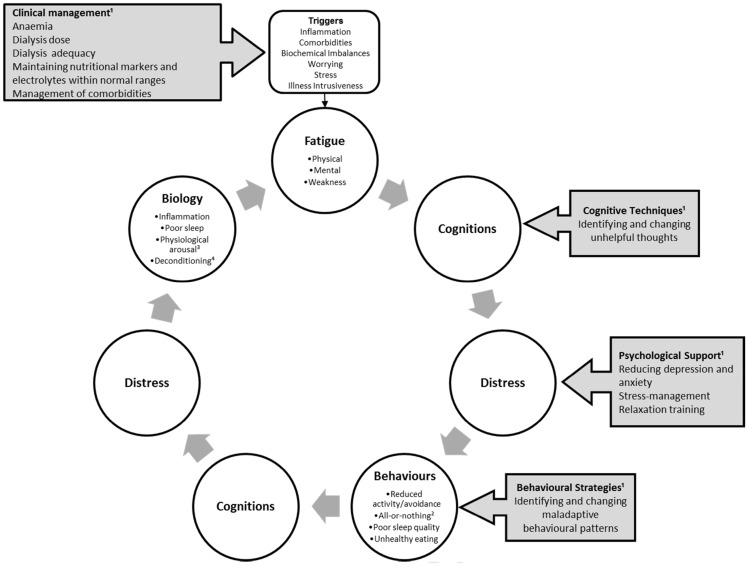
Fig. 1.
Preliminary biopsychosocial model of fatigue in end-stage kidney disease. This figure illustrates how fatigue can be triggered by illness, biochemical imbalances, or stress and worrying, and it can then be perpetuated and maintained by a vicious cycle of negative beliefs, depression and/or anxiety and maladaptive behavioural patterns. 1Grey boxes with arrows exemplify potential areas for intervention. Clinical management revolves around illness control and maintaining biochemical values within optimal ranges, as well as management of comorbidities. Cognitive techniques can be used to identify and change negative beliefs (e.g. catastrophizing) and to reduce depression and anxiety. Behavioural strategies, as part of psychotherapy, or physiotherapy can support patients in developing a stable activity pattern, and healthy sleep and dietary habits. 2All-or-nothing = behaviour characterized by bursts of activity followed by rest. ³Physiological arousal = in response to stress, chronic activation of the central and autonomic nervous systems as well as the endocrine system. 4Deconditioning = changes in body systems due to physical inactivity and disuses, such as loss in muscle strength and tone.