Abstract
Context:
Literature is inconsistent about the role of gender in mediating the relationship between life events and depression.
Aim:
Our objective was to explore gender differences in patterns and frequencies of stressful life events before onset of a depressive episode.
Setting and Design:
Cross-sectional study at a tertiary care center.
Subjects and Methods:
One hundred patients fulfilling Diagnostic and Statistical Manual of Mental Disorders fourth edition criteria for current major depression (50 males and 50 females) were recruited for the study. Structured instruments were used to assess psychiatric comorbidity, episode severity, and stressful life events. We compared the number and frequency of stressful life events between genders and their relationship with demographic and clinical variables.
Statistical Analysis Used:
Mann–Whitney U-test and Chi-square test.
Results:
Women with depression were older, more likely to be married (P < 0.01), had lower rates of comorbid panic disorder (P < 0.01) and nicotine dependence (P = 0.016) compared to men. Total stress scores and median number of stressful events in the year before onset of depression were significantly lower in women (P < 0.01). Getting married, job or property-related stressors, and breakup of friendship were more commonly reported stressors among males while more females reported dowry-related issues before symptom onset. In stratified analysis, these gender differences continued to hold good only in those with comorbid dysthymia.
Conclusion:
There appears to be a sex-specific effect of certain life events on depression. Comorbid dysthymia may play an important role in mediating this differential stress sensitivity across genders.
Keywords: Depression, dysthymia, gender, life events, psychiatry, stress
INTRODUCTION
Ever since the pioneering work of Brown et al.[1,2,3,4] was first published, life events have been shown to significantly influence the onset and course of depression. Stressful life events are strongly associated with the first onset of depression[5,6] and this association has been observed from adolescence onward.[7,8] This may be due to a neurobiological process, first postulated by Post,[9] in which exposure to stressful events before an index depressive episode causes sensitization (“kindling”) at the neuronal level, leaving the patient with a vulnerability to develop further episodes of depression even in the absence of a significant stressor.
Among the numerous factors that mediate the relationship between stressful events and depression, gender occupies an important place. From an early age, women appear to be more sensitive to the “depressogenic” effects of life stressors, to develop depression at lower levels of stress,[8,10] and to show exaggerated neuroendocrine responses to stress.[11] However, other researchers have obtained results that are at variance with these theories. For example, some studies have found no differences in stressful exposures across genders in patients with depression,[12] no differences in stressful life events in men and women presenting with a first depressive episode,[13] and weaker evidence for a “kindling” effect in women than in men.[6]
A possible explanation for these inconsistent results was suggested by a large study of twin pairs which found that conflicts with significant others were linked to depression more frequently in women, while divorce, separation, and work problems were more associated with depression in men.[14] These results highlight the fact that “stressors” or “life events” are not a single entity: There are many different kinds of stressful events, and specific types of events probably have gender- and context-specific effects. There is little research on the impact of life stressors on depression in cultures such as India, where the social context of both stress and depression is likely to be different from that of the above studies. One study found that there was a significant effect of gender on the nature of stressors reported before an episode.[15]
The current study aims to build on this literature by examining the frequencies and relationships of various forms of stressful events in a sample of 100 patients with a diagnosis of depression, presenting to a general hospital psychiatry unit in India. We hypothesized that there would be a gender-specific pattern of specific life events preceding the onset of a depressive episode in these patients.
SUBJECTS AND METHODS
The study subjects were male and female adult patients (n = 100; 50 of each sex; age range 18–60 years) fulfilling the Diagnostic and Statistical Manual of Mental Disorders fourth edition text revision criteria for current major depression.[16] Patients were recruited consecutively from the in- and out-patient services of a general hospital psychiatry unit in Puducherry, South India. The study was approved by the Institute Ethics Committee. After explaining the rationale of the study to patients and their caregivers, written informed consent was obtained from them. The diagnosis of depression was confirmed using the Mini International Neuropsychiatric Interview,[17] which was also used to assess comorbid psychiatric diagnoses. The severity of depressive symptoms was rated using the 17-item version of the Hamilton Rating Scale for Depression,[18] and concomitant anxiety was assessed using the Hamilton Rating Scale for Anxiety.[19]
As the nature and frequency of specific stressful life events varies across cultural contexts, we used the presumptive stressful life events scale (PSLES), an Indian adaptation of Holmes and Rahe's Stress Scale,[20] to examine all life events experienced by our patients in the year prior to the onset of their depressive episode. The PSLES lists 51 events that can be considered stressful in the Indian setting and assigns a score in terms of life change units to each event as in the Holmes and Rahe scale. Patients’ socioeconomic status was assessed using the modified Kuppuswamy classification, a tool developed in the Indian context which assesses socioeconomic status as a composite of three variables education, occupation, and monthly income. Based on the scores obtained, patients are classified into one of five “classes:” Upper, upper middle, lower middle, lower upper or upper.[21]
Our primary analysis was the comparison of number and frequency of stressful events, and the total PSLES score, across genders. In secondary analyses, we also examined the relationship of specific stressors with episode number, comorbidity, symptom profile, and genetic loading for depression and related “spectrum” conditions. All tests were two-tailed, and a value of P < 0.05 was considered statistically significant.
