of the gross and histopathological findings, the expression levels of the components of the TGF-β/Smad pathway were examined using reverse transcription-quantitative polymerase chain reaction and western blot analysis. The mRNA and protein levels of Smad3, p15, TGF-β1 and TGF-β receptor 1 were significantly increased, while those of cMyc and cyclin D1 (proliferation-associated genes) were significantly lower in the liver tissues of the KLF10-KO mice compared with those of the WT mice at 72 h post-PH. These results indicated that KLF10-KO may exhibit antiproliferative effects on liver regeneration following PH, through strengthening the TGF-β/Smad signaling pathway in a delayed manner.
Keywords: krüppel-like factor 10, liver regeneration, partial hepatectomy, proliferation, transforming growth factor-β/Smad pathway
Introduction
The liver has excellent regenerative capacities. Liver cells are quiescent under normal conditions; however, they enter the cell cycle when damaged and proliferate until the original liver volume is restored (1). A number of conditions may alter liver mass, including surgical resection, chemicals and pathogens (2–4). In the situation of liver cancer or hepatocirrhosis, surgical resection is a standard medical therapy. Cirrhosis of the liver is one of the leading causes of mortality, and liver cancer is the third most common cancer and the second leading cause of cancer-associated mortality worldwide (5,6).
Numerous signaling pathways are involved in liver regeneration, including pathways involving hepatocyte growth factor, epidermal growth factor, interleukin 6, tumor necrosis factor-α and transforming growth factor (TGF)-α and β (2,7). Among these, the TGF-β/Smad pathway is reported to suppress cellular proliferation and to regulate numerous biological processes; however, the responses to TGF-β differ according to cell or tissue type and the microenvironment (8–10).
Activation of secreted TGF-β and assembly of TGF-β receptor type 1 and 2 (TGF-β R1 and 2) in the cellular membrane is the first step in the TGF-β/Smad pathway. Subsequently, TGF-β R2 phosphorylates and activates TGF-β R1, which in turn phosphorylates cytoplasmic Smad2 and Smad3 [also termed receptor-Smads (R-Smads)]. Activated R-Smads bind Smad4 and move into the nucleus, and the Smads complex, along with co-factors, positively or negatively regulates the expression of target genes (11–14). In cellular proliferation, cMyc and cyclin D1 genes or proteins are downregulated, while the expression of p15, p21 and Smad2 genes is upregulated following activation of the TGF-β/Smad pathway. In non-Smad pathways, the TGF-β receptor activates other proteins, including RAS, phosphoinositide 3-kinase and FAS (12,14–16).
As a target gene of TGF-β, KLF10 may regulate the TGF-β/Smad pathway. KLF10 may enhance Smad2, p21 and plasminogen activator inhibitor-1 expression, and repress the transcription of the Smad7 gene. KLF10 also plays important roles in numerous biological processes, and it has been reported to inhibit proliferation and induce apoptosis in several cell types (10,17,18). However, the role of KLF10 in various pathophysiological conditions remains unclear.
Partial hepatectomy (PH), resulting in the removal of ~70% of the liver, is widely utilized for studies of liver regeneration, acute liver failure and the metastasis of liver cancer (19,20). KLF10 is known as a potential antiproliferative gene; however, to the best of our knowledge, there are no reports on the role of KLF10 in liver regeneration (10,21). In the present study, to elucidate the role of the KLF10 gene in liver regeneration following tissue loss, molecular and histopathological analyses were conducted using KLF10-knockout (KO) mice following a PH that removed two-thirds of the liver.
Materials and methods
Animals
All procedures were approved by the Institutional Animal Care and Use Committee of Konkuk University (Seoul, South Korea). Three pairs of 8-week-old KLF10-KO C57BL/6 J mice (age: 54–57 days, average 8 weeks; body weight: 23.1–24.9 g, average 24.1 g) were kindly provided by Professor Woon-Kyu Lee (Inha University, Incheon, Korea) (22). and five pairs of 6-week-old C57BL/6J mice (age: 32–35 days old, average 6 weeks old; body weight: 21.9–25.1 g, average 23.7 g) were obtained from the Korea Research Institute of Bioscience and Biotechnology (Daejeon, Korea). All mice were bred in the laboratory animal breeding room under specific pathogen-free conditions to produce the KO and wild-type (WT) mice groups. For genotyping each mouse, DNA samples were isolated from all mice tails using the Genomic DNA extraction kit (Bioneer Corporation, Daejeon, Korea) and subjected to polymerase chain reaction (PCR) using the AccuPower® PCR PreMix (#K-2016; Bioneer Corporation). The DNA primers for genotyping were: KLF10 forward, CCT TCC TGC CAA CAA CTC TC and reverse, TCT GAG GAG TGA CCC TTG CT; and KLF10-KO forward, TCG CCT TCT TGA CGA GTT CT (12) and reverse, TCTGAGGAGTGACCCTTGCT. The cycling conditions were initial denaturation for 5 min at 95°C, followed by 30 cycles of 1 min at 95°C, 1 min at annealing temperature, 1 min at 72°C and an additional 10 min at 72°C for final elongation. After the reaction, the PCR samples were electrophoresed on a 1.5% agarose gel. The size of KLF10 KO gene is 658 base pairs (bp) and that of WT gene is 248 bp.
