Figure 1.
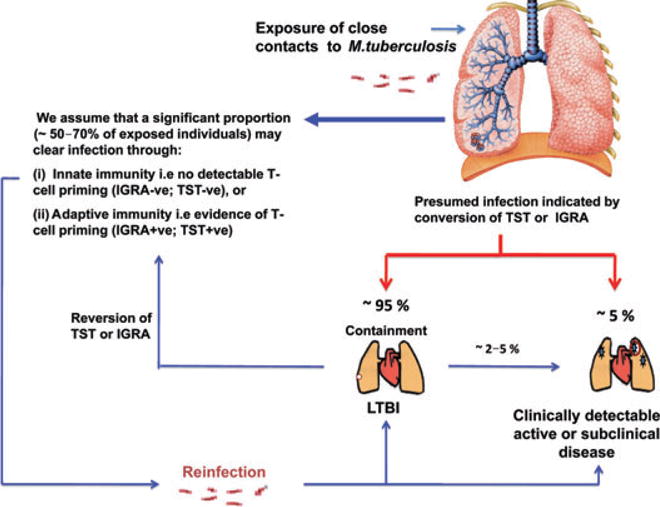
The spectrum of Mycobacterium tuberculosis infection and the life cycle of M. tuberculosis. Many exposed individuals (~30–50%) have no immunodiagnostic evidence of M. tuberculosis infection or T-cell priming despite heavy exposure to M. tuberculosis. These individuals, although unproven, may be innately resistant to M. tuberculosis infection. Of those who have immunodiagnostic evidence of T-cell priming (+ve TST or IGRA) it is likely that a substantial proportion have LTBI (clinically asymptomatic M. tuberculosis infection during which organisms are in a state of non-replicating persistence). Some individuals have transiently positive responses, and may subsequently ‘revert’ their reactions—they may have ‘acute resolving infection’ or clear their infection. These individuals may become reinfected and progress to active tuberculosis. A proportion of patients with LTBI may also progress to active disease. Given the lack of a gold diagnostic standard for LTBI some of these postulates are based on circumstantial evidence and remain unproven. A multitude of clinical conditions (HIV-1 infection, diabetes mellitus, malnutrition, tobacco smoking, TNF-α inhibitor therapy, helminth coinfection) may permit tipping of the immunological balance and promote transition from latent infection to active disease. IGRA, interferon-γ release assay; LTBI, latent tuberculosis infection; TNF-α, tumour necrosis factor-α; TST, tuberculin skin test.