RESULTS
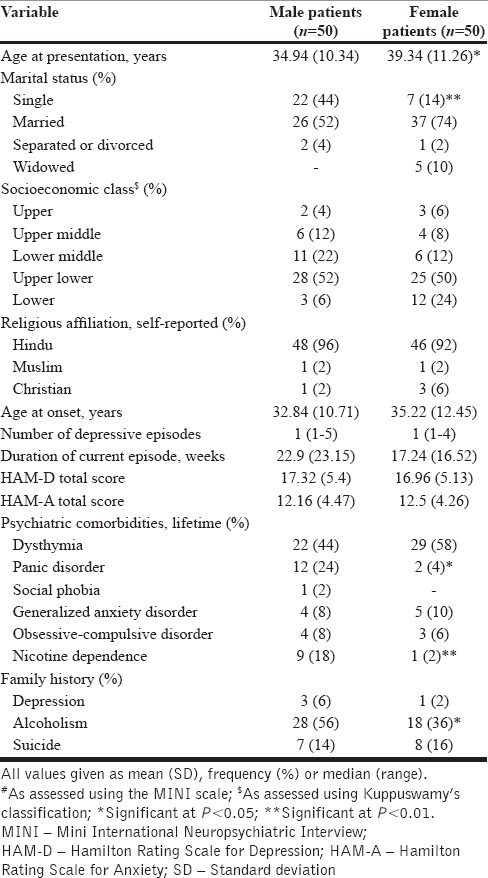
The study sample consisted of one hundred patients: 50 men and 50 women. Baseline demographic and clinical characteristics of the sample are given in Table 1. Women with depression were more likely to be married (χ2 = 15.01, P < 0.01) and were older than men at presentation (t = −2.04, P = 0.045). The majority of patients (76% of men and 62% of women) were in their first episode of depression, and the two groups were comparable in terms of clinician-rated severity of depressive and anxiety symptoms. A significant proportion of both men and women fulfilled criteria for a diagnosis of dysthymia prior to the onset of depression. Male patients were more likely to have comorbid panic disorder (P < 0.01, Fisher's exact test) and nicotine dependence (P = 0.016, Fisher's exact test).
Table 1.
Demographic and clinical characteristics of patients with major depression
The total PSLES score, measured in life change units similar to Holmes and Rahe's, was significantly lower in women than in men (mean 476.78 ± 158.81 in men, 390.96 ± 166.07 in women; t = 2.702, P < 0.01). There was a significant negative correlation between age and the total PSLES score (r = −0.283, P < 0.01). To control for this, an analysis of covariance was performed taking age as the covariate; this revealed that both sex (F = 4.92, P = 0.029) and age (F = 6.1, P = 0.015) were significantly related to the PSLES total score. There was no significant difference in PSLES scores between patients experiencing a first episode of depression (n = 69, mean 436.05 ± 170.38) and those with recurrent depression (n = 31, mean 432.19 ± 163.89; t = −0.106, P = NS).
The frequencies of the 51 specific types of life events listed in the PSLES in our sample are given in Table 2. Certain events, such as no. 21 (pregnancy of one's spouse) and no. 50 (a man's wife starts or stops working outside the home) could, by definition, be assessed only in male patients. The events that were significantly more likely to be prior to a depressive episode, in men, were: Damage to one's property or crops, conflict at the workplace, unemployment, the break-up of friendship, attending an interview for a job, and getting married or engaged. Women were significantly more likely to report problems related to dowry prior to the onset of depression.
Table 2.