Experimental design and surgical procedure
At 8 weeks of age, a two-thirds PH was performed. Subsequent to anaesthetizing with Zoletil (Virbac Corporation, Fort Worth, TX, USA) and Rompun (Bayer Korea, Ltd., Seoul, Korea), the middle abdominal skin and linea alba were incised. The left lateral and median liver lobes were excised and the peritoneum and the skin were closed (20). From each group of KLF10-KO and WT mice, 3–5 animals were sacrificed at 0, 24, 48 or 72 h post-PH using the CO2 euthanasia chamber (n=3, n=5, n=5 and n=5, respectively). At 2 h prior to euthanasia, 100 mg/kg 5-bromo-2-deoxy-uridine (BrdU; Sigma-Aldrich; EMD Millipore, Billerica, MA, USA) was injected intraperitoneally. At the time of sacrifice, all mice were grossly examined and blood was collected from the caudal vena cava. The liver was excised and weighed. The upper right lateral lobe was fixed in 10% neutral-buffered formalin for histopathological analysis and the other hepatic tissues were frozen for subsequent analyses.
Histological and immunohistochemical analysis
Fixed tissues were processed routinely for paraffin sectioning. Liver tissues were then embedded in paraffin and cut into 4-µm thick sections. The sections were deparaffinized, rehydrated and stained with hematoxylin and eosin (H&E) (Sigma-Aldrich; EMD Millipore). For immunohistochemistry, serial sections were cut, deparaffinized, rehydrated and serial incubated in 1.0% H2O2, 2 N HCl and 0.1% trypsin. The slides were pre-incubated with normal blocking serum (Vectastain ABC kit; #PK-6102; Vector Laboratories, Inc., Burlingame, CA, USA) according to the manufacturer's protocol and then incubated with anti-BrdU antibody (#B8434; dilution, 1:500; Sigma-Aldrich) for 2 h at room temperature. Detection of the BrdU was performed using biotinylated secondary antibodies (Vectastain ABC kit; #PK-6102; dilution, 1:200; Vector Laboratories, Inc.;), avidin-coupled peroxidase (Vectastain ABC kit; Vector Laboratories, Inc.), and diaminobenzidine (DAB; DAB substrate kit; Vector Laboratories, Inc.).
Reverse transcription-quantitative polymerase chain reaction (RT-qPCR)
Total RNA was prepared from frozen liver tissues using TRIzol (Invitrogen; Thermo Fisher Scientific, Inc., Waltham, MA, USA) and was reverse transcribed into cDNA using moloney-murine leukemia virus reverse transcriptase (Invitrogen; Thermo Fisher Scientific, Inc.). The cDNA was used as a template for amplification in the PCR using the AccuPower® PCR PreMix (#K-2016; Bioneer Corporation). Smad2, Smad3, Smad4, Smad7, p15, p21, TGF-β R1, TGF-β R2, cMyc, cyclin D1 and β-actin mRNA expression level were analyzed using the RT-qPCR method, as described by Shiao (23), with the previously described primers (12). The cycling conditions were initial denaturation for 5 min at 95°C, followed by 35 cycles of 1 min at 95°C, 1 min at annealing temperature, 1 min at 72°C and an additional 10 min at 72°C for final elongation. After the reaction, the PCR mixtures were electrophoresed on a 1.5% agarose gel. Band intensities were quantified using ImageQuant Software (Image Lab V4.0; Bio-Rad Laboratories, Inc., Hercules, CA, USA) and were normalized to the transcription levels of β-actin. Each sample was tested in triplicate.
