Abstract
Background:
Olfactory neuroblastoma (ONB) is a rare malignant neuroectodermal tumor of the nasal cavity. Mixed olfactory neuroblastoma which contains areas of divergent differentiation is even rare. Till date, only 4 cases of mixed olfactory neuroblastomas have been reported.
Case Description:
We report the case of a 46-year-old male who presented with the chief complaints of nasal bleeding and nasal obstruction since 4 months. Radiological imaging was suggestive of a large heterogeneous mass in the left superior nasal cavity with extensions into bilateral maxillary, ethmoidal, and sphenoidal sinuses, as well as into the anterior cranial fossa. Bifrontal osteoplastic craniotomy and excision of the intracranial part of the tumor from above and transnasal endoscopic removal of the mass in the nasal cavities and paranasal sinuses from below was done. Postoperative radiological imaging was suggestive of gross complete excision of the mass. Histopathological diagnosis was “mixed olfactory neuroblastoma-carcinoma (squamous and glandular differentiation) Hyams grade IV.” On immunohistochemistry, the tumor cells were positive for neuron specific enolase (NSE), synaptophysin, chromogranin, and CD56 and peripherally for S100. Because of personal reasons, the patient did not take adjuvant radiotherapy. He presented again after 2 months with a full blown recurrence of esthesioneuroblastoma with similar extensions as before. The patient is now planned for salvage surgery followed by adjuvant chemoradiation.
Conclusion:
We report the 5th case in the world of mixed olfactory neuroblastoma-carcinoma with squamous and glandular differentiation. From an analysis of the findings in the 5 reported cases of mixed olfactory neuroblastomas, one might infer that a separate subcategory of ONB, i.e., mixed ONB, should be considered because mixed ONBs have an aggressive behavior, high rates of recurrence, and these tumors should be treated aggressively by multimodality treatment.
Keywords: Carcinoma, esthesioneuroblastoma, mixed, neuroblastoma, olfactory
INTRODUCTION
Olfactory neuroblastoma (ONB), also called as esthesioneuroblastoma, is a rare malignant neuroectodermal tumor of the nasal cavity. Mixed olfactory neuroblastoma which contains areas of divergent differentiation is even rare. Till date, only 4 cases of mixed olfactory neuroblastomas have been reported.[3,13,15]
CASE REPORT
A 46-year-old male was admitted with the chief complaints of nasal bleeding and nasal obstruction since 4 months. His blood profile for biochemistry and hematology was within normal limits. Tests for human immunodeficiency virus (HIV), hepatitis B surface antigen (HBsAg), and hepatitis C virus were negative.
Contrast-enhanced computed tomography scan (CECT) and contrast-enhanced magnetic resonance imaging (CEMRI) of the brain and paranasal sinuses were suggestive of a large heterogeneous mass in the left superior nasal cavity (causing its expansion) with intense heterogeneous post-contrast enhancement. The lesion was extending posteriorly into the nasopharynx, medially into the right nasal cavity and right maxillary antrum with deviation of the nasal septum to the right side, and laterally into the left maxillary sinus with blockage of the osteomeatal complex. Superiorly, the lesion was seen to erode the cribriform plate and extend into the anterior cranial fossa. There was evidence of peritumoral cysts at the tumor–brain interface with perilesional edema. The lesion involved bilateral ethmoidal and sphenoidal sinuses also [Figure 1]. The patient underwent a combined bifrontal osteoplastic craniotomy and excision of the intracranial part of the tumor from above and transnasal endoscopic removal of the mass in the nasal cavities and paranasal sinuses from below. Postoperative CECT scan of the brain and paranasal sinuses was suggestive of gross complete excision of the mass [Figure 2].
Figure 1.
