Abstract
Background:
Knee malalignment is an important modifiable cause of osteoarthritis (OA). Surgical therapeutic procedures depend on proper knee alignment assessment. The purpose of this study was to compare knee alignment parameters between double and single leg weight-bearing radiographs and to evaluate the reproducibility of inter- and intra-observer measurements.
Methods:
One hundred eight patients (59 male and 49 female) with knee deformity visited at Kerman Knee Clinic were selected. Full limb anteroposterior (AP) Radiographs were taken for each participant in double and single leg weight-bearing positions. Hip-Knee-Ankle Angle (HKAA), Medial-Proximal-Tibial Angle (MPTA), Lateral-Distal-Femoral Angle (LDFA) and Joint-Line-Convergence Angle (JLCA) measured. Images stored on PC were examined by three observers to assess inter and intra observer reproducibility. Data analysis was done by SPSS software.
Results:
The mean age of patients was 48.4 (±6.84) years, mean BMI was 26.55 (±1.94) Kg/m2. The mean HKAA and JLCA were significantly different between double and single leg weight-bearing radiographs. Intraclass correlation coefficient (ICC) test showed high (0.99) inter-reproducibility between three observers in all cases, except one (ICC=0.92). Intra-observer reproducibility indicated a strong correlation between the observer’s measurements at different times (ICC > 0.99).
Conclusion:
HKAA and JLCA were affected by the patient’s position. Observer and time interval had no effect on either of HKAA, MPTA, LDFA, and JLCA. Also the measurement of knee alignment parameters was not dependent on observer’s experience. In conclusion single leg weight-bearing radiography is more representative of knee alignment and is inter and intra-observer reproducible.
Keywords: Knee Alignment, Osteoarthritis, Radiography, Reliability
Introduction
Osteoarthritis (OA) as one of five leading causes of disability among non-institutionalized adults, affects more than 20 million individuals in the United States (1, 2). Varus and valgus alignment of the lower limb accelerate degenerative changes and knee OA progression (3-8). Knee malalignment can be modified surgically (9, 10) but a meticulous analysis of the deformity has to be achieved in order to define the type, size and site of deformity for optimized therapeutic planning, surgical technique, and postoperative follow-up (11). Radiographic examination, as a clinical assessment, is a fundamental tool for pre- and post-operative planning (12, 13).
The frontal plane alignment measures are the gold standard method to assess knee alignment in patients with OA. Usual clinical tool for this purpose is full limb anteroposterior (AP) radiograph of lower extremities while the patient is standing on both feet (7, 13, 14).
Several different parameters measured in knee radiographs. One of the most common used parameters is the load-bearing axis (mechanical axis of the lower extremity), a line drawn from center of femoral head to center of the ankle. The orientation of this axis reflects alignment in standing position, sincein a varus knee the line passes medial to the knee and in a valgus knee, the load-bearing axis passes lateral to the knee (12, 15).
Lower limb alignment depends on two geometry: the long bones and articulating surfaces of femur and tibia (16). Hip-Knee-Ankle Angle (HKAA) as the most common parameter that is measured by radiographs indicates the size of deformity. It is the angle formed by the intersection of a line from the center of femoral head to the center of the tibial spine and a second line from the center of talus to the center of the tibial spine. The normal HKAA is 180º, the angle greater than 180º represent a valgus deformity, and less than 180º a varus deformity (17, 18).
Medial Proximal Tibial Angle (MPTA), Lateral Distal Femoral Angle (LDFA) and Joint Line Convergence Angle (JLCA) determine alignment between tibial and femoral surfaces in weight-bearing position (12, 16). These angles are defined as follow; MPTA: The angle between the tibial mechanical axis and tibial joint line (line across the medial and lateral tibial plateaus) that is normally 87º. LDFA: The angle between the femoral mechanical axis and femoral joint line (line across the distal femoral condyles) that is normally 93º. JLCA: The angle between femoral and tibial joint line that is normally 0º - 2º, meaning they are almost parallel. Abnormal angle is due to asymmetric wear (12, 19-21).
The initiation of knee OA may be due to the femoral shaft curvature changes along with aging. The varus femoral condylar orientation, medial joint space narrowing, and tibial plateau compression are the secondary sign of OA progression (22).
