Continuation of Figure 2:
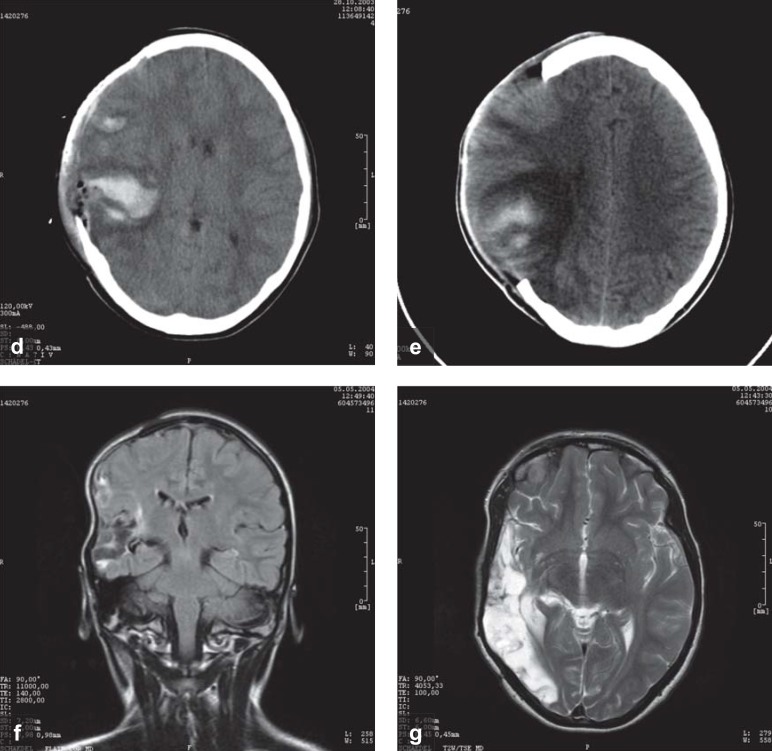
and e) Two weeks later, follow-up CTs show persistent brain swelling, with incipient resorption of the hemorrhagic contusion.
and g) Six months later, before the skull flap was surgically reinserted, follow-up MRI shows a large right temporo-occipital tissue defect. At this time, the patient has a moderately severe left visual field defect, but no other neurological deficits. She is back at school in her Gymnasium (academically-oriented German secondary school): she is reportedly doing poorly in mathematics and has difficulty with spatial processing, but her language ability is above average. Coma and pupillary areflexia at the time of the injury are best explained as reflecting acute, but reversible brainstem dysfunction, due to the pressure that was exerted mainly by the swelling of the brain contusion and, to a lesser extent, by the subdural hematoma. The mass effect was rapidly and successfully reduced by hemicraniectomy, preventing irreversible structural damage to the brainstem.