Abstract
Our understanding of polymicrobial gastrointestinal infections and their effects on host biology remains incompletely understood. Giardia duodenalis is an ubiquitous intestinal protozoan parasite infecting animals and humans. Concomitant infections with Giardia and other gastrointestinal pathogens commonly occur. In countries with poor sanitation, Giardia infection has been associated with decreased incidence of diarrheal disease and fever, and reduced serum inflammatory markers release, via mechanisms that remain obscure. This study analyzed Giardia spp. co-infections with attaching and effacing (A/E) pathogens, and assessed whether and how the presence of Giardia modulates host responses to A/E enteropathogens, and alters intestinal disease outcome. In mice infected with the A/E pathogen Citrobacter rodentium, co-infection with Giardia muris significantly attenuated weight loss, macro- and microscopic signs of colitis, bacterial colonization and translocation, while concurrently enhancing the production and secretion of antimicrobial peptides (AMPs) mouse β-defensin 3 and trefoil factor 3 (TFF3). Co-infection of human intestinal epithelial cells (Caco-2) monolayers with G. duodenalis trophozoites and enteropathogenic Escherichia coli (EPEC) enhanced the production of the AMPs human β-defensin 2 (HBD-2) and TFF3; this effect was inhibited with treatment of G. duodenalis with cysteine protease inhibitors. Collectively, these results suggest that Giardia infections are capable of reducing enteropathogen-induced colitis while increasing production of host AMPs. Additional studies also demonstrated that Giardia was able to directly inhibit the growth of pathogenic bacteria. These results reveal novel mechanisms whereby Giardia may protect against gastrointestinal disease induced by a co-infecting A/E enteropathogen. Our findings shed new light on how microbial-microbial interactions in the gut may protect a host during concomitant infections.
Introduction
Giardia duodenalis (syn. G. lamblia, G. intestinalis) is a ubiquitous intestinal protozoan parasite that infects a wide array of hosts, and is responsible for diarrheal disease as well as numerous post-infectious extraintestinal pathologies [1–5]. It is one of the most common fecal-oral parasitic infection of the human small intestine worldwide [1, 4, 5]. Due to the high burden of G. duodenalis-related illness on health and economics in the developing world, this protozoan parasite has been included in the World Health Organization’s (WHO) Neglected Diseases Initiative since 2006 [6, 7]. It is estimated that more than one billion people are at risk of infection from G. duodenalis each year [8]. Giardia infection can be an asymptomatic, or cause acute self-limiting diarrhea or chronic diarrhea, with or without dehydration, and with or without intestinal malabsorption [9–11]. Giardiasis is responsible for failure to thrive and cognitive malfunction in children from areas of the world where the infection is endemic [1, 12]. In spite of high parasite loads that can exceed 106 trophozoites per centimeter of gut during the acute stage of the infection, the intestinal mucosa of Giardia-infected hosts is devoid of overt signs of inflammation [4, 13–15].
Giardia infections are acquired via ingestion of infectious cysts in contaminated food or water sources, or directly via the fecal-oral route. These routes of infection are shared among a broad variety of gastrointestinal (GI) pathogens, and as a result, Giardia co-infections are common, especially in regions with poor water and food sanitation [16]. As discussed in a recent editorial, more research needs to characterize how concurrent infections may alter disease outcome, either directly or indirectly [17]. Using complex polymicrobial infection model systems that mimic true disease conditions will help uncover new, more realistic, therapeutic targets. Giardia infections have been reported concomitantly with bacterial, viral, and/or other parasitic enteropathogens [18–25]. Even though most of these pathogens are known to cause diarrheal disease, some reports suggest that Giardia may attenuate diarrheal illness severity [16, 26]. The mechanisms are unknown. Similarly, clinical research in those parts of the world has shown that children infected with G. duodenalis have a reduced likelihood of developing diarrheal disease and fever, and have reduced serum inflammatory scores compared to Giardia-negative children [27, 28]. In Bangladesh, Giardia infections have been associated with the development of diarrhea [29], yet, other studies in children from Bangladesh have suggested that the parasite neither increased nor decreased the odds of acute diarrhea [30]. Other reports indicate that Tanzanian children infected with Giardia were less likely to develop diarrheal disease when compared to children not infected with Giardia [27]. More research is required to elucidate how Giardia infections may result in diarrheal disease or remain asymptomatic.
Other reports have suggested that Giardia may be deleterious during co-infections with other GI pathogens [31, 32]. While many studies have investigated host immunity in giardiasis, it remains to be shown whether and how Giardia may have immunomodulatory effects that could modulate host susceptibility to GI co-infections [33].
The production of antimicrobial peptides (AMPs) by intestinal epithelial cells (IECs) plays a critical role in intestinal mucosal homeostasis and antimicrobial immunity against enteropathogens [34]. Salmonella spp., Shigella spp., Citrobacter rodentium, enteropathogenic Escherichia coli (EPEC) and enterohemorrhagic E. coli (EHEC) are able to induce the production of AMPs in humans or mice [35–37]. For example, in humans, human β-defensin-2 (HBD-2) is induced in IECs in vitro following exposure to pathogenic Salmonella spp. infection [38, 39] and in gastric epithelial cells, during human Helicobacter pylori infection [38]. HBD-2 has microbicidal activity against Gram positive and negative bacteria and yeast [40]. The murine homolog of HBD-2, mouse β-defensin 3 (mBD3), is broadly expressed within murine GI tissues, and has broad-spectrum antimicrobial activity [41, 42]. Trefoil factor 3 (TFF3) is a small cysteine-rich secretory peptide that is expressed by goblet cells throughout the gastrointestinal tract [43]. TFF3 promotes epithelial restitution following mucosal injury [44] and enhances the protective barrier properties of the mucus layer, which is important for protection against enteropathogens [45]. While not having a direct antibacterial effect, it protects the host against infection by binding to bacteria, and by synergizing with Muc2 [46–49]. The role of AMPs during Giardia infections remains incompletely understood. Previous experiments performed in vitro have demonstrated that G. duodenalis trophozoites are susceptible to intestinal epithelial AMPs [50], and intestinal epithelial cells exposed to Giardia parasites in vitro enhance production of matrix metalloprotease 7, mediators that are required for the activation of α-defensins [51]. Whether and how Giardia may affect AMP production in IECs to modulate disease during co-infections has yet to be assessed.
The Giardia genome contains 27 cathepsin B- and L-like cysteine proteases [52], and several of these proteases are released upon exposure to epithelial cells in vitro [53]. Our understanding of Giardia cathepsin cysteine proteases and their role during host-parasite interactions is ever expanding. Previous research has demonstrated that Giardia cathepsin cysteine proteases are implicated, at least in part, in trophozoite encystation and excystation [54], degradation of pro-inflammatory chemokines [26], and some of the pathophysiological changes observed in infected enterocytes [55]. The role of Giardia proteases in the modulation of AMPs and enteric disease modulation during co-infections is unknown.