Western blot analysis
Protein was extracted from the liver using the extraction solution (Pro-Prep™; Intron Biotechnology, Inc., Seongnam, Korea). The protein concentrations were determined using the bicinchoninic kit (Pierce; Thermo Fisher Scientific, Inc.). Subsequent to being transferred to nitrocellulose membranes, the proteins were blocked with 5% skimmed milk and then incubated overnight with specific antibodies against β-actin (#sc-47778; dilution, 1:500), Smad4 (#sc-7966; dilution, 1:500), Smad7 (#sc-11392; dilution, 1:1,000), p15 (#sc-65223; dilution, 1:200), p21 (#sc-817; dilution, 1:500), TGF-β R1 (#sc-398; dilution, 1:200), cMyc (#sc-56505; dilution, 1:200) (Santa Cruz Biotechnology, Inc., Dallas, TX, USA), Smad2 (#3122; dilution, 1:1,000), Smad3 (#9513; dilution, 1:200), p27 (#2552; dilution, 1:500), TGF-β R2 (#11888, dilution, 1:500) and cyclin D1 (#2922; dilution, 1:500; all from Cell Signaling Technology, Inc., Danvers, MA, USA) at 4°C. Subsequently, the membranes were washed with TBS with Tween-20 and incubated for 1 h with either horseradish peroxidase-conjugated anti-rabbit (#sc-2054; dilution, 1:1,000) or anti-mouse secondary antibodies (#sc-2031; dilution, 1:1,000; Santa Cruz Biotechnology, Inc.) at room temperature. Specific antibodies were detected with an electrochemiluminescence test kit (KPL, Inc., Gaithersburg, MD, USA). The band intensities were quantified using Image Lab V4.0 (Bio-Rad Laboratories, Inc.) and were normalized to β-actin expression (12).
Statistical analysis
Statistical analysis was performed using SPSS V14.0 software (SPSS, Inc., Chicago, IL, USA). Statistically significant differences between the studied groups were evaluated using Student's unpaired t-test. P<0.05 was considered to indicate a statistically significant difference.
Results
Gross findings
At 0, 24, 48 and 72 h post-PH, the body and liver weights of all mice were measured. Macroscopically, the volume of the remaining liver tissues increased from 48 h post-PH. The color of the liver subsequent to PH was paler than that of normal liver tissues from 48 h post-PH. At the time of sacrifice, the liver was removed and weighed to examine the liver/body weight ratio. The mean of the ratios at 0, 24, 48 and 72 h post-PH for the WT mice vs. KLF10-KO mice was 0.0194 vs. 0.0180, 0.0210 vs. 0.0194, 0.0275 vs. 0.0257 and 0.0361 vs. 0.0307, respectively (Fig. 1). Overall, KLF10-KO mice exhibited lower ratios compared with WT mice, and a significant difference was observed at 72 h post-PH (P=0.028).
Figure 1.
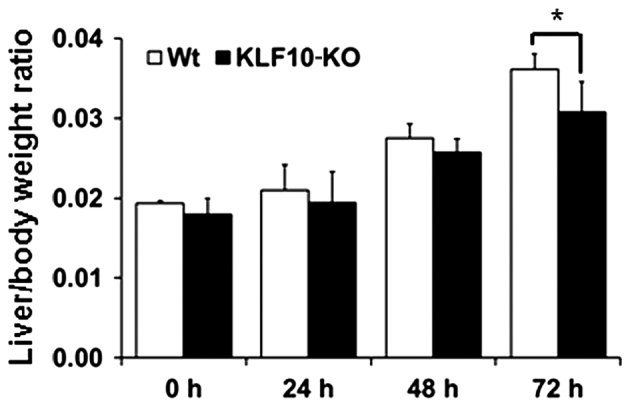
Liver/body weight ratio following PH. KLF10-KO mice exhibited lower ratios compared with WT mice, and a significant difference was observed at 72 h post-PH. *P<0.05 by unpaired Student's t-test. KLF10, krüppel-like factor 10; KO, knockout; WT, wild-type; PH, partial hepatectomy.
