Abstract
Desire for hastened death (DHD) represents a wish to die sooner than might occur by natural disease progression. Efficient and accurate assessment of DHD is vital for clinicians providing care to terminally ill patients. The Schedule of Attitudes Toward Hastened Death (SAHD) is a commonly used self-report measure of DHD. The goal of this study was to use methods grounded in item response theory (IRT) to analyze the psychometric properties of the SAHD and identify an abbreviated version of the scale. Data were drawn from 4 studies of psychological distress at the end of life. Participants were 1,076 patients diagnosed with either advanced cancer or AIDS. The sample was divided into 2 subsamples for scale analysis and development of the shortened form. IRT was used to estimate item parameters. A 6-item version of the SAHD (SAHD–A) was identified through examination of item parameter estimations. The SAHD–A demonstrated adequate convergent validity. Receiver operating characteristic analyses indicated comparable cut scores to identify patients with high levels of DHD. These analyses support the utility of the SAHD–A, which can be more easily integrated into research studies and clinical assessments of DHD.
Keywords: desire for death, palliative care, suicide, item response theory, scale evaluation
Over the past 20 years, researchers have been increasingly focused on understanding why a small but substantial number of terminally ill patients seek to hasten their own deaths. This desire may manifest in several different ways, including the expression of suicidal ideation, actual suicide attempts, requests for physician-assisted suicide, and refusal of life-prolonging interventions. Researchers have labeled these phenomena desire for hastened death (DHD; Chochinov et al., 1995). The construct of DHD represents a wish to die sooner than might occur by natural disease progression and can range from a passive or fleeting desire for death to occur quickly to specific thoughts regarding ending one’s life to formulating or enacting a plan for actively hastening death (Hudson et al., 2006; Mishara, 1999). Understanding the prevalence, correlates, and assessment of DHD is integral to helping clinicians respond to patient expressions of DHD by identifying optimal treatment approaches and clinical interventions.
Prevalence of DHD in terminally ill cancer patients ranges from 44.5% of patients reporting a fleeting desire for death (Chochinov et al., 1995) to 17% reporting a more persistent wish to die (Breitbart et al., 2000) to 12% openly discussing a wish for euthanasia with their physicians (Emanuel, Fairclough, Daniels, & Clarridge, 1996). Studies have consistently demonstrated significant positive correlations between DHD and depression, hopelessness, low spiritual well-being, low social support, cognitive impairment, and poor physical functioning (Breitbart et al., 2000; Hudson et al., 2006; O’Mahony et al., 2005; Pessin, Rosenfeld, Burton, & Breitbart, 2003; Rodin et al., 2007; Rosenfeld et al., 2006; Tiernan et al., 2002).
The Schedule of Attitudes Toward Hastened Death (SAHD; Rosenfeld et al., 1999, 2000) is a 20-item self-report measure that uses a true–false format to assess anticipated physical and emotional suffering and direct thoughts about facilitating one’s death. Initial validation studies found the SAHD to be a reliable and valid index of DHD (Rosenfeld et al., 1999, 2000). Given the importance of reducing patient burden in palliative care research, administration of a 20-item self-report scale is often challenging. Indeed, Pessin and colleagues (2008) found that while palliative care patients generally found participating in psychosocial research to be beneficial, those who found research participation burdensome often cited the length of questionnaires as a primary concern. Longer scales also increase the likelihood of nonresponse, resulting in missing data (Stanton, Sinar, Balzer, & Smith, 2002). Anecdotally, in our own research, we have noted that patients occasionally describe the SAHD as repetitive and potentially upsetting. There is a clear need for concise, focused measurement instruments, particularly in palliative care settings.
Item response theory (IRT) has been used increasingly often in health outcome research for the purpose of instrument development and evaluation (Cella et al., 2007). It can also be used to reduce the length of scales by identifying items most closely related to the trait of interest, resulting in reduced patient burden (Edelen & Reeve, 2007) and increasing the utility of self-report scales in both research and clinical settings. The purpose of this study was to analyze the SAHD using IRT to determine if an abbreviated form of the scale could be developed without sacrificing the scale’s utility. An abbreviated scale would reduce patient burden and could be more easily integrated into clinical applications (e.g., screening for psychological distress).