Recent findings have established that Giardia infection may have detrimental effects at intestinal sites beyond its area of trophozoite colonization, including post-infectious hypersensitivity in the rectum [12] and goblet cells depletion in the colon [56]. The mechanisms remain unclear, but these observations provide a rationale for investigating the effects of Giardia during co-infections with enteropathogens in colonic cells and tissues.
Together, the data describe a new causal relationship between the presence of Giardia and the attenuation of intestinal disease caused by a co-infecting A/E entropathogen.
Results
G. muris infection attenuates C. rodentium-induced colitis
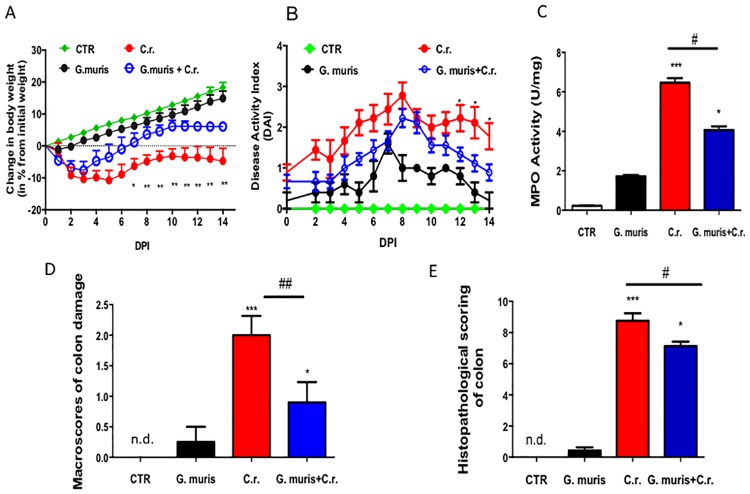
Our initial experiments sought to determine whether Giardia infections were protective during co-infection with the A/E pathogen C. rodentium. Therefore, 7 to 8 week old mice were co-infected with G. muris and C. rodentium for 14 days. The murine enteropathogen C. rodentium is commonly used a model for EPEC and EHEC infections [57, 58]. Similarly, G. muris is often used to model human G. duodenalis infections [59, 60]. Animals infected with C. rodentium lost weight from the first day of infection and did not return to baseline weight (Fig 1A), while animals co-infected with G. muris and C. rodentium lost weight at the beginning of infection but then dramatically recovered weight gain by day 7 compared to mice infected with C. rodentium alone (Fig 1A). Control animals and animals infected with G. muris gained weight similarly throughout the experimental time (Fig 1A). In co-infected animals, disease activity index (DAI) scores (fecal blood, fecal consistency, and histological evidence of erythema edema, colonic thickness) were higher than in control animals (Fig 1B), but significantly lower than in animals infected with C. rodentium alone (Fig 1B).
Fig 1. G. muris attenuates concomitant C. rodentium-induced colitis.
Male C57/BL6 mice (7–8 week old) were infected with either G. muris, or C. rodentium (C.r.), or both in co-infection (G. muris + C.r.). The figure illustrates (A) Changes in body weights and (B) disease activity index (DAI) assessed over 14 days. (C) On day 14 post-infection, colonic myeloperoxydase activity (MPO), (D) macroscopic damage of the colon and (E) histopathological damage scores on H&E stained tissue were assessed. All data are representative of n = 5–10/group and represented as mean±SEM. * p<0.05, ** p<0.01, *** p<0.001 –compared to control group (CTR); # p<0.05, ## p<0.01 versus the corresponding group, indicated by line; n.d. means not detected, that is equivalent to 0.
C. rodentium increased MPO activity in colonic tissue levels versus control values (Fig 1C). Co-infection with G. muris significantly attenuated this effect (Fig 1C). G. muris alone did not change colonic MPO activity (Fig 1C). Infection with C. rodentium alone also significantly increased colonic macro- and microscopic damage scores compared with uninfected control animals (Fig 1D and 1E, respectively). Co-infection with G. muris significantly attenuated this effect (Fig 1D and 1E). Damage scores from tissues of mice infected with G. muris alone were similar to controls (Fig 1D and 1E). Histopathology revealed that C. rodentium caused significant microscopic damage in the colon at 14 DPI (S1 Fig). Tissues from animals co-infected with G. muris showed only mild mucosal inflammatory infiltrates and edema (S1 Fig).
G. muris infection reduces fecal C. rodentium numbers
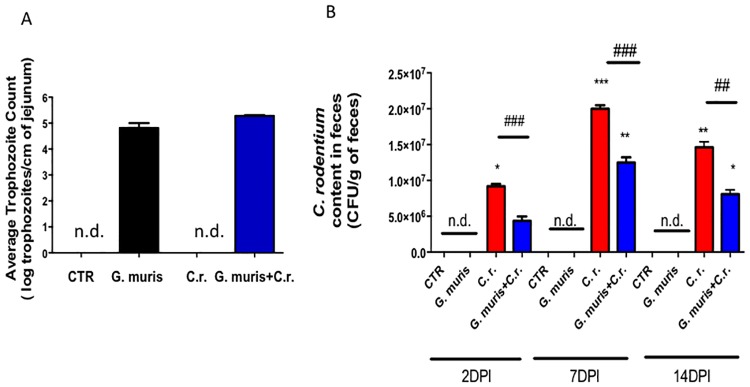
We next sought to determine whether the differences in the severity of colitis were associated with alterations of the gut microbial burden. On day 14 post-infection, trophozoites were enumerated in the jejunum of both groups infected with Giardia and values were not significantly different from each other (Fig 2A). In contrast, C. rodentium fecal CFUs were significantly lower in animals co-infected with G. muris than in those infected with C. rodentium alone (on days 2 and 7 post-infection) (Fig 2B).
Fig 2. Duodenal G. muris trophozoite counts, and fecal C. rodentium burden.
Male C57BL/6 mice aged 7 to 8 weeks were infected with G. muris and C. rodentium (C.r.) separately and in co-infection (G. muris + C.r.) (A) On day 14 post- infection, numbers of G. muris trophozoites were counted in the jejunum. (B) C. rodentium fecal burden was determined by plating colonic stool contents on Lysogeny broth (LB) agar plates. All data are representative of n = 5–10/group and represented as mean±SEM. * p<0.05, ** p<0.01, *** p<0.001– compared to control group (CTR); ### p<0.001 versus the corresponding group, indicated by line; n.d. means not detected, that is equivalent to 0.