During the stance phase of gait which encompasses sixty percent of the gait cycle, body weight supported by single leg (23). The mechanical axis angle is different in single-leg standing, double-leg standing, and supine positions (24).
In previous studies, lower limb axes and angles are drawn and measured on an AP radiograph which is taken while the patient is standing on both feet (3, 13, 22, 25, 26). Except for one study that compared and evaluated the reliability of mechanical axis between double and single leg weight-bearing (24), but other lower extremity alignment parameters have not been compared in weight bearing positions.
We designed this study to compare all four knee alignment parameters between double and single leg weight-bearing radiographs; and also to evaluate the reproducibility of inter- and intra-observer measurements.
Materials and Methods
Subjects
One hundred eight patients who had been visited at Kerman Knee Clinic, Kerman, Iran for knee deformity during Sep. 2012 to Oct. 2014 were selected. This study was approved by Kerman University of Medical Sciences Faculty of Medicine and the Committee of Ethics.
Anteroposterior (AP) full-limb radiograph (or Hip Knee Ankle) as the gold standard imaging modality for assessing lower limb alignment was used to determine knee deformity (varus or valgus) in patients who were clinically suspicious of knee malalignment (7). All the participants who attended in our study either had knee OA or were at high risk for developing knee OA. High risk individuals include who were overweight or obese, those with current knee pain and those with a history of knee injury or surgery. Exclusion criteria were rheumatoid arthritis, ankylosing spondylitis, psoriatic arthritis, Reiter’s syndrome, significant kidney disease, cancer, bilateral knee replacements, history of fracture, surgical treatment of OA (27). Eligible patients participated only if they gave the written informed consent to take another radiograph.
Radiographs
Antero-posterior full-limb radiographs in double leg weight-bearing position were taken with 130×36-cm graduated grid cassette to include the full limb of tall participants. The patients stood without footwear while their knees in full extension and tibial tubercles facing forward. The x-ray beam was centered at the knee with a setting of 100 to 300 mA/s and 80-90 kV, depending on limb size and tissue characteristics from 2.4m distance (7, 18).
Another radiograph was taken separately for each patient with above characteristic in a single leg weight-bearing position in which the patient raises one leg to put the weight completely on the malaligned knee.
Measurements
The digitalized images stored on a PC to be analyzed further using the software Medview Meddiag - ©MEDECOM – 3.0.4. This digital software provides minimal bios in placing points and drawing lines.
The following four parameters were determined on both radiographs for each patient. 1. HKA angle (HKAA) which was the angle between the femoral mechanical axis (a line from the center of the femoral head running distally to the mid-condylar point) and tibial mechanical axis (line from the center of the tibial plateau extending distally to the center of the tibial plafond). 2. MPTA was the angle between the tibial mechanical axis and tibial joint line. 3. LDFA was the angle between the mechanical femoral axis and femoral joint line. 4. JLCA was the angle between distal femoral joint line and proximal tibial joint line (7, 12).
We used Medview Meddiag software to measure the above-mentioned angles as follow:
The Observer put three points at femoral head borders and the software defined the circumscribed circle and the center of femoral head [Figure 1].
The observer pointed femoral inter condylar notch and outlined inter condylar tibial eminence [Figure 2].
After drawing inter malleolar line by observer [Figure 3], the software illustrated HKAA [Figure 4]
The Observer drew the tangent of femoral condyles and tibial plateau [Figure 4; 5] and the software outlined and measured all of the HKAA, MPTA, LDFA and JLCA on digital image [Figure 6]
Figure 1.
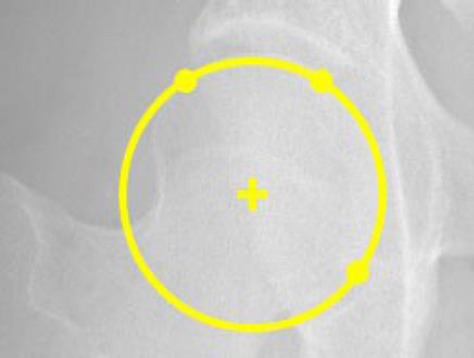
Defined the center of the femoral head.
Figure 2.