Method
Data for this study were drawn from four studies of psychological distress in patients with a terminal illness (Breitbart, Rosenfeld, Gibson, Pessin, et al., 2010; Olden, Rosenfeld, Pessin, & Breitbart, 2009; Rosenfeld et al., 2006, 2011). The SAHD was administered as a part of each study. Eligibility criteria included being English speaking and having a diagnosis of advanced cancer or AIDS. The total sample consisted of 1,076 participants. Average participant age was 58.1 (SD = 32.5). The majority of the sample was male (65.9%, n = 709). About half of participants were White (53.3%, n = 573), 32.1% (n = 345) were Black, 10.6% (n = 114) were Hispanic, and 2.8% (n = 30) were Asian or Pacific Islander; the remaining participants identified as Other (1.3%, n = 14).
Participants from the four studies were collapsed into three subsamples: patients with AIDS receiving inpatient care (n = 374, 34.8%), patients with cancer receiving inpatient palliative care (n = 509, 47.3%), and patients with cancer receiving outpatient care (n = 193, 17.9%). Differences between these three groups were expected given the differences in life expectancy and disease severity and past research demonstrating differences in rates of DHD among different medically ill populations and by proximity to death (e.g., Breitbart et al., 2000; Lichtenthal et al., 2009; Rosenfeld et al., 1999, 2000, 2006). There were considerable differences in illness severity between the subsamples, as the participants receiving inpatient palliative care had a life expectancy of approximately 6 weeks, whereas AIDS and cancer patients receiving outpatient care had a life expectancy of 6 to 12 months.
All participants completed the SAHD. Items expressing low levels of DHD were reverse scored so that for all items, higher scores indicated higher levels of DHD. Participants also completed measures of depression (the Hamilton Depression Rating Scale [HDRS], Hamilton, 1960), hopelessness (the Beck Hopelessness Scale [BHS], Beck, Weissman, Lester, & Trexler, 1974), and social support (the Duke–UNC Functional Social Support Questionnaire [DUFSS], Broadhead, Gehlbach, de Gruy, & Kaplan, 1988). Responses to Item 3 of the HDRS were used as a measure of suicidal ideation, and a single question assessing overall quality of life drawn from the McGill Quality of Life Questionnaire (Cohen, Mount, Strobel, & Bui, 1995) was administered. A subset of participants also completed the Desire for Death Rating Scale (DDRS; Chochinov et al., 1995).
Analyses were conducted using IBM SPSS 21 and R 3.1.0 (http://www.R-project.org/) with the ltm (Rizopoulos, 2006), OptimalCutpoints, (Lopez-Raton, Rodriguez-Alvarez, Cadarso-Suarez, & Gude-Sampedro, 2014), and lavaan (Rosseel, 2012) packages. The total sample was randomly divided into a development sample (n = 538) and a validation sample (n = 538). Dimensionality was evaluated using exploratory factor analysis (EFA) and confirmatory factor analysis (CFA). The EFA used a principal component factoring solution with varimax rotation. Acceptable model fit for the CFA was based on criteria outlined by Brown (2003) and included the root mean square error of approximation (RMSEA; <0.08; 90% confidence interval [CI] < 0.08), the comparative fit index (CFI; >0.90), and the Tucker-Lewis index (TLI; >0.90). A two-parameter logistic (2PL) model was used to estimate item parameters. This resulted in a model that estimated one intercept and one discrimination parameter for each item. As there are no established criteria for using IRT to guide scale reduction, an effort was made to select items that maintained adequate content coverage with maximum precision, as measured by item information, a concept that serves a similar function to reliability (Edelen & Reeve, 2007). Preliminary validation was conducted through examination of correlation coefficients between the short form of the SAHD and measures of psychological distress. Equivalent cut scores between the SAHD-A and the original SAHD were established through receiver operating characteristic (ROC) analyses. For the IRT analysis, individual missing items were addressed using maximum likelihood estimation that allows—and accounts for—missing data. Because the data set combined several studies, not all participants completed the same measures. Pairwise deletion was used to address missing data for the preliminary validation of the abbreviated version of the SAHD.
Results
The SAHD total scores for the development sample indicate that the majority of participants reported a low level of DHD (M = 3.64, SD = 4.08). However, consistent with the extant literature, a small number of participants reported a moderate (8–10; n = 30, 7.7%) or high (>10) level of DHD (n = 30, 7.7%). Mean score on the SAHD did not significantly differ between the three groups of patients included in the sample, F(2, 389) = 2.93, p = .06. Conditioning on the total SAHD score, nonparametric differential item functioning analysis revealed little difference at item level across three groups (complete results available upon request). This supports the decision to combine the three groups for further analysis.