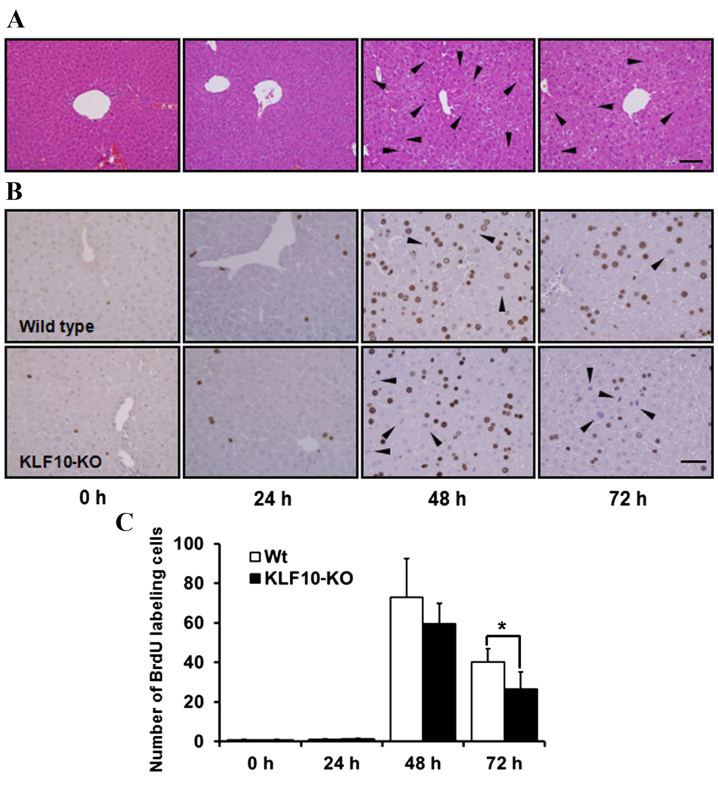
Histopathological analysis and BrdU staining
H&E staining revealed no marked features at 0 and 24 h post-PH. Pale cytoplasm and hypertrophy of hepatocytes was observed from 48 h post-PH (Fig. 2A). Mitotic figures, mainly in the centrilobular area, were the most frequent at 48 h post-PH, and these remained numerous at 72 h post-PH. Until 24 h post-PH, few mitotic figures were observed (Fig. 2A). Similarly, upon BrdU staining to analyze the proliferative potential of cells, the proportion of labeled nuclei was markedly increased at 48 h post-PH (Fig. 2B). The number of BrdU-positive nuclei was counted in an area of 0.1 mm2 under a light microscope at ×400 magnification. While calculating the BrdU labeling indices, the number of mitotic figures was added due to coarse staining of nuclei that were in the division stage (Fig. 2B). The mean of the BrdU labeling indices at 0, 24, 48 and 72 h post-PH for WT mice vs. KLF10-KO mice was 0.60 vs. 0.87, 1.12 vs. 1.30, 72.85 vs. 59.45 and 40.1 vs. 26.56, respectively (Fig. 2C). Overall, KLF10-KO mice exhibited lower indices compared with WT mice from 48 h post-PH, and a significant difference was observed at 72 h post-PH (P=0.036).
Figure 2.
Histopathological findings and BrdU stains of the liver tissue following partial hepatectomy. (A) Hematoxylin and eosin stains of 0, 24, 48 and 72 h post-PH. From 48 h post-PH, pale cytoplasm and hypertropy of hepatocytes was observed. Mitotic figures, mainly in the centrilobular area, were the most frequent at 48 h post-PH. Arrowheads indicate mitotic figures. Bar, 100 µm. (B) Immunohistochemical staining of BrdU in the liver tissue after PH. Nuclei of proliferating cells were numerous in WT mice from 48 h post-PH. Mitotic cells were coarsely stained (arrowheads). Bar, 50 µm. (C) BrdU indices of liver tissue. BrdU-positive nuclei were counted in an area of 0.1 mm2 and the number of mitotic cells was added. KLF10-KO mice showed lower indices compared with WT mice from 48 h post-PH, and there was a significant difference at 72 h after PH. *P<0.05 by unpaired Student's t-test. PH, partial hepatectomy; KLF10, krüppel-like factor 10; KO, knockout; WT, wild-type; BrdU, 5-bromo-2-deoxy-uridine.
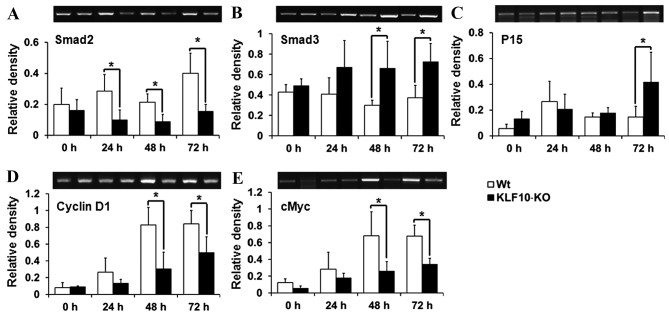
Expression of TGF-β/Smad pathway genes
To determine the causes for the gross and histological findings, the expression of the components of the TGF-β/Smads signaling pathway, which is known to be regulated by KLF10 (18), was analyzed. Smad2, Smad7 and p21, which have previously been reported to be target genes of KLF10 (10,17), and Smad3, Smad4, TGF-β1, TGF-βR1, TGF-βR2, p15, p21, cMyc and cyclin D1, which are mediators or target genes of the TGF-β/Smad pathway (14,15), were analyzed by RT-qPCR. Smad2, one of the R-Smads, exhibited significantly lower transcription levels in KLF10-KO mice compared with WT mice from 24 h post-PH (24 h, P=0.034; 48 h, P=0.036; 72 h, P=0.028; Fig. 3A). However, mRNA levels of Smad3 (another R-Smad) were increased in KLF10-KO mice compared with WT mice at all time points, and significant differences were observed from 48 h post-PH (48 h, P=0.039; 72 h, P=0.033; Fig. 3B). p15, a target gene of the TGF-β/Smad pathway, exhibited significantly increased expression in KLF10-KO mice compared with WT mice at 72 h post-PH (P=0.049; Fig. 3C). By contrast, cMyc and cyclin D1 genes, which are suppressed following activation of the TGF-β/Smad pathway, exhibited significantly greater expression in WT mice compared with KLF10-KO mice from 48 h post-PH (cMyc, 48 h, P=0.042; 72 h, P=0.011: cyclin D1, 48 h, P=0.036; 72 h, P=0.047; Fig. 3D and E). No significant differences were observed in the mRNA levels of other genes (data not shown).