Stressful life events reported by patients with depression
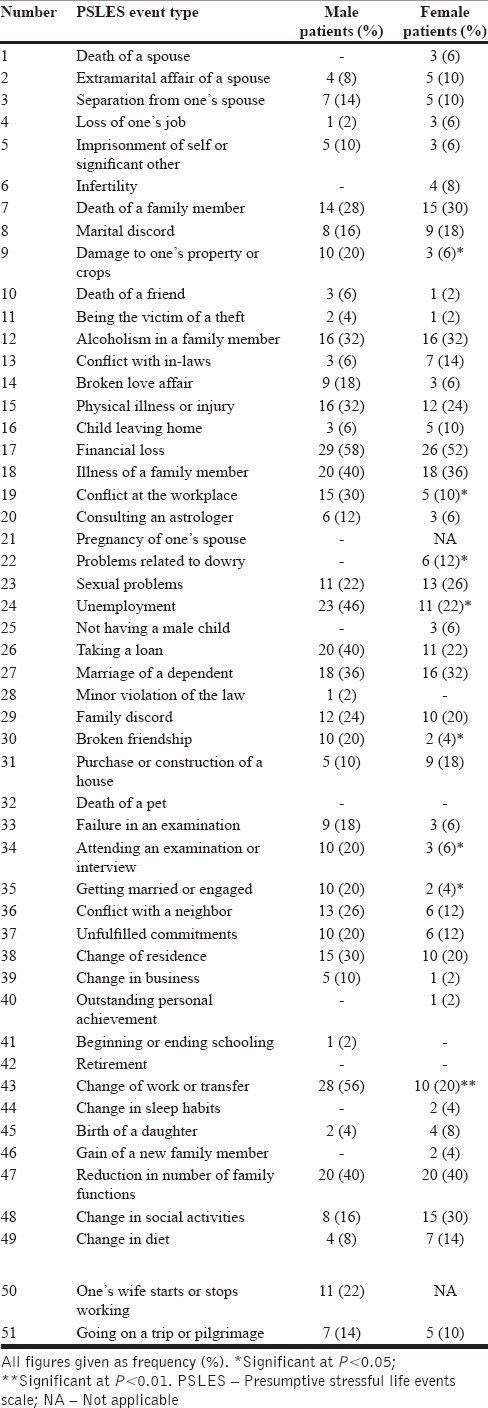
The median number of stressful life events reported in the year prior to the onset of depression was 8 (range 1–17), and was significantly higher in men than in women (Mann–Whitney U = 797.5, P < 0.01), but did not differ significantly between patients with a first episode of depression and recurrent depression (Mann–Whitney U = 1097.0, P = NS).
We also examined the relationships between the events listed in the PSLES and whether the patient presented with the first episode of depression, or with recurrent depression. Family discord was more frequent in recurrent depression (11/31 vs. 11/69 with a first episode; χ2 = 4.76, P = 0.029), but no specific kind of event was more frequent in patients with a first episode.
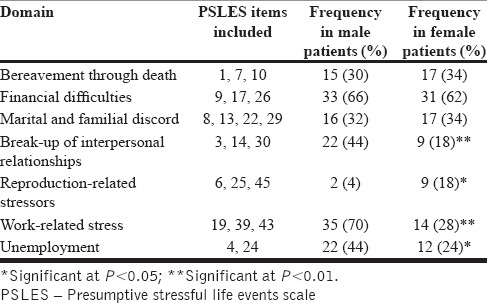
We also attempted to group life events according to common themes, as shown in Table 3. For example, items 1, 7, and 10 were grouped together as they all dealt with bereavement through death. Items 9, 17, and 26 all dealt with financial loss and were considered together. Other groupings, and the items comprising them, are given in the table. Using the above groupings, it was noted that break-ups in significant relationships, such as love affairs or friendships, were significantly more common in men, as were work-related stressors and unemployment. On the other hand, reproduction-related stressors, such as infertility or concerns about the gender of one's children, were more frequently reported by depressed women.
Table 3.
“Higher-order” groupings of stressful life events and their frequencies according to gender
As a potential confounding factor in our sample was the high rate (51%) of comorbid dysthymia, we repeated the above analyses excluding patients with this diagnosis. In the remaining patients (n = 49, 28 men and 21 women), we did not find a significant effect of either gender or episode number (first versus recurrent) on the total PSLES scores (P = NS for both comparisons). We were also unable to replicate the associations between gender and specific types of life events noted in Table 2, and we did not find any association between specific life events and the onset of the first episode of depression.