Giardia prevents attachment and translocation of C. rodentium into host tissues
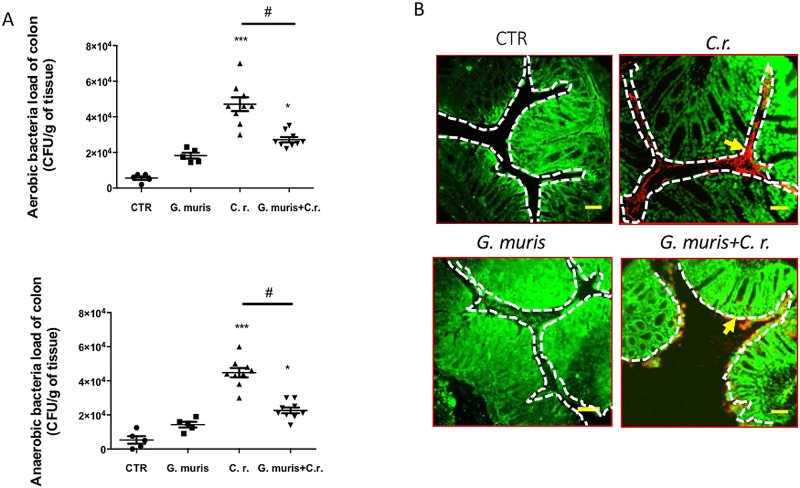
Follow-up analyses set out to determine whether G. muris co-infection prevented C. rodentium from disseminating into host tissues. Both aerobic and anaerobic bacterial loads of colonic homogenates were significantly reduced in the co-infected group compared to C. rodentium-infected mice (Fig 3A). In order to selectively visualize C. rodentium in the colon in situ, we used a green-fluorescent protein (GFP)-expressing C. rodentium, and immunostaining for C. rodentium lipopolysaccharide (LPS) [61]. In animals infected with C. rodentium alone, large numbers of bacteria were detected in the lumen, attached to the mucosa, and within colonic tissues. In mice co-infected with G. muris, C. rodentium was occasionally attached to the mucosa but was mostly localized in the lumen and not seen within tissues (Fig 3B and S2 Fig). Staining of C. rodentium LPS demonstrates bacterial attachment to the epithelial surface (Fig 3B), which was confirmed by staining of GFP-labelled C. rodentium (S2 Fig). This technique also revealed translocation of bacteria within the colonic tissue.
Fig 3. G. muris reduces C. rodentium colonization in the colon of co-infected mice, and decreases bacterial attachment to colonic mucosa.
Male C57BL/6 mice aged 7 to 8 weeks were infected with G. muris and C. rodentium (C.r.) separately and in co-infection (G. muris + C.r.) (A) On 14th day post-infection colon samples were collected and homogenized for aerobic and anaerobic colonic bacterial loads. (B) C. rodentium in the colon was stained using anti-lipopolysaccharide (LPS). The surface of the colonic mucosa is indicated by a white dashed line, and arrows indicate bacterial attachment to the colonic mucosa (Original magnification = 400x. Scale bar = 25 μm. Red—bacteria, Green—DAPI). All data are representative of n = 5–10/group and represented as mean±SEM. * p<0.05, ** p<0.01, *** p<0.001– compared to control group (CTR); # p<0.05 versus the corresponding group, indicated by line.
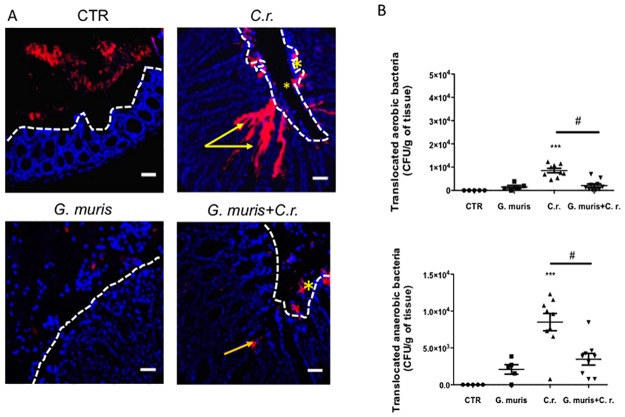
We next used fluorescent in situ hybridization (FISH) to visualize the translocation of commensal microbiota bacteria into tissues underlying the colonic epithelium. In uninfected mice, commensal microbes were kept at distance from the epithelium, and bacterial translocation into the lamina propria was not observed (Fig 4A). In animals infected with C. rodentium alone, commensal bacteria were observed deep in the bottom of intestinal crypts and within the mucus layer (Fig 4A). In mice co-infected with G. muris, the deeper invasion of microbiota was not observed (Fig 4A). Another set of experiments sought to determine whether G. muris was able to reduce C. rodentium-induced translocation of bacteria to distant organ sites. Infection with C. rodentium alone significantly elevated the numbers of aerobic and anaerobic bacteria translocated to both the spleen and liver (Fig 4B and S3 Fig). In mice co-infected with G. muris, aerobic and anaerobic bacterial counts in the spleen and liver were significantly reduced (Fig 4B and S3 Fig). Infection with G. muris alone induced a low degree of bacterial translocation (Fig 4B and S3 Fig).
Fig 4. G. muris reduces C. rodentium attachment to colonic tissues, and translocation to the spleen.
Male C57/Bl6 mice (7–8 week old) were infected with G. muris and C. rodentium (C.r.) separately and in co-infection. On day 14 post-infection colon samples and spleen were collected and analyzed. (A) Fluorescent in situ hybridization (FISH) staining was performed on the colonic samples. (Original magnification = 400x. Scale bar = 25 μm. Red—bacteria, Blue—DAPI). Stars identify bacteria attached to mucosa, and arrows indicate bacteria that have translocated into the lamina propria. (B) Translocation of aerobic and anaerobic bacteria to the spleen. All data are representative of n = 5–10/group and represented as mean±SEM. * p<0.05, ** p<0.01, *** p<0.001– compared to control group (CTR); # p<0.05 versus the corresponding group, indicated by line.