A scree plot of the EFA revealed one dominant factor (the first five eigenvalues are 6.67, 1.69, 1.31, 1.03, and .968). This ratio of first to second eigenvalue of greater than 3 supports the use of a unidimensional solution (Lord, 1980). A CFA with robust weighted least squares estimation was used to evaluate the unidimensional model in the validation sample. This analysis revealed acceptable model fit (RMSEA = 0.06; 90% CI [0.05, 0.07]; CFI = 0.96; TLI = 0.95). A 2PL IRT model was fit to the data. Item parameter estimates are displayed in Table 1. Item parameters indicated considerable variation in item discrimination (0.60–3.98). The intercept parameters ranged from 0.38 to 2.72.
Table 1.
Item Parameters
| Item | a | d |
|---|---|---|
| 1 | 1.03 | 2.09 |
| 2 | .80 | .89 |
| 3 | 2.71 | 1.40 |
| 4 | 2.06 | 2.26 |
| 5 | 1.82 | 2.03 |
| 6 | 3.13 | .92 |
| 7 | 1.80 | 1.93 |
| 8 | 1.36 | 2.19 |
| 9 | 1.76 | .39 |
| 10 | 3.79 | 1.15 |
| 11 | 1.98 | 1.91 |
| 12 | 2.43 | 1.42 |
| 13 | 3.98 | .95 |
| 14 | 3.24 | 1.01 |
| 15 | .60 | 2.72 |
| 16 | 3.03 | .64 |
| 17 | .67 | .38 |
| 18 | .96 | 2.58 |
| 19 | 1.56 | 1.10 |
| 20 | 1.73 | 1.72 |
Note. a = discrimination parameter; d = intercept parameter.
In order to identify a short form of the SAHD, we first examined the item information curve of each item on each dimension to identify those items that provided the most information about the underlying latent construct (DHD). The height of the item information curves guided item selection; however, the location and spread were also considered. The items were examined for face validity to ensure that they represented salient aspects of DHD. The selected items were reviewed by the original authors of the SAHD to confirm face validity. Ultimately, six items (3, 4, 10, 13, 14, and 16; see Figure 1) were selected that maximized these criteria.
Figure 1.
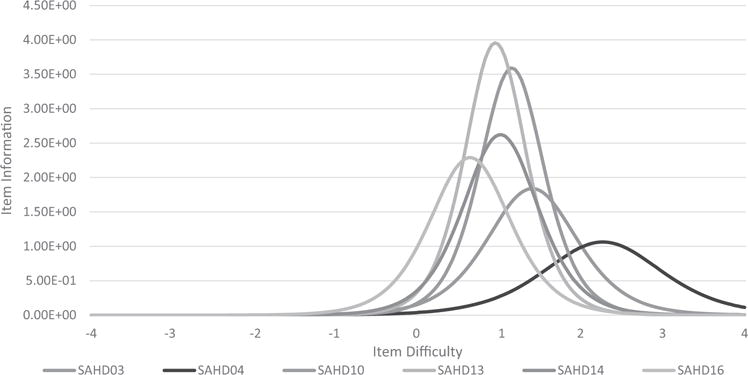
Item information curves for Schedule of Attitudes Toward Hastened Death, abbreviated version (SAHD–A) items.
The validity of the SAHD–A was examined through comparison to the original scale in the validation sample. Trait-level scores (0) were estimated for each participant for both the original SAHD and the SAHD–A using the multidimensional 2PL model. Estimated θ values for the two forms were strongly correlated (r = .88), providing initial evidence of validity. Examination of the test information functions of the SAHD and SAHD–A (see Figure 2) demonstrated that although the abbreviated form understandably provides less overall information, it actually provides comparable information about individuals with moderate to high levels of DHD.
Figure 2.
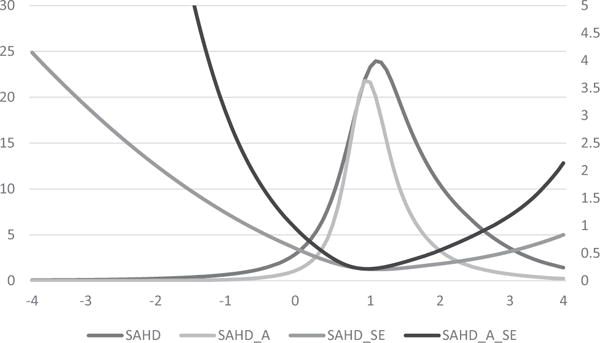
Test information and standard error (SE) for Schedule of Attitudes Toward Hastened Death (SAHD) and Schedule of Attitudes Toward Hastened Death, abbreviated version (SAHD–A). Test information is scaled on the y axis. Standard error is scaled on the z axis.