Conversely, we performed a subgroup analysis including only patients with dysthymia (n = 51, 22 men and 29 women). In this subset of patients, needing to take a loan (χ2 = 4.84, P = 0.028), getting married or engaged (P < 0.01, Fisher's exact test), and changes or transfers at work (χ2 = 19.45, P < 0.01) were more frequently reported by men; no specific life event was more frequently seen in women. More importantly, the median total number of stressors (Mann–Whitney U = 144.5, P < 0.01) and the total PSLES score (Mann–Whitney U = 156.0, P < 0.01) were significantly lower in women than in men with both dysthymia and depression.
Finally, we also examined if the presence or absence of comorbid dysthymia influenced the occurrence of specific life events prior to the onset of depression. We found that conflicts with neighbors (item 36; χ2 = 8.42, P < 0.01) and changes or transfers at work (item 43; χ2 = 4.92, P = 0.027) were less frequent in patients with comorbid dysthymia and depression, but no life event was more common in those with dysthymia. The presence or absence of dysthymia had no significant impact on the total PSLES score (t = 0.98, P = NS) or the number of stressors reported (Mann–Whitney U = 1061.5, P = NS).
DISCUSSION
Stressful life events were common in our sample of patients, with all patients reporting at least one such event in the year prior to the onset of their current depressive episode. The most frequent life events reported in our sample were financial loss (55%), illness of a family member (36%), and unemployment (34%). Except for the latter, which was more often reported by men, frequencies of the most common stressful events were comparable across genders. Given the high number of homemakers (26 of 50) in our group of women, even the latter difference may be an artefact of the sample's composition.
Both the total stress score, as measured using the PSLES, and the number of life events endorsed by patients were significantly higher in men than in women. This is in accordance with the hypothesis that women may be more sensitive than men to a “depressogenic” effect (a proneness to develop a depressive episode) of stress, and may, therefore, develop depression even at lower levels of exposure to stressful events.[8,10,22] However, when we corrected for the effects of dysthymia, the gender difference in stress exposure was evident only between men and women with this comorbidity; in those without dysthymia, no significant difference in PSLES scores or number of stressors was identified. This result provides partial support for a model known as the cognitive scar hypothesis, in which preexisting depressive symptoms increase an individual's cognitive vulnerability to develop syndromal depression in the face of stress.[23] A tentative interpretation of this data is that dysthymia lowers the threshold at which stress can trigger depression more significantly in women than in men.
In keeping with previous results,[14,15] we found that specific types of life event were more likely to precede depression in each gender. Events related to reproduction, such as infertility, were more common in women. This finding must be understood in the light of the sociocultural realities faced by our patients, who often experience a loss of status and stigmatization if they are unable to bear children, or if they have daughters rather than sons. An unexpected finding was the association between getting married or engaged, and the onset of depression in male patients, especially given that marriage is generally considered to be a protective factor against depression in men.[24] However, this association could only be confirmed in men who had comorbid dysthymia. It is possible that men with dysthymia may have had difficulties in coping with the emotional demands of marriage,[25] triggering a full-blown depressive episode.
We did not find a significant difference in total stress scores or number of life events between patients with a first episode of depression and those with recurrent episodes. However, this should not be taken as a refutation of the “kindling” hypothesis, as first episodes were overrepresented in our sample (69%) and very few patients had more than two episodes. Alternately, our study may have lacked the statistical power to demonstrate this phenomenon, which is more evident in large samples.[26]
Our results are subject to certain limitations. First, due to the cross-sectional nature of our study, information on stressful life events was obtained retrospectively and may have been incomplete or biased. Second, we only examined those life events listed in the PSLES; we did not consider other forms of severe stress, such as domestic violence, which have been shown to influence depression in our particular social and cultural context.[27,28] Third, we did not examine the effect of more remote stressful events, such as childhood trauma, which may affect an individual's sensitivity to stressors in adult life.[29] Fourth, we did not assess psychological variables, such as neuroticism[30] which may mediate the relationship between stressors and depression. Fifth, we did not examine the role of potential protective factors, such as coping skills[31] or social support.[32] Finally, due to the exploratory nature of our study, we did not correct our results for multiple comparisons, leading to the possibility of a type I error.