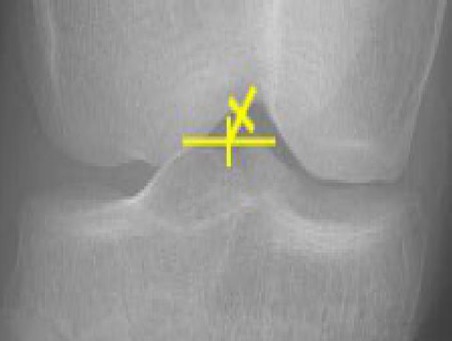
Intercondylar eminence of the tibia and Femoral intercondylar notch.
Figure 3.

Inter malleolar segment tangent.
Figure 4.
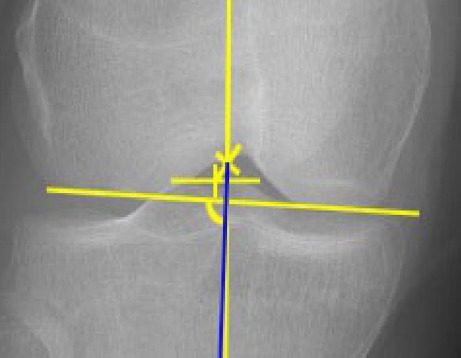
The tangent to the femoral condyles.
Figure 5.
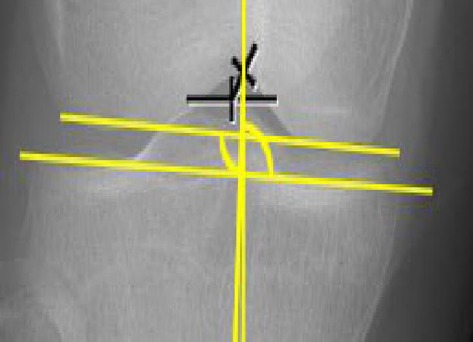
The tangent to the tibial plateau.
Figure 6.

HKAA: Hip Knee Ankle Angle, MPTA: Medial Proximal Tibial Angle, LDFA: Lateral Distal Femoral Angle, JLCA: Joint Line Convergence measured and displayed on digital image.
The reproducibility of this technique, was estimated by three distinct observers (an orthopedic surgeon with sixteen years of experience and two medical students trained in epidemiology and knee alignment) To assess inter-observer reproducibility, each radiograph measurement (single and double leg) was done by all three observers in a blind circumstance with no knowledge of prior results. Intra-observer reproducibility was evaluated in two independent measurements accomplished by the orthopedic surgeon for each patient within two weeks.
Statistical analysis
To evaluate changes in double and single leg standing angles, Paired t-test was used. The intra- and inter-observer reproducibility was assessed by means of intraclass correlation coefficient (ICC) (28). As explained before, each participant was measured 2 times by 3 observers and in 2 positions (12 observations per subjects). Taking into account the dependency of observations, linear mixed effects regression analysis was used to evaluate the effect of positions, observers, and time on measurements. The SPSS program statistical software was used for analysis. A P-value of less than 0.05 was considered to be statistically significant.
Results
One hundred and eight patients (59 male and 49 Female) were selected for this study. Their mean age was 48.4 (±6.84) years (range 31-60 years), mean body mass index (BMI) was 26.55 (±1.94) Kg/m2. Varus deformity was seen in 90.7% of patients.
According to Table 1, HKAA and JLCA were significantly different between double and single leg weight-bearing positions.
Table 1.
Comparison between single and double leg weight bearing radiography
| Paired Samples Test | |||||||
|---|---|---|---|---|---|---|---|
| Mean (degree) | Std. Deviation (degree) | Range (degree) | Mean | Std. Deviation | Std. Error | Sig. (2-tailed) | |
| HKAA1 | 8.80 | 4.97 | 0.30-24.83 | 0.76 | 3.13 | 0.30 | 0.01 |
| HKAA2 | 8.04 | 4.54 | 0.37-20.17 | ||||
| MPTA1 | 89.25 | 5.71 | 76.80-103.37 | 0.36 | 6.97 | 0.67 | 0.59 |
| MPTA2 | 88.89 | 9.32 | 19.50-102.43 | ||||
| LDFA1 | 90.34 | 3.53 | 79.73-98.77 | 0.20 | 2.32 | 0.22 | 0.38 |
| LDFA2 | 90.14 | 3.18 | 80.50-96.50 | ||||
| JLCA1 | 3.44 | 2.64 | 0.00-15.83 | 0.42 | 1.82 | 0.18 | 0.02 |
| JLCA2 | 3.02 | 2.38 | 0.07-11.63 | ||||
HKAA: Hip Knee Ankle Angle, MPTA: Medial Proximal Tibial Angle, LDFA: Lateral Distal Femoral Angle, JLCA: Joint Line Convergence Angle, 1: Stands for single leg, 2: stands for double leg weight-bearing Table 2. Linear regression for time, observer, and position effects
ICC test showed high inter-observer reproducibility between three observers in all angles. ICC was higher than 0.99 except for one (ICC=0.92). Intra-observer reproducibility demonstrated astrong correlation between the observer’s measurements at different times (ICC > 0.99).
