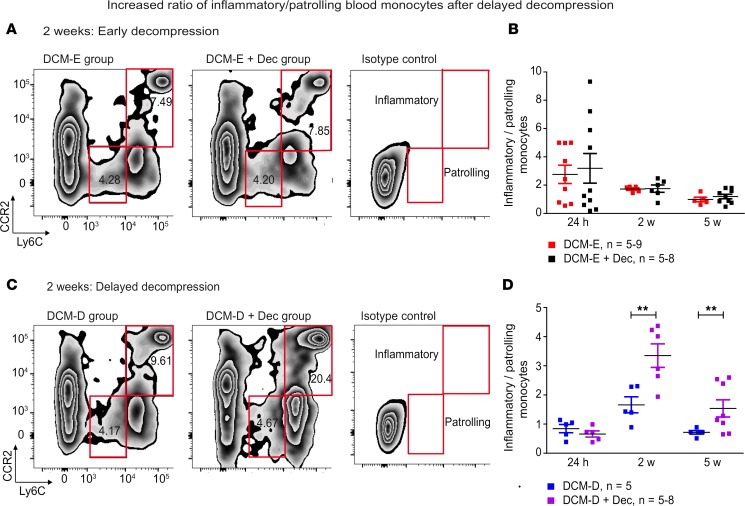
Figure 5. Delayed surgical decompression increases the ratio of inflammatory/patrolling blood monocytes.
(A) Blood samples were transcardially collected at selected time points in the DCM-E and DCM-E + Dec groups. Representative contour plots of blood monocytes for DCM-E, DCM-E + Dec, and isotype controls at 2 weeks after surgical decompression. Inflammatory monocytes were gated as Ly6ChiCCR2+ (upper red panel) and patrolling monocytes as Ly6CloCCR2– (lower red panel). (B) The ratio of inflammatory/patrolling monocytes was not significantly different between the DCM-E and DCM-E + Dec groups at all time points (24 hours [DCM-E, n = 9; DCM-E + Dec, n = 10], 2 weeks [DCM-E, n = 5; DCM-E + Dec, n = 6], and 5 weeks [DCM-E, n = 5; DCM-E + Dec, n = 9]). (C) Representative contour plots of inflammatory and patrolling blood monocytes for DCM-D, DCM-D + Dec, and isotype control at 2 weeks after surgical decompression. (D) The ratio of inflammatory/patrolling monocytes was similar between DCM-D and DCM-D + Dec groups at 24 hours after surgery (DCM-D, n = 5; DCM-D + Dec, n = 5). However, this ratio was higher in the group receiving delayed decompression as compared with the same group, at 2 and 5 weeks after decompression (DCM-D, n = 5; DCM-D + Dec, n = 5–8). **P < 0.01, two-way ANOVA. Data are presented as mean ± SEM. DCM, degenerative cervical myelopathy; Dec, decompression; DCM-E, age-matched early sham decompressed group; DCM-D, age-matched delayed sham decompressed group.