CONCLUSION
The study replicates previous findings about the differential effects of specific kinds of life events on depression in men and women, confirming that these effects are largely independent on the social context. In addition, we were also able to identify certain gender-specific stressors, such as reproduction-related events and dowry disputes that are peculiar to our own culture. Interestingly, we have demonstrated that the presence of subsyndromal (dysthymic) symptoms had a significant effect on stress sensitivity and that this effect is gender-specific to some extent. Whether the aggressive management of dysthymia may preempt the development of depression among women is a question that needs to be addressed through longitudinal study designs in future.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Brown GW, Harris TO, Peto J. Life events and psychiatric disorders part 2: Nature of causal link. Psychol Med. 1973;3:159–76. doi: 10.1017/s0033291700048492. [DOI] [PubMed] [Google Scholar]
- 2.Brown GW, Harris T, Copeland JR. Depression and loss. Br J Psychiatry. 1977;130:1–18. doi: 10.1192/bjp.130.1.1. [DOI] [PubMed] [Google Scholar]
- 3.Brown GW, Ní Bhrolcháin M, Harris TO. Psychotic and neurotic depression. Part 3. Aetiological and background factors. J Affect Disord. 1979;1:195–211. doi: 10.1016/0165-0327(79)90005-3. [DOI] [PubMed] [Google Scholar]
- 4.Finlay-Jones R, Brown GW. Types of stressful life event and the onset of anxiety and depressive disorders. Psychol Med. 1981;11:803–15. doi: 10.1017/s0033291700041301. [DOI] [PubMed] [Google Scholar]
- 5.Paykel ES. Life events and affective disorders. Acta Psychiatr Scand Suppl. 2003;418:61–6. doi: 10.1034/j.1600-0447.108.s418.13.x. [DOI] [PubMed] [Google Scholar]
- 6.Stroud CB, Davila J, Moyer A. The relationship between stress and depression in first onsets versus recurrences: A meta-analytic review. J Abnorm Psychol. 2008;117:206–13. doi: 10.1037/0021-843X.117.1.206. [DOI] [PubMed] [Google Scholar]
- 7.Carter JS, Garber J. Predictors of the first onset of a major depressive episode and changes in depressive symptoms across adolescence: Stress and negative cognitions. J Abnorm Psychol. 2011;120:779–96. doi: 10.1037/a0025441. [DOI] [PubMed] [Google Scholar]
- 8.Bouma EM, Ormel J, Verhulst FC, Oldehinkel AJ. Stressful life events and depressive problems in early adolescent boys and girls: The influence of parental depression, temperament and family environment. J Affect Disord. 2008;105:185–93. doi: 10.1016/j.jad.2007.05.007. [DOI] [PubMed] [Google Scholar]
- 9.Post RM. Transduction of psychosocial stress into the neurobiology of recurrent affective disorder. Am J Psychiatry. 1992;149:999–1010. doi: 10.1176/ajp.149.8.999. [DOI] [PubMed] [Google Scholar]
- 10.Kendler KS, Kuhn J, Prescott CA. The interrelationship of neuroticism, sex, and stressful life events in the prediction of episodes of major depression. Am J Psychiatry. 2004;161:631–6. doi: 10.1176/appi.ajp.161.4.631. [DOI] [PubMed] [Google Scholar]
- 11.Oldehinkel AJ, Bouma EM. Sensitivity to the depressogenic effect of stress and HPA-axis reactivity in adolescence: A review of gender differences. Neurosci Biobehav Rev. 2011;35:1757–70. doi: 10.1016/j.neubiorev.2010.10.013. [DOI] [PubMed] [Google Scholar]
- 12.Roca M, Gili M, Garcia-Campayo J, Armengol S, Bauza N, García-Toro M. Stressful life events severity in patients with first and recurrent depressive episodes. Soc Psychiatry Psychiatr Epidemiol. 2013;48:1963–9. doi: 10.1007/s00127-013-0691-1. [DOI] [PubMed] [Google Scholar]
- 13.Bukh JD, Bock C, Vinberg M, Gether U, Kessing LV. Gender differences among patients with a single depressive episode. Psychopathology. 2010;43:159–69. doi: 10.1159/000288638. [DOI] [PubMed] [Google Scholar]