We have seen that observer had no effect on any of four outcomes [Table 2]. For example, in terms of HKAA, the maximum difference seen between observers was as low as 8.37 and 8.49 which was far from being significant.
Table 2.
Linear regression for time, observer, and position effects
| Variable | Level | Mean | SE | P | |
|---|---|---|---|---|---|
| HKAA | Time | First Time | 8.40 | 0.44 | 0.98 |
| Second Time | 8.40 | 0.44 | |||
| Observer | Observer 1 | 8.40 | 0.44 | 1.00 | |
| Observer 2 | 8.49 | 0.44 | |||
| Observer 3 | 8.37 | 0.44 | |||
| Position | Standing on Single Leg | 8.80 | 0.44 | 0.00 | |
| Standing on Double Leg | 7.99 | 0.44 | |||
| MPTA | Time | First Time | 89.15 | 0.69 | 0.90 |
| Second Time | 89.20 | 0.69 | |||
| Observer | Observer 1 | 89.15 | 0.72 | 1.00 | |
| Observer 2 | 89.31 | 0.72 | |||
| Observer 3 | 88.75 | 0.72 | |||
| Position | Standing on Single Leg | 89.25 | 0.69 | 0.70 | |
| Standing on Double Leg | 89.11 | 0.69 | |||
| LDFA | Time | First Time | 90.26 | 0.31 | 0.76 |
| Second Time | 90.25 | 0.31 | |||
| Observer | Observer 1 | 90.22 | 0.31 | 1.00 | |
| Observer 2 | 90.30 | 0.31 | |||
| Observer 3 | 90.19 | 0.31 | |||
| Position | Standing on Single Leg | 90.33 | 0.31 | 0.14 | |
| Standing on Double Leg | 90.14 | 0.31 | |||
| JLCA | Time | First Time | 3.22 | 0.23 | 0.91 |
| Second Time | 3.21 | 0.23 | |||
| Observer | Observer 1 | 3.22 | 0.23 | 1.00 | |
| Observer 2 | 3.29 | 0.23 | |||
| Observer 3 | 3.19 | 0.23 | |||
| Position | Standing on Single Leg | 3.41 | 0.23 | 0.00 | |
| Standing on Double Leg | 3.02 | 0.23 | |||
HKAA: Hip Knee Ankle Angle, MPTA: Medial Proximal Tibial Angle, LDFA: Lateral Distal Femoral Angle, JLCA: Joint Line Convergence Angle
Table 2 illustrated that the time interval had no effect on the accuracy of evaluation of observer’s measurements. The maximum difference of angle measurements was 0.05 between first and second time [Table 2].
Using linear regression [Table 2] determined that HKAA and JLCA were different between double and single weight-bearing positions.
Discussion
The purpose of this study was to compare knee alignment parameters between double leg and single leg weight-bearing radiographs and to evaluate the reproducibility of inter- and intra-observer measurements.
Our demographic results revealed that the majority of our patients with knee alignment have high body mass index which was predictable. Gudbergsen et al. concluded that weight loss is effective for symptomatic relief in obese subjects with knee osteoarthritis (29). In the current study, the mean age of participants was above forty years old which is justified by pathophysiology of OA. Matsumoto et al. performed a study in 2015 indicated that aging was associated with the lateral curvature of femoral shaft changing in the initiation of varus type OA of the knee. Following these changes, secondary signs of OA progression including varus femoral condylar orientation, medial joint space narrowing, and tibial plateau compression arise (22). Advancing age causes reductions in cartilage volume, proteoglycan content, cartilage vascularization, and cartilage perfusion and is the major risk factor for osteoarthritis in association with biochemical factors as mentioned by American Association of Orthopedic Surgeons (30).