Figure 3.
Analysis of the mRNA levels of the genes (Smad2, Smad3, p15, cyclin D1 and cMyc) involved in the transforming growth factor-β/Smad pathway. (A) Smad2 was downregulated, while (B) Smad3 and (C) p15 were upregulated in the KLF10-KO mice (D) Cyclin D1 and (E) cMyc were also downregulated. Band intensities were quantified and normalized to the β-actin level. *P<0.05 by unpaired Student's t-test. KLF10, krüppel-like factor 10; KO, knockout; WT, wild-type.
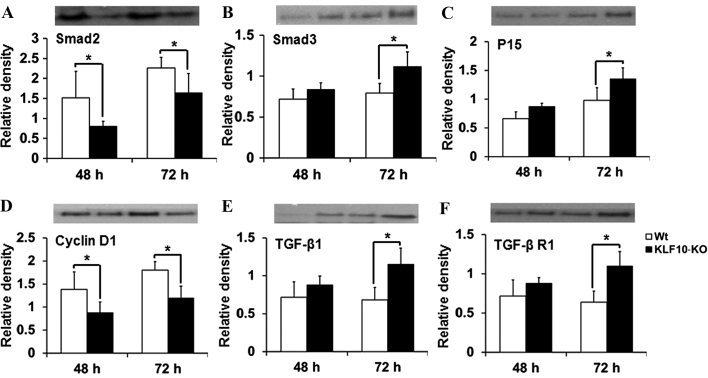
Expression of proteins involved in the TGF-β/Smad pathway
The expression of proteins targeted by the TGF-β pathway (Smad2, Smad3, Smad4, Smad7, p15, p21, p27, TGF-β1, TGF-β R1, TGF-β R2 and cyclin D1) was then investigated. In RT-qPCR analysis, significant differences were mostly observed at 48 and 72 h post-PH. The tissue lysates from these time points were analyzed by western blotting. The results for Smad2, Smad3 and cyclin D1 were similar to those obtained by RT-qPCR. Smad2 expression was significantly deacreased in KLF10-KO mice at 48 and 72 h post-PH compared with that in WT mice (P=0.049 and P=0.043, respectively; Fig. 4A). Protein levels of Smad3 and p15 were increased in the KLF10-KO mice compared with those in the WT mice, and significant differences were observed at 72 h post-PH (P=0.019 and P=0.040, respectively; Fig. 4B and C). The cyclin D1 level was significantly lower at 48 and 72 h post-PH in the KLF10-KO mice compared with that in the WT mice (P=0.045 and P=0.006, respectively; Fig. 4D). Additionally, the level of TGF-β1, which is positively regulated by the TGF-β/Smad pathway (14), was increased in the KLF10-KO mice compared with that in the WT mice, and significant differences were observed at 72 h post-PH (P=0.012; Fig. 4E). Expression of TGF-β R1, which is involved in the early steps of the TGF-β pathway (14), was similar to that of TGF-β1 (Fig. 4F). Other proteins did not show any significant differences (data not shown).
Figure 4.
Analysis of the levels of the proteins (Smad2, Smad3, p15, cyclin D1, TGF-β1 and TGF-β R1) involved in the TGF-β/Smad pathway. Considering reverse transcription-quantitative polymerase chain reaction results, liver tissues at 48 and 72 h post-partial hepatectomy were examined. (A) Smad2 levels were lower, while (B) Smad3 and (C) p15 levels were higher in the KLF10-KO mice compared with those in the WT mice. (D) Cyclin D1 levels were lower, while (E) TGF-β1 and (F) TGF-β R1 levels were higher in the KLF10 KO mice compared with those in the WT mice. Band intensities were quantified and normalized to the β-actin level. *P<0.05 by unpaired Student's t-test. TGF-β1, transforming growth factor-β1; TGF-β R1, transforming growth factor-β receptor 1; KLF10, krüppel-like factor 10; KO, knockout; WT, wild-type.