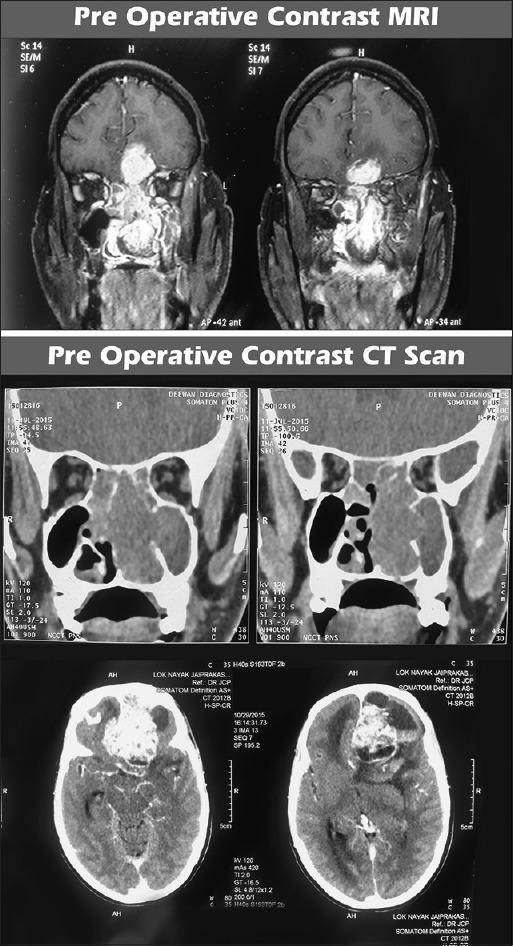
Pre operative CEMRI and CECT scan of the brain and paranasal sinuses showing dumbbell shaped mass in the left superior nasal cavity with extensions into the anterior cranial fossa and paranasal sinuses. The ‘waist’ of the dumbbell is at the cribriform plate. The mass shows intense heterogeneous post contrast enhancement. Peritumoral cysts are also noted at the tumor brain interface
Figure 2.
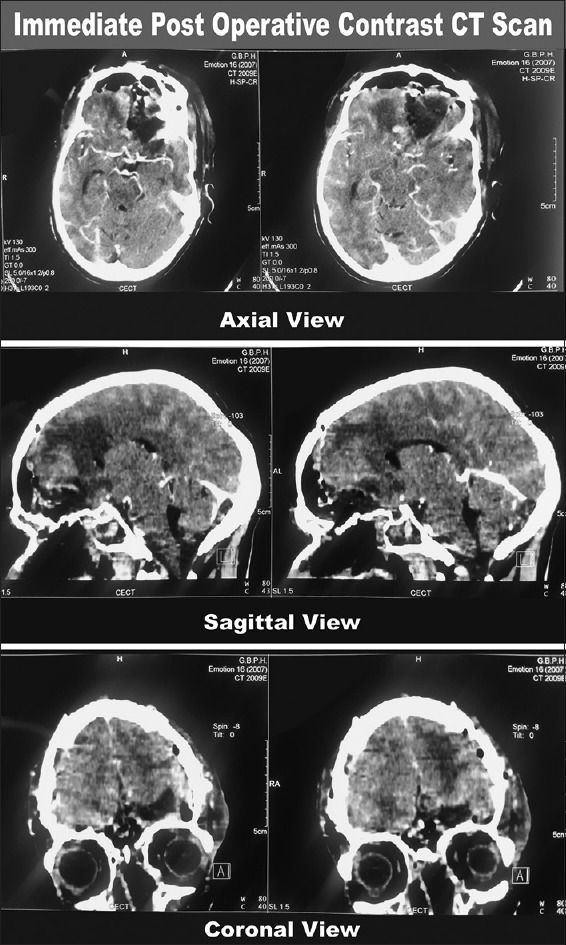
Immediate post operative CECT scan of the brain and paranasal sinuses showing complete excision of the mass
On histopathological examination (HPE), the tumor was composed of lobules, sheets, and nest of primitive cells which were displaying high nuclear: cytoplasmic (N:C) ratio, pleomorphism, round hyperchromatic nuclei with inconspicuous nucleoli, and scanty cytoplasm. On immunohistochemistry (IHC), the tumor cells were positive for neuron-specific enolase (NSE), synaptophysin, chromogranin, CD56, and peripherally for S100 and were negative for CD99. True rosette formation was noted. Large areas of necrosis and brisk mitotic activity were seen. Neurofibrillary matrix was absent. The tumor cells were seen infiltrating the adjacent brain parenchyma. Some areas showed epithelial differentiation in the form of glandular, squamous, and respiratory epithelium. On IHC, these areas were positive for cytokeratin (CK) and epithelial membrane antigen (EMA). CK 5/6 was positive in the squamous morules and CK 7 focally in the glandular component. Intervening stroma was positive for vimentin. The final histopathological report was “mixed olfactory neuroblastoma-carcinoma (squamous and glandular differentiation) Hyams grade IV” [Figure 3].
Figure 3.