Pearson product–moment correlation coefficients were used to examine the relationship between performance on measures of psychological distress and well-being and the SAHD–A (see Table 2). As expected, SAHD–A total scores were significantly positively correlated with measures of depression, hopelessness, and suicidal ideation. Significant negative correlations were found between the SAHD–A and quality of life, lending support for the convergent validity of the abbreviated scale. Most of these correlations were only slightly smaller than those that were observed for the full version of the SAHD. Total scores on the two versions of the SAHD were strongly correlated with one another, r = .89, p < .001, and had comparable reliability (SAHD: Cronbach’s α = .84, SAHD–A: Cronbach’s α = .83).
Table 2.
Convergent Validity of SAHD–A and SAHD
| Construct | Measure | n | SAHD total r | SAHD–A r |
|---|---|---|---|---|
| Depression | HDRS | 307 | .49* | .32* |
| Hopelessness | BHS | 307 | .71* | .61* |
| Suicidal ideation | HDRS, Item 3 | 307 | .66* | .61* |
| Quality of life | MQOL | 305 | −.34* | −.25* |
| Social support | DUFSS | 294 | −.12* | .02 |
| Desire for hastened death | DDRS | 307 | .75* | .74* |
Note. SAHD-A = Schedule of Attitudes Toward Hastened Death, abbreviated version; SAHD = Schedule of Attitudes Toward Hastened Death; HDRS = Hamilton Depression Rating Scale; BHS = Beck Hopelessness Scale; MQOL = McGill Quality of Life Questionnaire; DUFSS = Duke–UNC Functional Social Support Questionnaire; DDRS = Desire for Death Rating Scale.
p < .01.
Past research has used scores of 7 and 10 as cut scores for identifying individuals with high levels of DHD (Rosenfeld et al., 2000). The 20-item version of the SAHD was treated as the standard for classifying high versus low levels of DHD. ROC analyses using Youden’s (1950) criteria were employed to identify comparable cut scores for the SAHD-A by maximizing the sum of sensitivity and specificity. A cut score of 3 on the SAHD–A was found to be equivalent to both a score of 7 or greater on the SAHD and a score of 10 or greater on the SAHD. This cut score yielded high levels of sensitivity (.91 and .97) and specificity (.91 and .91), respectively, for the 7- and 10-item cut scores for the original version.
Discussion
Accurately and efficiently measuring psychological distress is imperative for conducting ethical, meaningful, and clinically useful psychosocial research with patients approaching the end of life. A critical step toward improving the feasibility of this research is creating instruments that are as efficient as possible while still maintaining adequate precision. Advances in data analysis methods, such as IRT, allow for a more sophisticated evaluation of commonly used measures. This study applied IRT to the SAHD in order to determine whether an abbreviated version might be developed that still retains adequate psychometric properties.
Unlike the initial validation studies of the SAHD that relied on relatively small samples, this study benefited from the use of a large and diverse sample of patients with advanced illness. IRT analyses provided detailed item-level information that helped select the items that best discriminated patients with high versus low DHD and provided the most information about individuals across the continuum of DHD. This process resulted in a six-item version of the scale. The SAHD–A was strongly correlated with the original 20-item scale and provided comparable overall information. Analysis of the SAHD–A using the validation sample provided support for the convergent validity of the abbreviated version. Although the correlations were somewhat stronger with the original 20-item scale, the decrement in these associations was not surprising given the restricted range inherent in an abbreviated scale. Importantly, the SAHD–A was similar to the SAHD in its relationship to suicidal ideation, and equivalent cut scores generated strong classification accuracy in identifying patients with moderate and high levels of DHD.