Discussion
Numerous factors may alter liver mass, and a number of signaling pathways are involved in liver regeneration (1,4,7). TGF-β is known to suppress cellular proliferation, including hepatic regeneration (8,9). KLF10, one of the target genes of TGF-β, enhances TGF-β-induced anti-proliferative effects in certain cell types by inducing the expression of several genes involved in TGF-β signaling, including Smads, p15, p21 and TGF-β1 (24–26). However, the exact function of KLF10 under various pathophysiological conditions remains unclear, and to the best of our knowledge, its role in liver regeneration has never been examined.
In the present study, the role of KLF10 in liver regeneration following tissue loss was investigated using KLF10-KO mice. The liver/body weight ratio of the KLF10-KO mice was lower than that of the WT mice at all examined time points, and a significant difference was observed at 72 h post-PH (Fig. 1). KLF10-KO mice also exhibited lower BrdU indices compared with WT mice from 48 h post-PH, and a significant difference was observed at 72 h post-PH (Fig. 2C). Thus, cellular proliferation appeared to be suppressed in KLF10-KO mice following PH (under conditions that supported regeneration in WT mice). To determine the causes for the decreased cellular proliferation in KLF10-KO mice, the expression of genes involved in the TGF-β/Smad pathway was examined by RT-qPCR. Under normal conditions and immediately following PH, no difference was observed in the expression of the examined genes. However, the mRNA levels of Smad2 decreased significantly in KLF10-KO mice from 24 h post-PH (Fig. 3A). KLF10 has been reported to enhance Smad2 expression (10), and this decrease may be a cause for KLF10 gene ablation in the KO mice. Unlike that of Smad2, the expression of Smad3 (a co-Smad) increased from 48 h post-PH in the KLF10-KO mice (Fig. 3B). The expression of p15, whose transcription is induced by the activated Smads complex, also increased from 48 h post-PH in the KLF10-KO mice (Fig. 3C). Consequently, the cMyc and cyclin D1 genes, which are downregulated by p15, showed significantly lower expression in the KLF10-KO mice compared with the WT mice from 48 h post-PH (Fig. 3D and E). Western blot analysis results for Smad2, Smad3, p15 and cyclin D1 were similar to those of RT-qPCR. In addition, the levels of TGF-β1 and TGF-β R1, which are involved in the early phases of the TGF-β pathway, were significantly increased at 72 h post-PH in the KLF10-KO mice compared with the WT mice (Fig. 4).
These results indicated that the knockout of KLF10 led to repression of the transcription and function of the proliferation-associated genes cMyc and cyclin D1 from 48 h post-PH, thereby inhibiting liver regeneration. This repression may be induced by the activation of the TGF-β/Smad pathway. Expression of TGF-β R1, TGF-β1, Smad3 and p15, one of the genes positively regulated by the TGF-β pathway, was increased in the KLF10-KO mice. Thus, during liver regeneration following PH, lack of KLF10 suppresses the proliferation of hepatocytes by activation of the TGF-β/Smad pathway, and the suppression of hepatocellular proliferation can be observed in a delayed manner at 72 h post-PH.
Cellular responses to TGF-β depend on the cell types, the microenvironment and the tissue type (9,27). KLF10, an early target of TGF-β, has been reported to exert effects similar to those of TGF-β. However, the specific functions of KLF10 under various physiological conditions are not well characterized (18,26,28,29). Our previous study reported the tumor-suppressor effects against chemically-induced liver tumorigenesis in KLF10-KO mice (12). Similarly, the anti-proliferative effects on hepatocytes after PH were shown in the present study. These results show that although there were no phenotypical changes in the liver of KLF10-KO mice under normal physiological conditions, the TGF-β/Smad pathway exhibited enhanced activation and cellular proliferation was decreased under conditions that promote cellular proliferative changes in the liver, including PH and chemically-induced tumorigenesis.
The aforementioned results may be due to KLF10 transcription being induced by factors other than TGF-β, including estrogen and epidermal growth factor (8,14,30,31). Furthermore, certain intracellular proteins, including KLF11, were recently reported to exhibit effects similar to those of KLF10 (26,32). Considering these findings, certain compensatory mechanisms for KLF10 ablation may exist in non-Smad TGF-β pathways or KLF10 signaling under proliferative conditions. The detailed molecular mechanism underlying this compensatory mechanism warrants additional study.