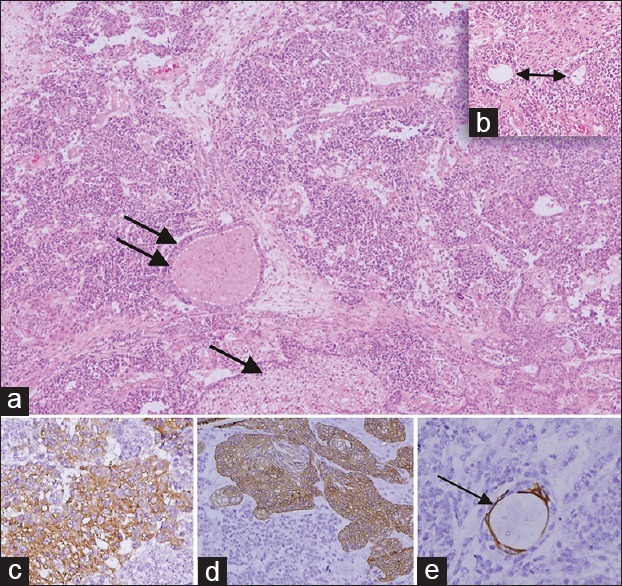
(a and b) Hematoxylin and eosin stained slides (x100) - showing olfactory neuroblastoma which is having a lobular pattern of primitive cells, no fibrillary matrix and showing squamous (single arrow) and glandular differentiation (double arrow) and inset (x200) having true rosettes (Flexner Wintersteiner rossette, double head arrow). (c-e) IHC (×400) (c) Strong synaptophysin positivity is seen in the tumor cells, (d) Cytokeratin 5/6 positivity is seen in the squamous cells and (e) Cytokeratin 7- focal positivity in the glands (thin arrow)
The patient was discharged after removal of stitches on postoperative day 7. He was advised to take adjuvant radiotherapy, which the patient did not take due to personal reasons. Two months later, he presented to us again with nasal bleeding and nasal obstruction. CECT scan and CEMRI of the brain and paranasal sinuses were suggestive of a large recurrence of esthesioneuroblastoma with similar extensions as before [Figure 4]. Metastatic work up of the patient was normal. The patient is now planned for salvage surgery followed by adjuvant chemoradiation.
Figure 4.
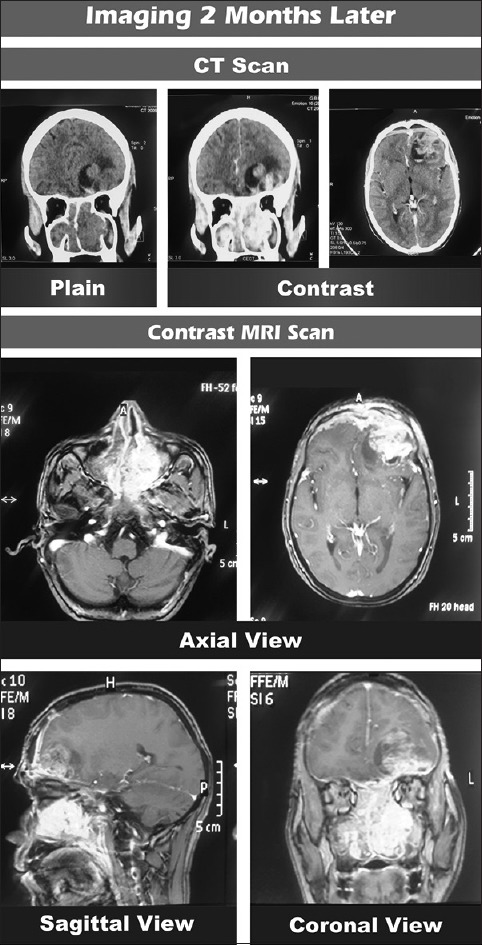
Imaging two months after the first surgery showing full blown recurrence of esthesioneuroblastoma
DISCUSSION
Olfactory neuroblastoma (ONB) is a rare malignant neuroectodermal tumor of the nasal cavity. Berger and Luc first described this uncommon neoplasm in 1924.[2] Since then, approximately 1200 cases of ONB have been identified. Mixed olfactory neuroblastoma which contains areas of divergent differentiation is even rare. Mixed olfactory neuroblastoma with carcinoma was first reported by Miller et al. in 1984.[13] Till date, only 4 cases of mixed olfactory neuroblastomas have been reported (2 cases by Miller et al. and 1 each by Chang et al. and Sato et al).[3,13,15] The specialized sensory olfactory epithelium contains three cell types – basal cells, olfactory neurosensory cells, and supporting sustentacular cells. The basal cells are the stem cells which may be the candidate cell of origin for mixed ONB.[18]
The incidence of ONB is approximately 2–3% of all sinonasal tract tumors.[18] There is no gender predilection. ONB may occur at any age with a bimodal peak in the second and sixth decades of life.[5,16]
The most common presenting symptoms are nasal bleeding and nasal obstruction. Other symptoms include anosmia, headache, pain, excessive lacrimation, rhinorrhea, proptosis, and visual disturbances. Uncommonly, ONB may be associated with syndrome of inappropriate antidiuretic hormone secretion (SIADH) with dilutional hyponatremia or ectopic adrenocorticotropic hormone (ACTH) production leading to Cushing syndrome.[18]