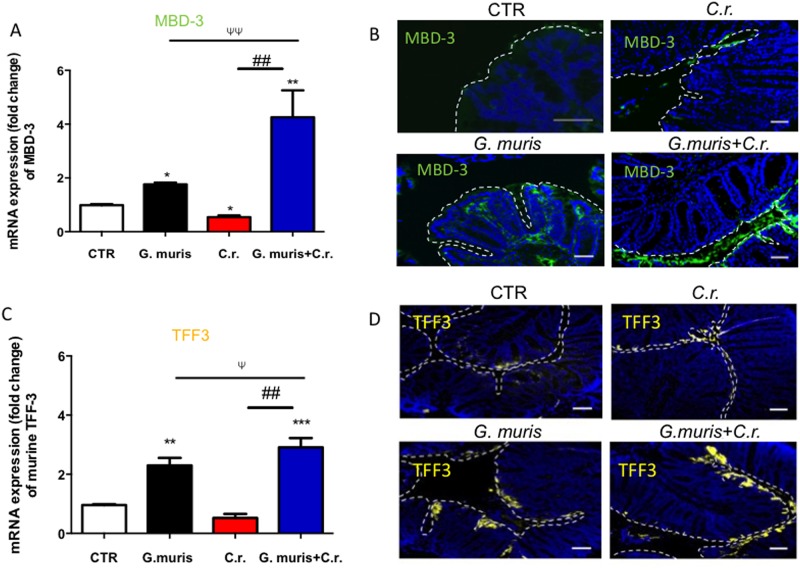
Giardia stimulates transcription and expression of β-defensin 3 (MBD-3) and Trefoil factor 3 (TFF3)
We next assessed whether Giardia infection may activate host AMPs. Analyses of colonic tissues revealed that MBD-3 and TFF3 mRNA was significantly higher in co-infected mice compared with those infected with C. rodentium alone (Fig 5A and 5C). AMP mRNAs were also significantly higher in mice infected with Giardia alone compared to uninfected controls (Fig 5A and 5C). We then visualized the protein expression of AMPs in colonic tissues using immunofluorescence. Giardia alone increased MBD-3 and TFF3 staining intensity in the colonic lamina propria (Fig 5B and 5D). In co-infected mice, high staining intensity of MDB-3 and TFF3 was observed on the apical surface of epithelium but also within the colonic lumen (Fig 5B and 5D). In contrast, mice infected with C. rodentium alone exhibited much lower levels of MBD-3 and TFF3, which were seen predominantly in the colonic lumen and mucosa (Fig 5B and 5D). In uninfected controls, very low levels of MBD-3 and TFF3 could be seen, mostly on the epithelial surface of colonic crypts (Fig 5B and 5D).
Fig 5. Animals co-infected with G. muris and C. rodentium have elevated colonic expression and secretion of MBD-3 and TFF-3.
Male C57/BL6 mice (7–8 week old) were infected with G. muris and C. rodentium (C.r.) separately and in co-infection. The figure illustrates results from analyses of the colon performed 14 days post-infection. (A and C) Colonic mRNA levels of mbd-3 and tff3 were assessed. (B and D) Immunofluorescence of MBD-3 (green) and TFF3 (yellow) was also performed. Original magnification = 400x. Scale bar = 25 μm. Colonic mucosa is indicated by a white dashed line. All data are representative of n = 5–10/group and represented as mean±SEM. * p<0.05, ** p<0.01, *** p<0.001– compared to control group (CTR); ## p<0.01 versus the corresponding group, indicated by line; Ψ p<0.05, ΨΨ p<0.01 versus the corresponding group, indicated by line.
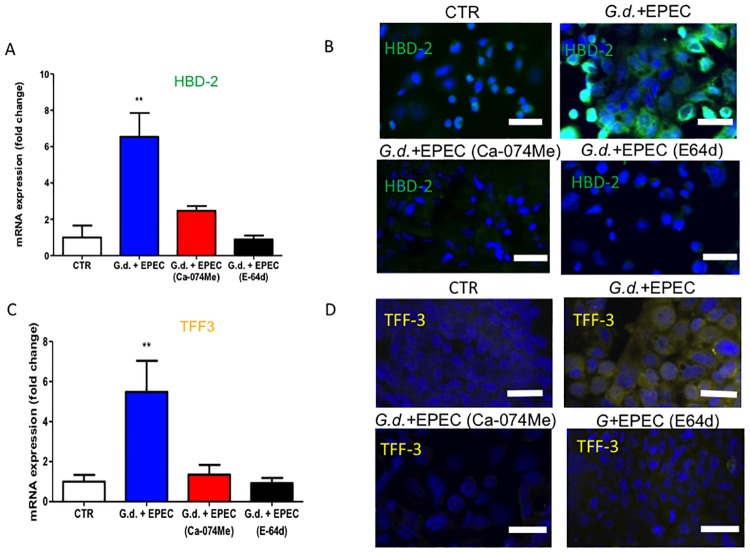
G. duodenalis co-infection with EPEC increases AMPs production in cysteine protease dependent manner in human intestinal epithelial cells
In order to test the present in vivo findings from mice in human cells, confluent human Caco-2 enterocytes were co-incubated with G. duodenalis trophozoites and EPEC, the human analogue of C. rodentium. With this model we set out to determine potential mechanisms via which Giardia may protect a host during co-infection. In addition, we investigated whether G. duodenalis cathepsin-like cysteine proteases were involved in inducing expression of AMPs within human IECs. The expression of HBD-2 and TFF3 mRNA was significantly increased in Caco-2 monolayers co-infected with EPEC and G. duodenalis compared with those infected with EPEC alone, with Giardia alone, or with uninfected controls (Fig 6A and 6C, S4A and S4C Fig). Immunostaining intensity of HBD-2 and TFF3 was higher on Caco-2 enterocytes co-infected with G. duodenalis and EPEC than cells infected with EPEC alone or uninfected cells, or cells exposed to Giardia alone (Fig 6B and 6D, S4B and S4D Fig). Inhibition of G. duodenalis cathepsin cysteine proteases with a cathepsin B selective inhibitor (Ca-074Me) as validated recently [26], or a broad spectrum cysteine protease inhibitor (E-64d) completely abolished the elevation of mRNA and immunostained protein for both AMPs observed in co-infected cells (Fig 6B and 6D).
Fig 6. Co-infection with G. duodenalis and EPEC activates the production of anti-microbial peptides (APMs) in Caco-2 cells in cathepsin B-like protease- dependent manner.
Caco-2 monolayers were co-incubated with G. duodenalis for 1 hour, pre-treated or not with a cathepsin B specific inhibitor, Ca-074Me, or a broad-spectrum cysteine protease inhibitor, E-64d, and then administered EPEC for 2 hours. (A and C) mRNA levels of HBD-2 and TFF3 were analyzed. Data is represented as fold change relative to the control group in mean ±SEM. (B and D) Immunofluorescence of Caco-2 monolayers for DAPI (blue) and HBD-2 (green) or TFF3 (yellow) was also performed. Original magnification = 400x Scale bar = 50 μm. All data are representative of n = 5–10/group and represented as mean±SEM. * p<0.05, ** p<0.01, *** p<0.001– compared to control group (CTR); G.d. means G. duodenalis.