In conclusion, the hepatocytes of KLF10-KO mice exhibited less proliferation compared with those of WT mice following PH in the present study. This decrease was caused by reinforcement of TGF-β/Smad signaling. TGF-β1, TGF-β R1 and Smad3 were upregulated, and this induced increased expression of p15. These factors led to repressed expression of the proliferation-associated genes, cMyc and cyclin D1. The present findings demonstrated that knockout of KLF10 suppressed cellular proliferation through reinforcement of the TGF-β/Smad pathway in the presence of external stimuli that could induce hepatocyte proliferation, including tumorigenesis and regeneration, following tissue loss (12).
Acknowledgements
The present study was supported by the Konkuk University in 2013.
References
- 1.Fausto N, Campbell JS, Riehle KJ. Liver regeneration. J Hepatol. 2012;57:692–694. doi: 10.1016/j.jhep.2012.04.016. [DOI] [PubMed] [Google Scholar]
- 2.Fausto N. Liver regeneration. J Hepatol. 2000;32(1 Suppl):S19–S31. doi: 10.1016/S0168-8278(00)80412-2. [DOI] [PubMed] [Google Scholar]
- 3.Michalopoulos GK. Liver regeneration. J Cell Physiol. 2007;213:286–300. doi: 10.1002/jcp.21172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Michalopoulos GK. Liver regeneration after partial hepatectomy: Critical analysis of mechanistic dilemmas. Am J Pathol. 2010;176:2–13. doi: 10.2353/ajpath.2010.090675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Maluccio M, Covey A. Recent progress in understanding, diagnosing and treating hepatocellular carcinoma. CA Cancer J Clin. 2012;62:394–399. doi: 10.3322/caac.21161. [DOI] [PubMed] [Google Scholar]
- 6.Mathers CD, Boerma T, Ma Fat D. Global and regional causes of death. Br Med Bull. 2009;92:7–32. doi: 10.1093/bmb/ldp028. [DOI] [PubMed] [Google Scholar]
- 7.Taub R. Liver regeneration: From myth to mechanism. Nat Rev Mol Cell Biol. 2004;5:836–847. doi: 10.1038/nrm1489. [DOI] [PubMed] [Google Scholar]
- 8.Derynck R, Akhurst RJ, Balmain A. TGF-beta signaling in tumor suppression and cancer progression. Nat Genet. 2001;29:117–129. doi: 10.1038/ng1001-117. [DOI] [PubMed] [Google Scholar]
- 9.Itoh S, ten Dijke P. Negative regulation of TGFbeta receptor/Smad signal transduction. Curr Opin Cell Biol. 2007;19:176–184. doi: 10.1016/j.ceb.2007.02.015. [DOI] [PubMed] [Google Scholar]
- 10.Subramaniam M, Hawse JR, Rajamannan NM, Ingle JN, Spelsberg TC. Functional role of KLF10 in multiple disease processes. Biofactors. 2010;36:8–18. doi: 10.1002/biof.67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ellenrieder V. TGFbeta-regulated gene expression by smads and Sp1/KLF-like transcription factors in cancer. Anticancer Res. 2008;28:1531–1539. [PubMed] [Google Scholar]
- 12.Heo SH, Jeong ES, Lee KS, Seo JH, Lee WK, Choi YK. Krüppel-like factor 10 null mice exhibit lower tumor incidence and suppressed cellular proliferation activity following chemically induced liver tumorigenesis. Oncol Rep. 2015;33:2037–2044. doi: 10.3892/or.2015.3801. [DOI] [PubMed] [Google Scholar]
- 13.Inman GJ. Switching TGFβ from a tumor suppressor to a tumor promoter. Curr Opin Genet Dev. 2011;21:93–99. doi: 10.1016/j.gde.2010.12.004. [DOI] [PubMed] [Google Scholar]
- 14.Massagué J. TGFbeta in Cancer. Cell. 2008;134:215–230. doi: 10.1016/j.cell.2008.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kaminska B, Wesolowska A, Danilkiewicz M. TGF beta signalling and its role in tumour pathogenesis. Acta Biochim Pol. 2005;52:329–337. [PubMed] [Google Scholar]
- 16.Kang JS, Liu C, Derynck R. New regulatory mechanisms of TGF-beta receptor function. Trends Cell Biol. 2009;19:385–394. doi: 10.1016/j.tcb.2009.05.008. [DOI] [PubMed] [Google Scholar]