- 14.Kendler KS, Thornton LM, Prescott CA. Gender differences in the rates of exposure to stressful life events and sensitivity to their depressogenic effects. Am J Psychiatry. 2001;158:587–93. doi: 10.1176/appi.ajp.158.4.587. [DOI] [PubMed] [Google Scholar]
- 15.Deshpande SS, Kalmegh B, Patil PN, Ghate MR, Sarmukaddam S, Paralikar VP. Stresses and disability in depression across gender. Depress Res Treat 2014. 2014:735307. doi: 10.1155/2014/735307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, (DSM-IV). Text Revision. Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- 17.Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, et al. The mini-international neuropsychiatric interview (M.I.N.I): The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59(Suppl 20):22–33. [PubMed] [Google Scholar]
- 18.Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hamilton M. The assessment of anxiety states by rating. Br J Med Psychol. 1959;32:50–5. doi: 10.1111/j.2044-8341.1959.tb00467.x. [DOI] [PubMed] [Google Scholar]
- 20.Singh G, Kaur D, Kaur H. Presumptive stressful life events scale (psles) – A new stressful life events scale for use in India. Indian J Psychiatry. 1984;26:107–14. [PMC free article] [PubMed] [Google Scholar]
- 21.Bairwa M, Rajput M, Sachdeva S. Modified Kuppuswamy's socioeconomic scale: Social researcher should include updated income criteria, 2012. Indian J Community Med. 2013;38:185–6. doi: 10.4103/0970-0218.116358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Maciejewski PK, Prigerson HG, Mazure CM. Sex differences in event-related risk for major depression. Psychol Med. 2001;31:593–604. doi: 10.1017/s0033291701003877. [DOI] [PubMed] [Google Scholar]
- 23.Nolen-Hoeksema S, Girgus JS, Seligman ME. Predictors and consequences of childhood depressive symptoms: A 5-year longitudinal study. J Abnorm Psychol. 1992;101:405–22. doi: 10.1037//0021-843x.101.3.405. [DOI] [PubMed] [Google Scholar]
- 24.Simon RW. Revisiting the relationships among gender, marital status, and mental health. AJS. 2002;107:1065–96. doi: 10.1086/339225. [DOI] [PubMed] [Google Scholar]
- 25.Subodh BN, Avasthi A, Chakrabarti S. Psychosocial impact of dysthymia: A study among married patients. J Affect Disord. 2008;109:199–204. doi: 10.1016/j.jad.2007.11.006. [DOI] [PubMed] [Google Scholar]
- 26.Kendler KS, Thornton LM, Gardner CO. Stressful life events and previous episodes in the etiology of major depression in women: An evaluation of the “kindling” hypothesis. Am J Psychiatry. 2000;157:1243–51. doi: 10.1176/appi.ajp.157.8.1243. [DOI] [PubMed] [Google Scholar]
- 27.Trivedi JK, Mishra M, Kendurkar A. Depression among women in the South-Asian region: The underlying issues. J Affect Disord. 2007;102:219–25. doi: 10.1016/j.jad.2006.09.024. [DOI] [PubMed] [Google Scholar]
- 28.Zahidie A, Jamali T. An overview of the predictors of depression among adult Pakistani women. J Coll Physicians Surg Pak. 2013;23:574–80. [PubMed] [Google Scholar]
- 29.Young E, Korszun A. Sex, trauma, stress hormones and depression. Mol Psychiatry. 2010;15:23–8. doi: 10.1038/mp.2009.94. [DOI] [PubMed] [Google Scholar]
- 30.Goodwin RD, Gotlib IH. Gender differences in depression: The role of personality factors. Psychiatry Res. 2004;126:135–42. doi: 10.1016/j.psychres.2003.12.024. [DOI] [PubMed] [Google Scholar]
- 31.Wilhelm K, Parker G, Dewhurst J. Examining sex differences in the impact of anticipated and actual life events. J Affect Disord. 1998;48:37–45. doi: 10.1016/s0165-0327(97)00138-9. [DOI] [PubMed] [Google Scholar]
- 32.Dalgard OS, Dowrick C, Lehtinen V, Vazquez-Barquero JL, Casey P, Wilkinson G, et al. Negative life events, social support and gender difference in depression: A multinational community survey with data from the ODIN study. Soc Psychiatry Psychiatr Epidemiol. 2006;41:444–51. doi: 10.1007/s00127-006-0051-5. [DOI] [PubMed] [Google Scholar]