The development of the SAHD–A has advantages for clinical and research settings. It can be more easily incorporated into research, as it will reduce the time needed to complete the measure without a marked decrease in the information obtained. This will minimize patient burden while allowing researchers to develop more parsimonious assessment batteries. In addition, the SAHD–A may be more easily integrated into clinical practice (i.e., in treatment settings). Elevated scores could be considered a red flag for a patient who may benefit from mental health assessment. Recent research has demonstrated that treatment for depression may result in a decrease in DHD (Breitbart, Rosenfeld, Gibson, Kramer, et al., 2010) and hence may warrant such referrals.
There are, of course, study limitations, including the lack of well-established guidelines for selecting items using IRT. Item selection for the SAHD–A was based on an examination of slope and intercept parameters and corresponding item information curves, but no a priori thresholds exist for differentiating acceptable versus unacceptable item parameters. Efforts were also made to maintain face validity of the included items, and the selected items were approved by the original authors of the SAHD. Although it is possible that other combinations of items could provide as much information as the six items we selected, these six items appeared to maximize both the scale’s psychometric and theoretical properties. Total scores on the SAHD–A are equally useful as total SAHD scores in identifying individuals with high DHD.
The assessment of DHD represents a critical issue for palliative care research. Identifying patients who may be inclined to terminate treatment prematurely or may even be in need of more aggressive mental health interventions is obviously important. The development of a brief scale that can facilitate this process while simultaneously minimizing patient burden represents a crucial step forward in this process. Hopefully, the availability of the SAHD–A will help improve the quality of care and quality of life for patients with advanced and life-limiting illnesses.
Acknowledgments
This research was supported in part by Grant NCI F31CA165635 from the National Cancer Institute to Elissa Kolva with Barry Rosenfeld as the grant sponsor.
Contributor Information
Elissa Kolva, Department of Medicine, University of Colorado, Denver.
Barry Rosenfeld, Department of Psychology, Fordham University.
Ying Liu, Department of Psychology, Fordham University.
Hayley Pessin, Memorial Sloan Kettering Cancer Center, Department of Psychiatry & Behavioral Sciences, New York, New York.
William Breitbart, Memorial Sloan Kettering Cancer Center, Department of Psychiatry & Behavioral Sciences, New York, New York.
References
- Beck AT, Weissman A, Lester D, Trexler L. The measurement of pessimism: The Hopelessness Scale. Journal of Consulting and Clinical Psychology. 1974;42:861–865. doi: 10.1037/h0037562. http://dx.doi.org/10.1037/h0037562. [DOI] [PubMed] [Google Scholar]
- Breitbart W, Rosenfeld B, Gibson C, Kramer M, Li Y, Tomarken A, Schuster M. Impact of treatment for depression on desire for hastened death in patients with advanced AIDS. Psychosomatics. 2010;51:98–105. doi: 10.1176/appi.psy.51.2.98. http://dx.doi.org/10.1176/appi.psy.51.2.98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breitbart W, Rosenfeld B, Gibson C, Pessin H, Poppito S, Nelson C, Olden M. Meaning-centered group psychotherapy for patients with advanced cancer: A pilot randomized controlled trial. Psycho-Oncology. 2010;19:21–28. doi: 10.1002/pon.1556. http://dx.doi.org/10.1002/pon.1556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breitbart W, Rosenfeld B, Pessin H, Kaim M, Funesti-Esch J, Galietta M, Brescia R. Depression, hopelessness, and desire for hastened death in terminally ill patients with cancer. JAMA: Journal of the American Medical Association. 2000;284:2907–2911. doi: 10.1001/jama.284.22.2907. http://dx.doi.org/10.1001/jama.284.22.2907. [DOI] [PubMed] [Google Scholar]