- 17.Johnsen SA, Subramaniam M, Monroe DG, Janknecht R, Spelsberg TC. Modulation of transforming growth factor beta (TGF-beta)/Smad transcriptional responses through targeted degradation of TGF-beta-inducible early gene-1 by human seven in absentia homologue. J Biol Chem. 2002;277:30754–30759. doi: 10.1074/jbc.M204812200. [DOI] [PubMed] [Google Scholar]
- 18.Subramaniam M, Hawse JR, Johnsen SA, Spelsberg TC. Role of TIEG1 in biological processes and disease states. J Cell Biochem. 2007;102:539–548. doi: 10.1002/jcb.21492. [DOI] [PubMed] [Google Scholar]
- 19.Martins PN, Theruvath TP, Neuhaus P. Rodent models of partial hepatectomies. Liver Int. 2008;28:3–11. doi: 10.1111/j.1478-3231.2007.01628.x. [DOI] [PubMed] [Google Scholar]
- 20.Mitchell C, Willenbring H. A reproducible and well-tolerated method for 2/3 partial hepatectomy in mice. Nat Protoc. 2008;3:1167–201170. doi: 10.1038/nprot.2008.80. [DOI] [PubMed] [Google Scholar]
- 21.Breitkopf K, Weng H, Dooley S. TGF-β/Smad-signaling in liver cells: Target genes and inhibitors of two parallel pathways. Signal Transduction. 2006;6:329–337. doi: 10.1002/sita.200600097. [DOI] [Google Scholar]
- 22.Song KD, Kim DJ, Lee JE, Yun CH, Lee WK. KLF10, transforming growth factor-β-inducible early gene 1, acts as a tumor suppressor. Biochem Biophys Res Commun. 2012;419:388–394. doi: 10.1016/j.bbrc.2012.02.032. [DOI] [PubMed] [Google Scholar]
- 23.Shiao YH. A new reverse transcription-polymerase chain reaction method for accurate quantification. BMC Biotechnol. 2003;3:22. doi: 10.1186/1472-6750-3-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Buenemann CL, Willy C, Buchmann A, Schmiechen A, Schwarz M. Transforming growth factor-beta1-induced Smad signaling, cell-cycle arrest and apoptosis in hepatoma cells. Carcinogenesis. 2001;22:447–452. doi: 10.1093/carcin/22.3.447. [DOI] [PubMed] [Google Scholar]
- 25.Dooley S, Weng H, Mertens PR. Hypotheses on the role of transforming growth factor-beta in the onset and progression of hepatocellular carcinoma. Dig Dis. 2009;27:93–101. doi: 10.1159/000218340. [DOI] [PubMed] [Google Scholar]
- 26.Spittau B, Krieglstein K. Klf10 and Klf11 as mediators of TGF-beta superfamily signaling. Cell Tissue Res. 2012;347:65–72. doi: 10.1007/s00441-011-1186-6. [DOI] [PubMed] [Google Scholar]
- 27.Heldin CH, Miyazono K. Transforming growth factor-beta. An interesting candidate for clinical use. Lakartidningen. 1995;92:1569–1572. (In Swedish) [PubMed] [Google Scholar]
- 28.Bensamoun SF, Hawse JR, Subramaniam M, Ilharreborde B, Bassillais A, Benhamou CL, Fraser DG, Oursler MJ, Amadio PC, An KN, Spelsberg TC. TGF-beta inducible early gene-1 knockout mice display defects in bone strength and microarchitecture. Bone. 2006;39:1244–1251. doi: 10.1016/j.bone.2006.05.021. [DOI] [PubMed] [Google Scholar]
- 29.Bos JM, Subramaniam M, Hawse JR, Christiaans I, Rajamannan NM, Maleszewski JJ, Edwards WD, Wilde AA, Spelsberg TC, Ackerman MJ. TGFβ-inducible early gene-1 (TIEG1) mutations in hypertrophic cardiomyopathy. J Cell Biochem. 2012;113:1896–1903. doi: 10.1002/jcb.24058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Moustakas A, Heldin CH. Non-Smad TGF-beta signals. J Cell Sci. 2005;118:3573–3584. doi: 10.1242/jcs.02554. [DOI] [PubMed] [Google Scholar]
- 31.Tsubone T, Moran SL, Subramaniam M, Amadio PC, Spelsberg TC, An KN. Effect of TGF-beta inducible early gene deficiency on flexor tendon healing. J Orthop Res. 2006;24:569–575. doi: 10.1002/jor.20101. [DOI] [PubMed] [Google Scholar]
- 32.Gohla G, Krieglstein K, Spittau B. Tieg3/Klf11 induces apoptosis in OLI-neu cells and enhances the TGF-beta signaling pathway by transcriptional repression of Smad7. J Cell Biochem. 2008;104:850–861. doi: 10.1002/jcb.21669. [DOI] [PubMed] [Google Scholar]