On imaging studies, a “dumbbell shaped” mass extending across the cribriform plate is one of the most characteristic findings of this tumor. The upper portion of the dumbbell-shaped mass is in the anterior cranial fossa whereas the lower portion is in the nasal cavity with the “waist” at the cribriform plate as seen in our case [Figure 1]. Another characteristic imaging feature of ONBs is the presence of peritumoral cysts at the tumor brain interface, as seen in our case [Figures 1 and 4].[17]
ONB is a distinct entity from primitive neuroectodermal tumor (PNET) and the Ewing sarcoma family of tumors. The most common translocation, present in approximately 90% of Ewing sarcoma cases, is t(11;22) (q24;q12) which is not seen in cases of ONB.[1]
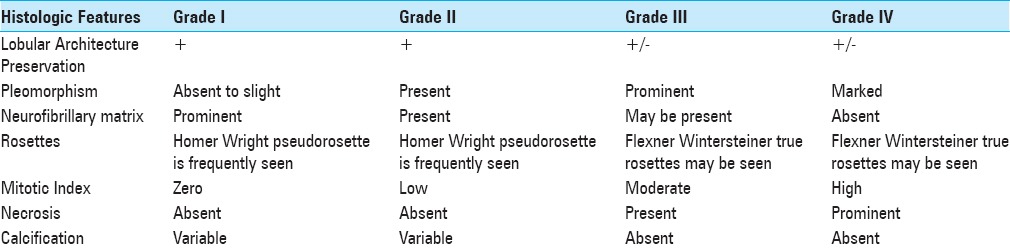
Histologically, ONB is divided into 4 grades by Hyams [Table 1].[8] Hyams grades III and IV are associated with a poor prognosis. On IHC studies, ONBs are positive for NSE, synaptophysin, chromogranin, CD56, and neurofilament protein (NFP). S-100 protein staining seen along the periphery of the neoplastic lobules is characteristic of ONB as seen in our case. Epithelial markers including epithelial membrane antigen (EMA) and carcinoembryonic antigen (CEA) are absent in ONB. Hematolymphoid markers (CD45, B cell, and T cell), melanoma markers [human melanoma black 45 (HMB 45), melan A, tyrosinase], myogenic markers (desmin, myogenin, myoglobin), and Ewing's sarcoma markers (CD99/MIC2) are also absent in ONB cases.[10]
Table 1.
Hyam's histological grading system for olfactory neuroblastoma's
Kadish et al. were the first to propose a staging classification for ONB.[9] According to Kadish staging, in group A, the tumor is confined to the nasal cavity; in group B, the tumor involves the nasal cavity plus one or more paranasal sinuses; and in group C, the tumor extends beyond the sinonasal cavities. According to Kadish staging, our case belongs to group C.
Morita et al. modified the Kadish staging to include 4 groups.[14] Group D was added to the Kadish classification, which included all patients of ONB with metastasis to the cervical lymph nodes or distant sites. Group C was redefined to include only cases of local disease with extension beyond the paranasal sinuses into the anterior cranial fossa.[14]
Complete surgical excision of the mass (craniofacial resection either open or endoscopic) followed by adjuvant radiotherapy is the “gold standard” for treating ONBs. In 1976, at the University of Virginia, Drs. Jane and Fitz Hugh introduced craniofacial resection for the treatment of ONB. These masses should be resected en-bloc, and the ipsilateral cribriform plate and crista galli should be resected along with the specimen.