- Broadhead WE, Gehlbach SH, de Gruy FV, Kaplan BH. The Duke-UNC Functional Social Support Questionnaire: Measurement of social support in family medicine patients. Medical Care. 1988;26:709–723. doi: 10.1097/00005650-198807000-00006. http://dx.doi.org/10.1097/00005650-198807000-00006. [DOI] [PubMed] [Google Scholar]
- Brown TA. Confirmatory factor analysis of the Penn State Worry Questionnaire: Multiple factors or method effects? Behaviour Research and Therapy. 2003;41:1411–1426. doi: 10.1016/s0005-7967(03)00059-7. http://dx.doi.org/10.1016/S0005-7967(03)00059-7. [DOI] [PubMed] [Google Scholar]
- Cella D, Yount S, Rothrock N, Gershon R, Cook K, Reeve B, Rose M. The Patient-Reported Outcomes Measurement Information System (PROMIS): Progress of an NIH Roadmap cooperative group during its first two years. Medical Care. 2007;45(Suppl. 1):S3–S11. doi: 10.1097/01.mlr.0000258615.42478.55. http://dx.doi.org/10.1097/01.mlr.0000258615.42478.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chochinov HM, Wilson KG, Enns M, Mowchun N, Lander S, Levitt M, Clinch JJ. Desire for death in the terminally ill. The American Journal of Psychiatry. 1995;152:1185–1191. doi: 10.1176/ajp.152.8.1185. http://dx.doi.org/10.1176/ajp.152.8.1185. [DOI] [PubMed] [Google Scholar]
- Cohen SR, Mount BM, Strobel MG, Bui F. The McGill Quality of Life Questionnaire: A measure of quality of life appropriate for people with advanced disease. A preliminary study of validity and acceptability. Palliative Medicine. 1995;9:207–219. doi: 10.1177/026921639500900306. http://dx.doi.org/10.1177/026921639500900306. [DOI] [PubMed] [Google Scholar]
- Edelen MO, Reeve BB. Applying item response theory (IRT) modeling to questionnaire development, evaluation, and refinement. Quality of Life Research: An International Journal of Quality of Life Aspects of Treatment, Care and Rehabilitation. 2007;16(Suppl. 1):5–18. doi: 10.1007/s11136-007-9198-0. http://dx.doi.org/10.1007/s11136-007-9198-0. [DOI] [PubMed] [Google Scholar]
- Emanuel EJ, Fairclough DL, Daniels ER, Clarridge BR. Euthanasia and physician-assisted suicide: Attitudes and experiences of oncology patients, oncologists, and the public. The Lancet. 1996;347:1805–1810. doi: 10.1016/s0140-6736(96)91621-9. http://dx.doi.org/10.1016/S0140-6736(96)91621-9. [DOI] [PubMed] [Google Scholar]
- Hamilton M. A rating scale for depression. Journal of Neurology, Neurosurgery & Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. http://dx.doi.org/10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hudson PL, Kristjanson LJ, Ashby M, Kelly B, Schofield P, Hudson R, Street A. Desire for hastened death in patients with advanced disease and the evidence base of clinical guidelines: A systematic review. Palliative Medicine. 2006;20:693–701. doi: 10.1177/0269216306071799. http://dx.doi.org/10.1177/0269216306071799. [DOI] [PubMed] [Google Scholar]
- Lichtenthal WG, Nilsson M, Zhang B, Trice ED, Kissane DW, Breitbart W, Prigerson HG. Do rates of mental disorders and existential distress among advanced stage cancer patients increase as death approaches? Psycho-Oncology. 2009;18:50–61. doi: 10.1002/pon.1371. http://dx.doi.org/10.1002/pon.1371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lopez-Raton M, Rodriguez-Alvarez MX, Cadarso-Suarez C, Gude-Sampedro F. OptimalCutpoints: An R package for selecting optimal cutpoints in diagnostic tests. Journal of Statistical Software. 2014;61:1–36. http://dx.doi.org/10.18637/jss.v061.i08. [Google Scholar]
- Lord FM. Applications of item response theory to practical testing problems. New York, NY: Erlbaum; 1980. [Google Scholar]
- Mishara BL. Synthesis of research and evidence on factors affecting the desire of terminally ill or seriously chronically ill persons to hasten death. Omega: Journal of Death and Dying. 1999;39:1–70. doi: 10.2190/5YED-YKMY-V60G-L5U5. http://dx.doi.org/10.2190/5YED-YKMY-V60G-L5U5. [DOI] [PubMed] [Google Scholar]