Overcorrection and under correction of knee deformity lead to inconvenience and persistent pain in patient’s knee (31). Accuracy in pre- and post-operative knee alignment radiography is an important factor that must be regarded. The gold standard modality for knee alignment assessment is full limb lower extremity radiography in double leg weight bearing position. The current study was focused on full limb radiography and also compared double versus single leg weight-bearing positions. Van Raaij et al. in 2009 investigated two methods of femorotibial measurement on short knee images compared to the gold standard HKA angle on a full-limb view. Although angleon short knee images was correlated with HKA angle on full limb radiographs (r=0.65), these methods demonstrated poor inter- and intra- observer agreement (ICC=0.37) (14). Several studies were conducted for assessing reproducibility of angle measurements in short and full-limbradiographs. In 2009, Colebatch et al. compared and assessed the reproducibility of knee axial alignment (HKA and FTA), on conventional AP knee and full-limb radiographs in healthy peoples. They suggested standard AP knee radiographs with proper reproducibility as a useful method for measuring knee alignment (18). But Sheehy et al. used the femoral shaft-tibial shaft angle (FS-TS) from short knee radiograph to estimate the HKA angle in OA patients. They recommended that use off ull-length radiograph for an accurate estimation of HKA angle because FS-TS angle depends on direction and degree of knee deformity (27). In this study, four knee alignment parameters (HKAA, MPTA, LDFA, and JLCA) in both radiographs were assessed by three observers. The Results showed accurate inter-observer reproducibility for all angles (ICC>0.916). Linear Regression results confirmed the reproducibility of the measurement by all three observers and indicated the independency of their experience (P>0.05). High intra-observer reproducibility was also obtained (ICC>0.999) and linear regression test confirmed the accuracy of time independency (P>0.05). These findings were consistent with the investigations of Matos et al. study. They evaluated inter and intra-observer analysis on measurements of the anatomical axis (FTA), as a fundamental element for assessing alignment of the lower limb, between AP full-limb and short film knee radiographs in OA patients. The results demonstrated that the methods for measuring the FTA on short and full limb radiographs were reliable and reproducible. In addition, observers experience had no impact on measurement results (13).
In the current study we demonstrated that HKAA and JLCA were significantly different between double and single leg weight-bearing positions. The linear regression analysis confirmed the effectiveness of the patient’s position on these angles (P=0.000). According to Table 1. HKAA and JLCA were higher in single leg weight-bearing position which was similar to findings in the study of Specogna et al. They found that HKAA measured on single leg weight-bearing radiography is more representative of dynamic joint load and further highlights the difference between dynamic and static measures (24). During dynamic activities, such as gait, or single-leg weight-bearing, the force line shifts medial to the knee joint center, therefore the compressive stress is increased in medial aspect. Followed by this change the angles are higher while the patient is standing on single leg and varus deformity is augmented in this position (32).
The measurement of Knee alignment parameters (HKAA, MPTA, LDFA, and JLCA) on both radiographs by three observers indicated high inter-observer reproducibility for all angles and it was not affected by observer’s experience. The results also showed high rate of intra-observer concordance and reproducibility. The present study found that HKA angle and JLC angle changed significantly in single leg versus double leg weight bearing position.
This research was supported by Neurology Research Center, Kerman University of Medical Sciences, Kerman, Iran.
The authors report no conflict of interest concerning the materials or methods used in this study or the findings specified in this paper.