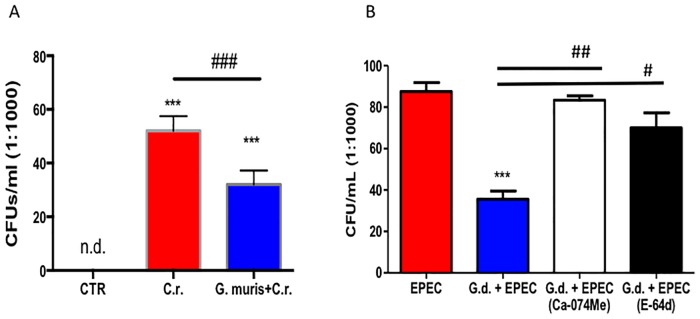
Giardia directly inhibits the growth of A/E pathogens in a protease dependent manner
Another set of studies assessed whether Giardia trophozoites may directly affect A/E bacteria. Direct antibacterial properties of G. muris on C. rodentium and of G. duodenalis on EPEC are illustrated in Fig 7. Giardia significantly inhibited the growth of A/E bacteria: C. rodentium and EPEC survival in vitro was reduced when co-cultured for 3h with Giardia trophozoites (Fig 7). The inhibitory effect on EPEC by G. duodenalis was abolished when trophozoites were pre-treated with cysteine protease inhibitors (Fig 7B).
Fig 7. Giardia directly inhibits the growth of EPEC.
G. muris trophozoites were co-incubated for 3h in Lysogeny broth (LB) media. Bacterial colonies were counted after plating and overnight incubation. (A) G. muris significantly reduces the growth of C. rodentium. (B) G. duodenalis significantly inhibits the growth of EPEC. All data are representative of n = 5–10/group and represented as mean±SEM. * p<0.05, ** p<0.01, *** p<0.001– compared to control group (CTR); # p<0.05, ### p<0.001 versus the corresponding group, indicated by line; n.d. means not detected, that is equivalent to 0; G.d. means G. duodenalis.
Discussion
Our understanding of polymicrobial interactions remains incompletely understood, and the mechanisms by which such infections could either benefit or harm the host remain largely unknown. These mechanisms are commonly involved in infections due to contaminated food or water, and hence carry great significance for child health in countries with limited resources [62]. Recent studies found that in such countries, infection with Giardia appeared to protect children against diarrheal disease via unknown mechanisms [27, 28]. Whether Giardia may modulate the effects of co-infecting enteropathogens has yet to be established. The present report demonstrates that Giardia sp. infections may increase the expression and secretion of AMPs from IECs and protect against at least some A/E gastrointestinal pathogens during co-infection. The release of cathepsin B-like cysteine proteases from Giardia parasites appears to be, at least partially, responsible for inducing the expression of AMPs from IECs. The findings also show that Giardia cysteine proteases are able to directly inhibit the growth of an A/E bacterial pathogen. Together, these effects may explain at least in part how giardiasis may protect against intestinal disease induced by an enteropathogen.
Findings from the present study demonstrate that Giardia infections induce protective responses within the intestinal mucosa that attenuate the severity of disease induced by a co-infecting A/E pathogen. These findings complement previously published observations that Giardia infections modulate host pro-inflammatory responses to pathogenic bacteria and pro-inflammatory stimuli [26, 14, 63], and may explain how Giardia infections can protect against the development of diarrheal disease and reduce the expression of pro-inflammatory markers in children, when compared to children not infected with G. duodenalis [24, 25]. Giardia co-infections have been shown to attenuate the severity of rotavirus-induced diarrheal disease in infants [64]. In contrast, separate research has suggested that Giardia-rotavirus co-infections synergistically increased the incidence and severity of diarrheal disease in affected hosts [25]. Collectively, the data reveal that Giardia infections contain mechanisms capable of attenuating the severity of diarrheal disease induced by a co-infecting GI pathogen. These conflicting studies suggest that G. duodenalis may either enhance or attenuate the severity of diarrheal disease induced by a co-infecting GI pathogen, and highlight the need for additional research in this field.
Differences in disease outcomes may result from parasite genetics and/or genotype associated with particular Giardia isolates. Indeed, G. duodenalis isolates differently modulate host colonic immune responses to bacterial pro-inflammatory toxins [14] and may induce different pathophysiologic responses within hosts [65, 66]. Furthermore, the ability of G. duodenalis to alter pathophysiology may also be dependent on the type of co-infecting gastrointestinal pathogen. For example, in vivo experimental infections have shown that in animals co-infected with Giardia and Trichinella, presence of one parasite increases susceptibility to the other via mechanisms that have yet to be characterized [67]. Giardia infections have also been shown recently to shift the intestinal microbiota and change the biofilm organization of gut bacterial communities [68, 69]. Enteropathogen-induced changes of commensal microbiota are postulated to contribute to host disease [70, 71]. As shifts in the gastrointestinal microbial community have been associated with increased or decreased susceptibility to pathogenic infection [72, 73], research needs to determine whether and how Giardia-induced modulation of the gastrointestinal microbial community may alter susceptibility to infection with various GI pathogens.
Findings from the present study demonstrate that Giardia spp. infections are protective during co-infection with an A/E enteropathogen, in association with parasite-induced release of β-defensins and TFF3 from IECs. AMPs are essential to intestinal homeostasis and antimicrobial defense against invading GI pathogens [34]. A variety of GI pathogens, including Salmonella spp., Shigella spp., C. rodentium, EPEC and enterohemorrhagic EHEC [35–39] are known to activate AMP production. Inhibition of AMP secretion by Paneth cells enhances host susceptibility to infection [74–76]. Previous research has shown that α- and β-defensins can kill Giardia trophozoites in vitro [50]. However, the role of defensins during Giardia infections in vivo remains largely unknown. α-defensins appear to play a redundant role in controlling Giardia parasite burden [51], while murine β-defensin 1 is increased in animals lacking the IL-17A gene, and infected with Giardia parasites [77]. Our study is the first to demonstrate that Giardia spp. infections are capable of upregulating human β-defensin 2 (HBD-2) and mouse β-defensin 3 (MBD-3) in the presence of an A/E pathogen, and of attenuating the disease induced by a co-infecting GI pathogen. This study also shows that Giardia infections increase the expression of another anti-microbial peptide, trefoil factor three (TFF3). Goblet cell mucins and TFF3 play important roles in defending the intestinal mucosa against enteropathogens [60, 78, 79]. Importantly, the findings reported here also demonstrate that Giardia trophozoites have direct anti-bacterial effects via their cathepsin-like cysteine proteases. Mice in which intestinal antimicrobial peptides have been knocked-out are not viable [80, 81]. Additional research is warranted to assess whether the mechanisms of Giardia spp.-mediated resistance against A/E infections may also protect against other enteropathogens. Consistent with the present findings that showed that co-infection with Giardia attenuated C. rodentium-induced colonic elevation of MPO, a well-known marker of granulocyte infiltration, recent findings have reported that Giardia was able to cleave CXCL-8, a potent chemoattractant for neutrophils [26]. These effects may directly translate into an anti-diarrheagenic effect as it has been established that diarrhea caused by EHEC, as well as other pro-inflammatory bacterial enteropathogens, was directly induced by neutrophilic infiltration, independently of toxin production by the bacteria [82]. This may further explain why giardiasis can protect children against diarrheal disease in areas of the World with poor sanitation.