- Olden M, Rosenfeld B, Pessin H, Breitbart W. Measuring depression at the end of life: Is the Hamilton Depression Rating Scale a valid instrument? Assessment. 2009;16:43–54. doi: 10.1177/1073191108320415. http://dx.doi.org/10.1177/1073191108320415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Mahony S, Goulet J, Kornblith A, Abbatiello G, Clarke B, Kless-Siegel S, Payne R. Desire for hastened death, cancer pain and depression: Report of a longitudinal observational study. Journal of Pain and Symptom Management. 2005;29:446–457. doi: 10.1016/j.jpainsymman.2004.08.010. http://dx.doi.org/10.1016/j.jpainsymman.2004.08.010. [DOI] [PubMed] [Google Scholar]
- Pessin H, Galietta M, Nelson CJ, Brescia R, Rosenfeld B, Breitbart W. Burden and benefit of psychosocial research at the end of life. Journal of Palliative Medicine. 2008;11:627–632. doi: 10.1089/jpm.2007.9923. http://dx.doi.org/10.1089/jpm.2007.9923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pessin H, Rosenfeld B, Burton L, Breitbart W. The role of cognitive impairment in desire for hastened death: A study of patients with advanced AIDS. General Hospital Psychiatry. 2003;25:194–199. doi: 10.1016/s0163-8343(03)00008-2. http://dx.doi.org/10.1016/S0163-8343(03)00008-2. [DOI] [PubMed] [Google Scholar]
- Rizopoulos D. ltm: An R package for latent variable modeling and item response analysis. Journal of Statistical Software. 2006;17:1–25. http://dx.doi.org/10.18637/jss.v017.i05. [Google Scholar]
- Rodin G, Zimmermann C, Rydall A, Jones J, Shepherd FA, Moore M, Gagliese L. The desire for hastened death in patients with metastatic cancer. Journal of Pain and Symptom Management. 2007;33:661–675. doi: 10.1016/j.jpainsymman.2006.09.034. http://dx.doi.org/10.1016/j.jpainsymman.2006.09.034. [DOI] [PubMed] [Google Scholar]
- Rosenfeld B, Breitbart W, Galietta M, Kaim M, Funesti-Esch J, Pessin H, Brescia R. The schedule of attitudes toward hastened death: Measuring desire for death in terminally ill cancer patients. Cancer. 2000;88:2868–2875. doi: 10.1002/1097-0142(20000615)88:12<2868::aid-cncr30>3.0.co;2-k. http://dx.doi.org/10.1002/1097-0142(20000615)88:12<2868::aid-cncr30>3.0.co;2-k. [DOI] [PubMed] [Google Scholar]
- Rosenfeld B, Breitbart W, Gibson C, Kramer M, Tomarken A, Nelson C, Schuster M. Desire for hastened death among patients with advanced AIDS. Psychosomatics: Journal of Consultation and Liaison Psychiatry. 2006;47:504–512. doi: 10.1176/appi.psy.47.6.504. http://dx.doi.org/10.1176/appi.psy.47.6.504. [DOI] [PubMed] [Google Scholar]
- Rosenfeld B, Breitbart W, Stein K, Funesti-Esch J, Kaim M, Krivo S, Galietta M. Measuring desire for death among patients with HIV/AIDS: The Schedule of Attitudes Toward Hastened Death. The American Journal of Psychiatry. 1999;156:94–100. doi: 10.1176/ajp.156.1.94. http://dx.doi.org/10.1176/ajp.156.1.94. [DOI] [PubMed] [Google Scholar]
- Rosenfeld B, Pessin H, Lewis C, Abbey J, Olden M, Sachs E, Breitbart W. Assessing hopelessness in terminally ill cancer patients: Development of the Hopelessness Assessment in Illness Questionnaire. Psychological Assessment. 2011;23:325–336. doi: 10.1037/a0021767. http://dx.doi.org/10.1037/a0021767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosseel Y. Lavaan: An R package for structural equation modeling. Journal of Statistical Software. 2012;48:1–36. http://dx.doi.org/10.18637/jss.v048.i02. [Google Scholar]
- Stanton JM, Sinar EF, Balzer WK, Smith PC. Issues and strategies for reducing the length of self-report scales. Personnel Psychology. 2002;55:167–194. http://dx.doi.org/10.1111/j.1744-6570.2002.tb00108.x. [Google Scholar]
- Tiernan E, Casey P, O’Boyle C, Birkbeck G, Mangan M, O’Siorain L, Kearney M. Relations between desire for early death, depressive symptoms and antidepressant prescribing in terminally ill patients with cancer. Journal of the Royal Society of Medicine. 2002;95:386–390. doi: 10.1258/jrsm.95.8.386. http://dx.doi.org/10.1258/jrsm.95.8386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Youden WJ. Index for rating diagnostic tests. Cancer. 1950;3:32–35. doi: 10.1002/1097-0142(1950)3:1<32::aid-cncr2820030106>3.0.co;2-3. http://dx.doi.org/10.1002/1097-0142(1950)3:1<32::aid-cncr2820030106>3.0.co;2-3. [DOI] [PubMed] [Google Scholar]


