Figure 1.
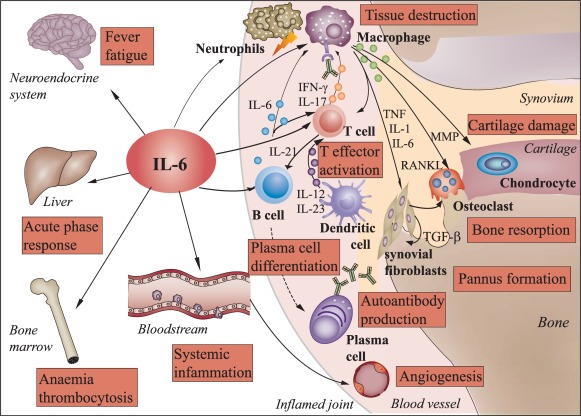
Pleiotropic effects of interleukin‐6 in rheumatoid arthritis. Interleukin (IL)‐6 exerts systemic effects on multiple tissues and cells of the immune system. In rheumatoid arthritis (RA), IL‐6 triggers systemic inflammatory processes, such as increase in thermogenesis and synthesis of acute phase proteins by hepatocytes, resulting in manifestations such as fever, fatigue and anaemia. In the synovial tissue of the joints, IL‐6 also induces vascularization, infiltration of inflammatory cells, such as neutrophils and monocytes/macrophages, and expansion of synovial fibroblasts leading to RA tissue destruction and pannus formation, respectively. IL‐6 also promotes cartilage damage, the differentiation of osteoclasts and bone resorption by stimulating the expression of matrix metalloproteinases (MMPs) and receptor activator of nuclear factor kappa B (NK‐κB) ligand (RANKL). Furthermore, IL‐6 promotes the expansion of CD4+ T cells and, together with cytokines secreted by inflammatory dendritic cells, induces the differentiation into interferon (IFN)‐γ and/or IL‐17‐producing T effector cells which, in turn, activate macrophages and attract neutrophils. IL‐6 drives also the differentiation of B cells to autoantibody‐producing plasma cells. Binding of autoantibodies to Fc receptors further triggers activation and release of inflammatory mediators by macrophages. TGF = transforming growth factor; TNF = tumour necrosis factor.