References
- 1.Pereira D, Peleteiro B, Araujo J, Branco J, Santos RA, Ramos E. The effect of osteoarthritis definition on prevalence and incidence estimates:a systematic review. Osteoarthritis Cartilage. 2011;19(11):1270–85. doi: 10.1016/j.joca.2011.08.009. [DOI] [PubMed] [Google Scholar]
- 2.Murphy L, Helmick CG. The impact of osteoarthritis in the United States:a population-health perspective. Am J Nurs. 2012;112(3 Suppl 1):S13–9. doi: 10.1097/01.NAJ.0000412646.80054.21. [DOI] [PubMed] [Google Scholar]
- 3.Brouwer GM, van Tol AW, Bergink AP, Belo JN, Bernsen RM, Reijman M, et al. Association between valgus and varus alignment and the development and progression of radiographic osteoarthritis of the knee. Arthritis Rheum. 2007;56(4):1204–11. doi: 10.1002/art.22515. [DOI] [PubMed] [Google Scholar]
- 4.Cerejo R, Dunlop DD, Cahue S, Channin D, Song J, Sharma L. The influence of alignment on risk of knee osteoarthritis progression according to baseline stage of disease. Arthritis Rheum. 2002;46(10):2632–6. doi: 10.1002/art.10530. [DOI] [PubMed] [Google Scholar]
- 5.Cicuttini F, Wluka A, Hankin J, Wang Y. Longitudinal study of the relationship between knee angle and tibiofemoral cartilage volume in subjects with knee osteoarthritis. Rheumatology (Oxford) 2004;43(3):321–4. doi: 10.1093/rheumatology/keh017. [DOI] [PubMed] [Google Scholar]
- 6.Felson DT, Nevitt MC, Yang M, Clancy M, Niu J, Torner JC, et al. A new approach yields high rates of radiographic progression in knee osteoarthritis. J Rheumatol. 2008;35(10):2047–54. [PMC free article] [PubMed] [Google Scholar]
- 7.Sharma L, Song J, Felson DT, Cahue S, Shamiyeh E, Dunlop DD. The role of knee alignment in disease progression and functional decline in knee osteoarthritis. JAMA. 2001;286(2):188–95. doi: 10.1001/jama.286.2.188. [DOI] [PubMed] [Google Scholar]
- 8.Teichtahl AJ, Davies-Tuck ML, Wluka AE, Jones G, Cicuttini FM. Change in knee angle influences the rate of medial tibial cartilage volume loss in knee osteoarthritis. Osteoarthritis Cartilage. 2009;17(1):8–11. doi: 10.1016/j.joca.2008.05.013. [DOI] [PubMed] [Google Scholar]
- 9.Virolainen P, Aro HT. High tibial osteotomy for the treatment of osteoarthritis of the knee:a review of the literature and a meta-analysis of follow-up studies. Arch Orthop Trauma Surg. 2004;124(4):258–61. doi: 10.1007/s00402-003-0545-5. [DOI] [PubMed] [Google Scholar]
- 10.Karachalios T, Sarangi PP, Newman JH. Severe varus and valgus deformities treated by total knee arthroplasty. J Bone Joint Surg Br. 1994;76(6):938–42. [PubMed] [Google Scholar]
- 11.Moreland JR, Bassett LW, Hanker GJ. Radiographic analysis of the axial alignment of the lower extremity. J Bone Joint Surg Am. 1987;69(5):745–9. [PubMed] [Google Scholar]
- 12.Cooke TD, Sled EA, Scudamore RA. Frontal plane knee alignment:a call for standardized measurement. J Rheumatol. 2007;34(9):1796–801. [PubMed] [Google Scholar]
- 13.Matos LF, Giordano M, Cardoso GN, Farias RBE, Albuquerque RP. Comparative radiographic analysis on the anatomical axis in knee osteoarthritis cases:inter and intraobserver evaluation. Rev Bras Ortop. 2015;50(3):283–9. doi: 10.1016/j.rboe.2015.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.van Raaij TM, Brouwer RW, Reijman M, Bierma-Zeinstra SM, Verhaar JA. Conventional knee films hamper accurate knee alignment determination in patients with varus osteoarthritis of the knee. Knee. 2009;16(2):109–11. doi: 10.1016/j.knee.2008.10.003. [DOI] [PubMed] [Google Scholar]
- 15.Tetsworth K, Paley D. Malalignment and degenerative arthropathy. Orthop Clin North Am. 1994;25(3):367–77. [PubMed] [Google Scholar]
- 16.Cooke D, Scudamore A, Li J, Wyss U, Bryant T, Costigan P. Axial lower-limb alignment:comparison of knee geometry in normal volunteers and osteoarthritis patients. Osteoarthritis Cartilage. 1997;5(1):39–47. doi: 10.1016/s1063-4584(97)80030-1. [DOI] [PubMed] [Google Scholar]