The G. duodenalis genome contains genes for numerous cathepsin cysteine proteases, and their functions are beginning to be understood [52]. Previous research has demonstrated that G. duodenalis cysteine proteases are involved in trophozoite encystation and excystation [54], cleaving intestinal epithelial structural proteins [55], and degrading pro-inflammatory chemokines [26]. Data from the present study establish that G. duodenalis co-infection with EPEC enhances intestinal epithelial beta-defensin and TFF3 production in a parasite cysteine protease-dependent manner, hence adding a novel role for G. duodenalis cathepsin-like cysteine proteases. The exact mechanisms require further clarification. Recent observations indicate that EHEC induces modest HBD-2 expression in human enterocytres in vitro via nuclear factor κB (NF-κB) and p38 MAPK pathways [83]. The effects of Giardia cathepsin cysteine proteases on these pathways to modulate AMPs during co-infection require further investigation. It has also been established that Entamoeba histolytica cysteine proteases activate NLRP3-inflammasome in macrophages [84]. Inflammasome activation is known to play a pivotal role in host defense against A/E pathogens [85], and animals deficient in NLRP3 display altered colonic β-defensin profiles [86]. The effects of Giardia cysteine proteases on inflammasome in the context of parasite-induced activation of AMPs is the topic of ongoing research. Microbial-microbial interactions within the gut are extremely complex, and involve the pathogen, the host, and the microbiota. As it was recently reported that Giardia modifies the gut microbiota [68] more research is needed to identify the role played by the intestinal microbiome in these interactions, as well as the possible difference between Giardia Assemblages A and B.
In conclusion, our study demonstrates that Giardia spp. attenuates the severity of intestinal disease induced by a co-infecting A/E bacterial pathogen. Giardia also directly inhibits the growth of pathogenic bacteria via its cysteine proteases. In addition, we propose that another mechanism leading to protection during a co-infection with A/E pathogens may involve a Giardia cysteine(s) protease(s)-dependent activation of host-defense via expression and secretion of AMPs such as HBD-2 and TFF3. Further research is needed to assess the molecular pathway(s) by which Giardia infection could activate host defensive mechanisms that leads to the activation of AMPs and TFF3 production in the presence of an A/E enteropathogen. Study of the mechanisms whereby microbial-microbial interactions may modulate disease outcome carry great potential for the development of therapeutic strategies in parts of the world with poor sanitation where A/E-induced enterocolitis is common.
Materials and methods
Ethics statement
All animal experiments have been approved by the Animal Care Committee at the university of Calgary (approval certificate #AC13-0067). The committee approved of the procedures described in the protocol and certifies that they are in accordance with the principles outlined in the current guidelines of the Canadian Council on Animal Care.
All isolates used in this study have been used for over 15 years in the laboratory. Therefore, their isolation did not require their approval from an ethical review board at their time of collection.
Giardia parasites and bacterial cultures
G. duodenalis NF Assemblage A was obtained from a water sample during an outbreak in Newfoundland, Canada [87]. Keister’s modified TY1-S-33 media supplemented with piperacillin (Sigma-Aldrich, Oakville, Canada) was used to grow trophozoites to confluence axenically in 15 ml polystyrene tubes (Falcon, NY, USA) at 37°C [88, 89]. G. muris trophozoites were obtained from the duodenal scrapings of CD-1 mice infected with G. muris cysts (provided by Dr. Allan Shostak, University of Alberta, Edmonton, Canada). Five days after cyst inoculation, CD-1 mice were sacrificed and trophozoites were isolated from a 15 cm segment of duodenum and proximal jejunum in sterile TYI-S33 Giardia medium containing 3.0 mg/ml piperacillin (Sigma-Aldrich, Oakville, Canada). After vortex shaking, tube contents were filtered through sterile gauze, centrifuged at 800g for 10 minutes and pellets were incubated in fresh TYI-S33 Giardia medium for 2 hours. G. muris trophozoites were detached by cold PBS, pelleted by centrifugation at 800g for 10 minutes, and diluted in sterile PBS at a concentration of 5.0x106 trophozoites per ml. EPEC strain O127:H6 (typical EPEC strain; provided by R. DeVinney, Microbiology and Infectious Diseases, University of Calgary) and C. rodentium (obtained from Dr. P. Sherman, Hospital of Sick Children, University of Toronto) were grown in Luria-Bertani (LB) broth (BD, Missisauga, Canada) at 37°C to log phase. Bacteria were harvested by centrifugation at 1000g for 10 minutes and re-suspended in appropriate volume of Dublecco’s PBS (Sigma-Aldrich, Oakville, Canada). GFP-labeled C. rodentium bacteria were constructed by chromosomal insertion of gfp (green fluorescent protein) into C. rodentium DBS-100 [61].
Co-infection model in mice
C. rodentium co-infection with G. muris in mice was used to model EPEC co-infection with G. duodenalis in humans. Seven to eight week old C57BL/6 male mice (Charles River, Sherbrooke, Canada) were housed in facilities with 12-hour light/dark cycles and free access to food and water. Animals were infected by oral gavage with 5.0x106 G. muris trophozoites in 0.1 ml of Dulbecco’s PBS (Sigma-Aldrich, Oakville, Canada). One-hour after inoculation, animals were infected with 2.5x108 colony-forming units (CFUs) of GFP-C. rodentium in 0.1 ml of PBS. Mouse body weight and disease activity index (DAI) scores were recorded daily for the next 14 days. DAI included parameters of colitis/gastroenteritis (i.e. soft, liquid, solid feces condition and presence of fecal blood). After 14 days, mice were killed by cervical dislocation and G. muris trophozoites in the duodenum were enumerated using a light microscope and hemocytometer (Hausser Scientific, Horsham, USA). Animal colonic tissues were examined as below and, collected for mRNA analysis, myeloperoxidase (MPO) activity assays, bacterial colonization assays, or fixed in a 4% paraformaldehyde solution for immunofluorescence, fluorescent in situ hybridization, or hematoxylin and eosin staining, as described below. Whole spleen and a part of liver were also collected for bacterial translocation assays (see below).
Macro- and microscopic colitis severity assessment
Animal colons were opened and assessed for macroscopic damage, according to a previously published score scale [90]. Criteria assessed for microscopic damage score are submucosal edema, epithelial hyperplasia, epithelial integrity, neutrophil and mononuclear cell infiltration investigated by light microscopy on hematoxylin-eosin (H&E) sections [91–93]. For each animal, macroscopic and microscopic damage score were assessed blindly by two investigators.