Neck metastasis, at presentation, occurs in 5–8% of the patients, although the incidence of neck metastasis in patients with ONB is 20–25%.[19] The most common site of metastasis in patients of ONB is the cervical lymph nodes (Level II lymph nodes are the most frequently involved followed by level I, level III, and the retropharyngeal group of lymph nodes).[7,19] When neck nodes are involved in the disease process, the treatment should include a selective neck dissection followed by adjuvant radiotherapy to the neck.[19] At present, data is not sufficient to justify elective neck dissection or elective neck irradiation for patients of ONB with N0 neck.[19] Distant metastasis occurs in 12–25% of these patients with lung, brain, and bone being the most common sites.[4]
ONB is believed to be a radiosensitive tumor. Radiation therapy is usually given in the adjuvant setting, and the dose received is usually less than 60 Gy. Chemotherapy may have a role in patients with advanced disease. At the University of Virginia, patients of ONB with tumors which are staged as Kadish A or B received preoperative radiotherapy followed by a craniofacial resection, and patients with advanced disease (Kadish stage C) were treated first with two cycles of cyclophosphamide and vincristine with or without doxorubicin followed by 50 Gy of radiotherapy, which was followed by a craniofacial resection. With this regimen, the disease free survival was 86.5% and 82.6% at 5 and 15 years, respectively.[11] A study at the Massachusetts Eye and Ear Infirmary and Massachusetts General Hospital, Harvard medical school concluded that ONBs can be safely and effectively treated with craniofacial resection followed by proton beam irradiation.[6] The 5-year disease-free and overall survival rates in this study were 86.4% and 95.2%, respectively.[6] McElroy et al. in their paper “Chemotherapy for advanced esthesioneuroblastoma: the Mayo Clinic experience” concluded that cisplatin-based chemotherapy is active in advanced, high-grade esthesioneuroblastoma and is a reasonable choice in the systemic treatment of these patients.[12] The M.D. Anderson Cancer Centre approach to treat ONB is complete surgical resection (craniofacial resection) followed by adjuvant radiotherapy.[4] Overall patient survival rates with this approach at 5 and 10 years were 89% and 81%, respectively.[4]
Five year survival data for stages A, B, and C of the Kadish classification system are 75%, 68% and 41%, respectively.[18] Most frequent recurrence is local with recurrence rates of approximately 30%. The mean time for recurrence of ONB is 4.67 years.[4] The mean time for recurrence in the 5 cases of mixed ONB described in literature is 7 months (4 out of the 5 cases recurred at 11 months, 12 months, 3 months, and 2 months respectively) with a recurrence rate of 80%. In our case, there was a full blown recurrence in 2 months.
CONCLUSION
We report the 5th case in the world of mixed olfactory neuroblastoma-carcinoma with squamous and glandular differentiation.[3,13,15] From an analysis of the findings in the 5 cases of mixed olfactory neuroblastomas, one might infer that a separate subcategory of ONBs i.e., mixed ONBs, should be considered because mixed ONBs have an aggressive behavior, high rates of recurrence, and these tumors should be treated aggressively by multimodality treatment.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Footnotes
Contributor Information
Charandeep S. Gandhoke, Email: charandeepsingh2008@gmail.com.
Aditi Dewan, Email: adidewan@gmail.com.
Divya Gupta, Email: divyagupta.leo@gmail.com.
Simran K. Syal, Email: simransyal100@gmail.com.
Anita Jagetia, Email: anitajagetia@gmail.com.
Ravindra K. Saran, Email: ravindraksaran@hotmail.com.
Ravi Meher, Email: ravimeher@gmail.com.
Arvind K. Srivastava, Email: aksrivastava2008@gmail.com.
Daljit Singh, Email: drdaljit@hotmail.com.
