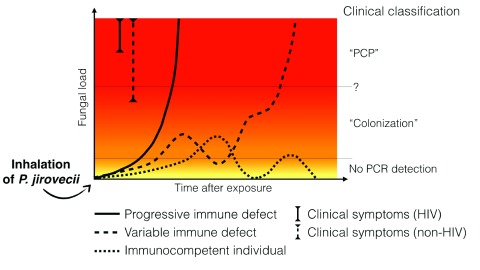
Figure 1. The variable evolution of Pneumocystis fungal load after exposure depending on the host’s immune status.
Upon exposure, P. jirovecii multiplies at the surface of type I pneumocytes in the alveoli. At the very beginning of the infection, quantitative polymerase chain reaction (qPCR) may not be positive owing to very low or localized multiplication of P. jirovecii, even if a bronchoalveolar lavage (the most sensitive specimen) is performed. Depending on the host’s immune status, the evolution of the fungal load could differ: - Rapid and constant multiplication of P. jirovecii leading to Pneumocystis pneumonia (PCP) is typically observed in HIV patients or in patients under immunosuppressive regimens (regular line). The situation known as “PCP” is observed when a high fungal load is associated with symptoms. Note that symptoms appear for lower fungal loads in non-HIV patients compared to HIV patients. - Variable fungal load above or below the detection’s threshold is observed in patients with variable immune status with PCP occurring when immunosuppression increases. This situation is typically seen in hematology or cancer patients submitted to several courses of chemotherapy (dashed line). PCR detection in asymptomatic patients in the situation known as “colonization” could correspond to patients controlling the disease (decreasing fungal load) or to patients who will develop PCP in the near future. The threshold between PCP and “colonization” may be different in HIV-positive and HIV-negative patients. - Immunocompetent patients are potentially a reservoir of P. jirovecii with low multiplication rate due to rapid immune control and subsequent decrease of fungal load. Re-infection with a new genotype or reactivation could occur later on (dotted line).