- 17.Hsu RW, Himeno S, Coventry MB, Chao EY. Normal axial alignment of the lower extremity and load-bearing distribution at the knee. Clin Orthop Relat Res. 1990;255(1):215–27. [PubMed] [Google Scholar]
- 18.Colebatch AN, Hart DJ, Zhai G, Williams FM, Spector TD, Arden NK. Effective measurement of knee alignment using AP knee radiographs. Knee. 2009;16(1):42–5. doi: 10.1016/j.knee.2008.07.007. [DOI] [PubMed] [Google Scholar]
- 19.Yoshioka Y, Siu D, Cooke TD. The anatomy and functional axes of the femur. J Bone Joint Surg Am. 1987;69(6):873–80. [PubMed] [Google Scholar]
- 20.Chao EY, Neluheni EV, Hsu RW, Paley D. Biomechanics of malalignment. Orthop Clin North Am. 1994;25(3):379–86. [PubMed] [Google Scholar]
- 21.Pornrattanamaneewong C, Narkbunnam R, Chareancholvanich K. Medial proximal tibial angle after medial opening wedge HTO:A retrospective diagnostic test study. Indian J Orthop. 2012;46(5):525–30. doi: 10.4103/0019-5413.101042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Matsumoto T, Hashimura M, Takayama K, Ishida K, Kawakami Y, Matsuzaki T, et al. A radiographic analysis of alignment of the lower extremities--initiation and progression of varus-type knee osteoarthritis. Osteoarthritis Cartilage. 2015;23(2):217–23. doi: 10.1016/j.joca.2014.11.015. [DOI] [PubMed] [Google Scholar]
- 23.Vaughan CL. Theories of bipedal walking:an odyssey. J Biomech. 2003;36(4):513–23. doi: 10.1016/s0021-9290(02)00419-0. [DOI] [PubMed] [Google Scholar]
- 24.Specogna AV, Birmingham TB, Hunt MA, Jones IC, Jenkyn TR, Fowler PJ, et al. Radiographic measures of knee alignment in patients with varus gonarthrosis:effect of weightbearing status and associations with dynamic joint load. Am J Sports Med. 2007;35(1):65–70. doi: 10.1177/0363546506293024. [DOI] [PubMed] [Google Scholar]
- 25.McDaniel G, Mitchell KL, Charles C, Kraus VB. A comparison of five approaches to measurement of anatomic knee alignment from radiographs. Osteoarthritis Cartilage. 2010;18(2):273–7. doi: 10.1016/j.joca.2009.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Durandet A, Ricci PL, Saveh AH, Vanat Q, Wang B, Esat I, et al. Radiographic analysis of lower limb axial alignments. Proc World Cong Engin. 2013;2205(2):1354–8. [Google Scholar]
- 27.Sheehy L, Felson D, Zhang Y, Niu J, Lam YM, Segal N, et al. Does measurement of the anatomic axis consistently predict hip-knee-ankle angle (HKA) for knee alignment studies in osteoarthritis? Analysis of long limb radiographs from the multicenter osteoarthritis (MOST) study. Osteoarthritis Cartilage. 2011;19(1):58–64. doi: 10.1016/j.joca.2010.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rosner B. Fundamentals of biostatistics. 6th ed. New York, USA: Thomson; 2006. [Google Scholar]
- 29.Gudbergsen H, Boesen M, Lohmander LS, Christensen R, Henriksen M, Bartels EM, et al. Weight loss is effective for symptomatic relief in obese subjects with knee osteoarthritis independently of joint damage severity assessed by high-field MRI and radiography. Osteoarthritis Cartilage. 2012;20(6):495–502. doi: 10.1016/j.joca.2012.02.639. [DOI] [PubMed] [Google Scholar]
- 30.Osteoarthritis. American Academy of Orthopedic Surgeons. Available at:URL: http://orthoinfo.aaos.org/topic.cfm?topic=a0.0227.2014 .
- 31.Nourbakhsh M, Motififard M, Shemshaki H, Etemadifar M, Zarezade A, Farajzadegan Z, et al. Efficacy of tibial proximal osteotomy in correction of lower limb alignment indexes in patients with osteoarthritis in medial compartment of knee. Med Arh. 2012;66(1):58–60. doi: 10.5455/medarh.2012.66.58-60. [DOI] [PubMed] [Google Scholar]
- 32.Levangie PK, Norkin CC. Joint Structure and Function. 5th ed. New York: Davis Company; 2011. [Google Scholar]