REFERENCES
- 1.Argani P, Perez-Ordonez B, Xiao H. Olfactory neuroblastoma is not related to the Ewing family of tumors: Absence of EWS/FLI1 gene fusion and MIC2 expression. Am J Surg Pathol. 1998;22:391–8. doi: 10.1097/00000478-199804000-00002. [DOI] [PubMed] [Google Scholar]
- 2.Berger L, Luc R. L’esthesioneuroepitheliome olfactif. Bull Assoc Fr Etude Cancer. 1924;13:410–21. [Google Scholar]
- 3.Chang KC, Jin YT, Chen RM, Su LJ. Mixed olfactory neuroblastoma and craniopharyngioma: An unusual pathological finding. Histopathology. 1997;30:378–82. doi: 10.1046/j.1365-2559.1997.d01-615.x. [DOI] [PubMed] [Google Scholar]
- 4.Diaz EM, Johnigan RH, Pero C, El-Naggar AK, Roberts DB, Barker JL, et al. Olfactory neuroblastoma: The 22-year experience at one comprehensive cancer center. Head Neck. 2005;27:138–49. doi: 10.1002/hed.20127. [DOI] [PubMed] [Google Scholar]
- 5.Elkon D, Hightower SI, Lim ML, Cantrell RW, Constable WC. Esthesioneuroblastoma. Cancer. 1979;44:1087–94. doi: 10.1002/1097-0142(197909)44:3<1087::aid-cncr2820440343>3.0.co;2-a. [DOI] [PubMed] [Google Scholar]
- 6.Herr MW, Sethi RK, Meier JC, Chambers KJ, Remenschneider A, Chan A, et al. Esthesioneuroblastoma: An update on the massachusetts eye and ear infirmary and Massachusetts general hospital experience with craniofacial resection, proton beam radiation, and chemotherapy. J Neurol Surg B Skull Base. 2014;75:58–64. doi: 10.1055/s-0033-1356493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Howell MC, Branstetter BF, 4th, Snyderman CH. Patterns of regional spread for esthesioneuroblastoma. Am J Neuroradiol. 2011;32:929–33. doi: 10.3174/ajnr.A2401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hyams VJ, Batsakis JG, Michaels L. Tumors of the Upper Respiratory Tract and Ear, Atlas of Tumor Pathology. Vol. 25. Washington DC: Armed Forces Institute Press; 1988. Olfactory neuroblastoma; pp. 240–8. [Google Scholar]
- 9.Kadish S, Goodman M, Wang CC. Olfactory neuroblastoma. A clinical analysis of 17 cases. Cancer. 1976;37:1571–6. doi: 10.1002/1097-0142(197603)37:3<1571::aid-cncr2820370347>3.0.co;2-l. [DOI] [PubMed] [Google Scholar]
- 10.Lester D, Thompson R. Olfactory Neuroblastoma. Head Neck Pathol. 2009;3:252–9. doi: 10.1007/s12105-009-0125-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Loy AH, Reibel JF, Read PW, Thomas CY, Newman SA, Jane JA, et al. Esthesioneuroblastoma: Continued follow-up of a single institution's experience. Arch Otolaryngol Head Neck Surg. 2006;132:134–8. doi: 10.1001/archotol.132.2.134. [DOI] [PubMed] [Google Scholar]
- 12.McElroy EA, Jr, Buckner JC, Lewis JE. Chemotherapy for advanced esthesioneuroblastoma: The Mayo Clinic experience. Neurosurgery. 1998;42:1023. doi: 10.1097/00006123-199805000-00040. [DOI] [PubMed] [Google Scholar]
- 13.Miller DC, Goodman ML, Pilch BZ, Shi SR, Dickersin GR, Halpern H, et al. Mixed olfactory neuroblastoma and carcinoma. A report of two cases. Cancer. 1984;54:2019–28. doi: 10.1002/1097-0142(19841101)54:9<2019::aid-cncr2820540940>3.0.co;2-p. [DOI] [PubMed] [Google Scholar]
- 14.Morita A, Ebersold MJ, Olsen KD, Foote RL, Lewis JE, Quast LM. Esthesioneuroblastoma: Prognosis and management. Neurosurgery. 1993;32:706. doi: 10.1227/00006123-199305000-00002. [DOI] [PubMed] [Google Scholar]
- 15.Sato Y, Handa T, Orita Y, Hirokawa M, Tsukayama C. A case report of mixed olfactory neuroblastoma- Neuroblastoma and adenocarcinoma. Kawasaki Med J. 1997;23:55–9. [Google Scholar]
- 16.Spaulding CA, Kranyak MS, Constable WC, Stewart FM. Esthesioneuroblastoma: A comparison of two treatment eras. Int J Radiat Oncol Biol Phys. 1988;15:581–90. doi: 10.1016/0360-3016(88)90298-2. [DOI] [PubMed] [Google Scholar]
- 17.Tseng J, Michel MA, Loehrl TA. Peripheral cysts: A distinguishing feature of esthesioneuroblastoma with intracranial extension. Ear Nose Throat. 2009;88:E14. [PubMed] [Google Scholar]
- 18.Wenig BM., ed . Atlas of Head and Neck Pathology. 3rd ed. Philadelphia: Elsevier, Inc; 2016. Neoplasms of the sinonasal tract; pp. 148–55. [Google Scholar]
- 19.Zanation AM, Ferlito A, Rinaldo A, Gore MR, Lund VJ, McKinney KA, et al. When, how and why to treat the neck in patients with esthesioneuroblastoma: A review. Eur Arch Otorhinolaryngol. 2010;267:1667–71. doi: 10.1007/s00405-010-1360-6. [DOI] [PMC free article] [PubMed] [Google Scholar]


