eFigure.
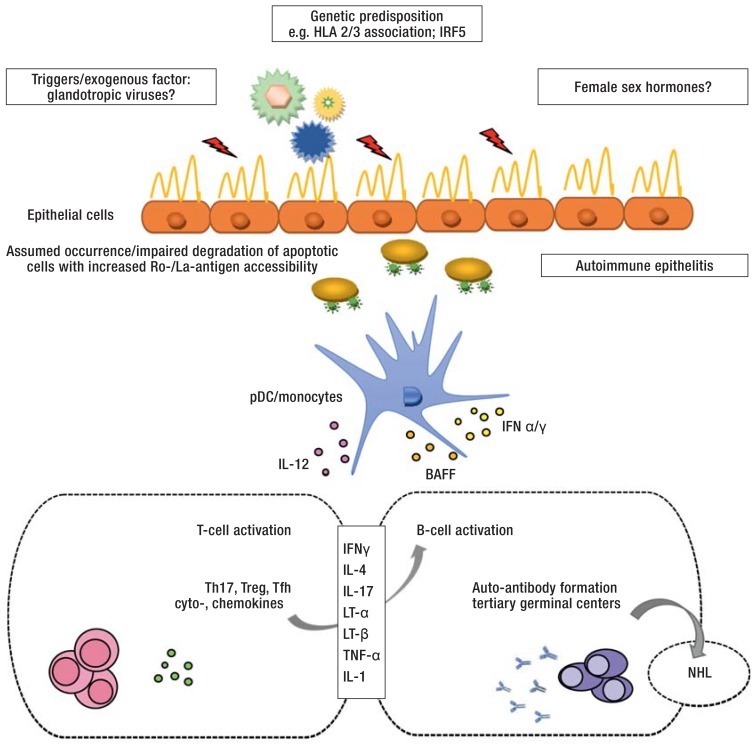
Diagram of the pathogenesis of Sjögren’s syndrome (modified according to [e6])
Genetic predisposition (e2, e3), exogenous triggering factors (e.g. glandotropic viruses) and hormonal changes are thought to initiate and maintain the immunopathogenesis of the disease. Glandular epithelial cells supposedly play a central pathophysiological role in the development of auto-immune epithelitis, especially with regard to antigen presentation of Ro/SSA- and La/SSB-protein complexes which are found on the surface of apoptotic cells (19). Both the innate (e.g. pDC/monocytes) and the adaptive immune system (T-/B-cells) are involved in the initiation of the disease and perpetuation of the immune response (e5, e6). Via the activation of various CD4+ T-helper cell subsets, B cells play an important role in auto-antibody production, from the formation of ectopic germinal center-like structures to the malignant transformation to NHL (11).
BAFF, B cell-activating factor of the tumor necrosis factor family; HLA, human leukocyte antigen; IFN ɑ/ɣ, interferon ɑ/ɣ; IL-1, -4, -12, -17, interleukin 1, 4, 12, 17; IRF5, interferon regulatory factor 5; LT-ɑ, lymphotoxin ɑ; LT-ß, lymphotoxin ß; NHL, Non-Hodgkin lymphoma; pDC, plasmacytoid dendritic cells; Tfh, follicular T cells; Th17, T helper cells 17; TNF-ɑ, tumor necrosis factor ɑ; Treg, regulatory T cells