Bacterial translocation assays
Total bacterial colonization of the colon was measured by plating colonic homogenates without luminal content, previously washed with sterile Dulbecco’s PBS (Sigma-Aldrich, Oakville, Canada). Proximal colonic tissue samples were weighted and collected in 2 mL Fast-Prep tubes (MP Biomedicals, Montreal, Canada) containing a mixture of 0.9–2.0 mm stainless steel beads (NextAdvance, NY, USA). Tissues samples were diluted in 1:1000 in PBS and inoculated on LB agar (BD 244520, Mississauga, Canada) plates in aerobic and anaerobic conditions, and CFUs were counted after 24 and 48 h, respectively. Spleen and liver were collected for bacterial translocation assessment as follows: tissues were homogenized using FastPrep24 (MP Biomedicals, Montreal, Canada), after were incubated similarly on LB agar plates aerobically (24 hours) and anaerobically (48 hours) at 37°C, using the AnaeroGen 2,5L packs (Thermoscientific, Ottawa, Canada). Bacterial counts were calculated by enumerating CFUs normalized to tissue or fecal weight. Plating of GFP-C.rodentium cultures from fecal homogenate were done using Columbia blood agar plates (Sigma Aldrich, Oakville, Canada) containing chloramphenicol (30μg/ml).
RNA extraction and quantitative RT-PCR
Total RNA was extracted from proximal colon tissues samples and Caco-2 cells using a QIAGEN RNeasy Mini Kit (QIAGEN, Toronto, Canada) following the manufacturer’s instructions and retrotranscribed by RT-qPCR KIT (QIAGEN, Toronto, Canada). Real-time PCR was conducted with QuantiTect SYBR Green PCR Kit (QIAGEN, Toronto, Canada) on a Rotor Gene 3000 Cycler (QIAGEN, Corbett, Australia) and normalized to β-actin. Primers and reaction conditions for detected genes are given in S1 Table [94–97].
Myeloperoxidase (MPO) analysis
Myeloperoxidase (MPO) activity is a well-established marker of granulocyte infiltration to assay tissue inflammation [98]. On day 14 colon was removed, distal colonic tissue samples (where the highest level of edema in this model was indicated) were weighted, and collected in 2ml Fats-Prep tubes (MP Biomedicals, Montreal, Canada) containing a mixture of 0.9–2.0 mm stainless steel beads (NextAdvance, NY, USA). Tissue samples were suspended in 50 mM potassium phosphate buffer containing 5 mg/mL hexadecyltrimethylammonium bromide (Sigma-Aldrich, Oakville, Canada) at a ratio of 50 mg tissue per 1 mL lysis buffer. Samples were homogenized using a Fast-Prep24 device (MP Biochemicals, Montreal, Canada) at speed 6.0 for 40 seconds. The resulting homogenate solution was collected into pyrogen-free 1.5mL Eppendorf tubes and centrifuged at 10,000x g for 15 minutes at 4°C. 7 μl of supernatant was added to a 96-well plate (ThermoFisher Scientific, Ottawa, Canada) with 200 μL of the reaction mixture (comprised of 0.005 g O-dianisidine (Sigma-Aldrich, Oakville, Canada), 30 mL of distilled H2O, 3.33 mL of potassium phosphate buffer, and 17 mL of 1% H2O2). Using a microplate scanner (SpectraMax M2e, Molecular Devices, Sunnyvale, CA, USA), three absorbance readings at 450 nm were recorded every 30 seconds. MPO activity was measured as units of activity per milligram of tissue, with 1 unit of MPO being defined as the amount required to degrade 1 μmol of H2O2 per minute at room temperature.
Co-infection model using a human intestinal epithelial cell line
The human adenocarcinoma (Caco-2) cell line (ATCC HTB-37, Cedarlane Corporation, ON, Canada) was grown in minimum essential medium eagle media (MEME) (Sigma-Aldrich, Oakville, Canada) supplemented with 100 g/ml of streptomycin, 100 U/ml of penicillin, 200 mM L-glutamine, 5 mM sodium pyruvate, (all from Sigma Aldrich, Oakville, Canada) and 20% heat-inactivated fetal bovine serum (FBS) (VWR, Radnor, USA). Cells were used between passages 25 and 34 and kept at 37°C, 5% CO2, and 96% humidity for all experiments. Confluent Caco-2 monolayers growing in 6-well plates (Falcon, NY, USA) were infected with G. duodenalis NF trophozoites at a multiplicity of infections (MOI) of 10:1 for 1 hour, and exposed to EPEC at an MOI of 100:1 for additional 2 hours.
Caco-2 cells were also grown in 8-well chamber slides pretreated with poly-L-ornithine solution (Sigma-Aldrich, Oakville, Canada) to promote adhesion. Confluent Caco-2 monolayers were infected with G. duodenalis NF trophozoites at an MOI of 10:1 for 1 hour, and EPEC at an MOI of 100:1 for a further 2 hours. Following the incubation period, samples were processed for immunofluorescence (see below). In another set of experiments, G. duodenalis trophozoites were pretreated for 30 minutes with an irreversible cathepsin B specific inhibitor l-3-trans-(propylcarbamoyl)oxirane-2-carbonyl)-l-isoleucyl-l-proline methyl ester (Ca-074Me, Sigma-Aldrich, Oakville, Canada) or broad spectrum cysteine protease inhibitor (2S, 3S)-trans-epoxysuccinyl-l-leucylamido-3-methylbutane ethyl ester (E-64d, Sigma-Aldrich, Oakville, Canada) to final concentrations of 10μM or 1μM, respectively, prior to their administration and co-incubation with EPEC and confluent Caco-2 monolayers; the concentrations of inhibitors used was adapted from previously validated studies [26, 55].
Direct antibacterial effect of Giardia
G. muris trophozoites isolated from mice were co-incubated in 96 wells-plate (ThermoFisher Scientific, Ottawa, Canada) with GFP-C. rodentium CFUs at an MOI of 10:1. G. muris trophozoites and GFP-C. rodentium CFUs were resuspended in 100 μL of Dublecoos’ PBS (Sigma Aldrich, Oakville, Canada). Optical density (600 nm) was recorded for 3 hours every 20 minutes on a microplate reader (BMG Labtech, Guelph, Canada). After reading 10 μL of well content was plated on LB agar plates (BD, Mississauga, Canada) in dilution 1: 1000 and incubated at 37°C, 5% CO2, and 96% humidity for 24 hours. The number of colonies formed were then counted and analyzed.
Plain G. duodenalis trophozoites and pretreated for 30 minutes with specific l-3-trans-(propylcarbamoyl)oxirane-2-carbonyl)-l-isoleucyl-l-proline methyl ester (Ca-074 Me) (Sigma-Aldrich, Oakville, Canada) and nonspecific (2S, 3S)-trans-epoxysuccinyl-l-leucylamido-3-methylbutane ethyl ester (E-64d) (Sigma-Aldrich, Oakville, Canada) cysteine protease inhibitors G. duodenalis trophozoites were isolated from polystyrene tubes at 100% confluency were co-incubated in 96 wells-plate with EPEC at an MOI of 10:1 for 2 hours. G. duodenalis trophozoites and EPEC were resuspended in 100 μL of Dublecco’s PBS (Sigma-Aldrich, Oakville, Canada). Optical density (600 nm) was recorded for 3 hours every hour on a microplate reader (BMG Labtech, Guelph, Canada). After co-incubation 10 μL well content was inoculated on LB agar plates (BD 244520, Mississauga, Canada) in dilution 1:1000 and incubated at 37°C, 5% CO2, and 96% humidity for 24 h. The number of colonies formed were then counted and analyzed.
Immunofluorescence and fluorescence in situ hybridization (FISH)
Formalin-fixed paraffin-embedded colonic tissues were sectioned (6 μm) and analyzed via immunofluorescence and FISH. For FISH analysis, tissue sections were hybridized with 10 ng/mL of a universal bacterial 16S fluorescent rRNA probe, according to previously published protocol [99]. For immunofluorescence, tissue sections were incubated with anti-CR LPS (Biotech Laboratories, Ottawa, Canada), biotinylated goat anti-GFP (GeneTex, Irvine, USA), anti-MBD-3 (Santa Cruz Biotechnology, Dallas, USA), anti-TFF3 (Santa Cruz Biotechnology, Dallas, USA) overnight at 4°C.
Confluent Caco-2 monolayers were fixed with 100% methanol and permeabilized with 0.1% Triton 1% BSA solution in PBS. Primary antibodies were used to detect β defensin-2 (Santa Cruz Biotechnology, Dallas, USA) and TFF3 (Santa Cruz Biotechnology, Dallas, USA). The selectivity of these antibodies has been previously validated [61, 100–102]. Caco2 cells are known to produce low levels of TFF3, and the use of Caco2 enterocytes to detect modulation of TFF3 release has been previously validated [103–105]. Images were acquired using a Nikon epifluorescent microscope, and ImageJ was used for microscopic image analysis.
Statistical analysis
Data were expressed as mean ±SEM. Data representation and statistical analysis were performed using GraphPad Prism 6 software for Macintosh (San Diego, USA). Statistical significance was determined by one-way analysis of variance with Kruskal—Wallis test or by two-way analysis. Comparison between groups was performed using Tukey’s test for multiple comparison analyses. Mann Whitney’s test was used to compare non-parametric data. An associated P value of less than 0.05 was considered significant.
Supporting information
Male C57/Bl6 mice (7–8 week old) were infected with G. muris and C. rodentium (C.r.) separately and in co-infection. On 14th day post-infection, colonic samples were collected and stained. (A-D) Hematoxylin eosin (H&E) staining of colon tissues, representatives from all four groups. (Original magnification = 100x. Scale bar = 100 μm). (E-F) H&E staining of colon tissues, represents data from C. rodentium-infected mice and co-infected group. (Original magnification = 200 x. Scale bar = 50 μm).
(TIF)
Male C57/Bl6 mice (7–8 week old) were infected with G. muris and C. rodentium (C.r.) separately and in co-infection. Colonic samples were collected and analyzed on 14th day post-infection. Anti-GFP-C. rodentium staining represents C. rodentium burden of colon (attachment and translocation). Mucosal surface is indicated by a white dash line (Original magnification = 400x. Scale bar represents 25 μm. Red—bacteria, Green—DAPI). Arrows indicate deep crypt invasion of bacteria to host tissues. All data are representative of n = 5–10/group.
(TIF)
Male C57/Bl6 mice (7–8 week old) were infected with G. muris and C. rodentium (C.r.) separately and in co-infection. On 14th day post-infection, liver samples were plated on lysogeny broth (LB) agar to reveal and count translocated bacteria. All data are representative of n = 5–10/group and represented as mean±SEM. * p<0.05, ** p<0.01, *** p<0.001– compared to control group (CTR) # p<0.05 versus the corresponding group, indicated by line; n.d. means not detected, that is equivalent to 0.
(TIF)
G. duodenalis co-infection with EPEC increased mRNA expression of HBD-2. Cells were incubated with G. duodenalis for 3 hours and co-incubated with EPEC for 2 hours. (A) mRNA level of HBD-2. (B) IF staining for HBD-2. (C) mRNA level of TFF3. (D) IF staining for TFF3. Data is represented as fold change means relative to the control group ± SEM. (Original magnification = 400x. Scale bar = 25 μm. Blue-DAPI, Yellow-HBD-2, Green-Human TFF3). All data are representative of n = 5–10/group and represented as mean±SEM. * p<0.05, ** p<0.01, *** p<0.001– compared to control group (CTR); G.d. means G. duodenalis.
(TIF)
(DOCX)
Acknowledgments
The authors thank Dr. Allan Shostak (University of Alberta) for providing the G. muris, and the support of animal facility staff at the University of Calgary LESARC.
Data Availability
All relevant data are within the paper and its Supporting Information file.
Funding Statement
Funded by Natural Sciences and Engineering Research Council of Canada (NSERC), Discovery Grant #183681-2011, www.nserc-crsng.gc.ca, Natural Sciences and Engineering Research Council of Canada Collaborative Research and Training Experience Program (NSERC CREATE), #413888-2012, www.nserc-crsng.gc.ca, Canadian Institutes of Health Research (CIHR) # 12033, www.cihr.gc.ca/e/193.html, Crohn’s Colitis Canada (CCC) grant in aid of research, #20142017.
References
- 1.Platts-Mills JA, Babji S, Bodhidatta L, Gats J, Haque R, Havt A, et al. Pathogen-specific burdens of cummunity diarrhea in developing countries: A multisite birth cohort study (MAL-ED). Lancet Glob Health 2015;3(9):e564 doi: 10.1016/S2214-109X(15)00151-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hawrelak J. Giardiasis: pathophysiology and management. Altern Med Rev. 2003;8(2):129–42. . [PubMed] [Google Scholar]
- 3.Adam RD. Biology of Giardia lamblia. Clin Microbiol Rev. 2001;14(3):447–75. doi: 10.1128/CMR.14.3.447-475.2001 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ankarklev J, Jerlstrom-Hultqvist J, Ringqvist E, Troell K, Svard SG. Behind the smile: cell biology and disease mechanisms of Giardia species. Nat Rev Microbiol. 2010;8(6):413–22. doi: 10.1038/nrmicro2317 . [DOI] [PubMed] [Google Scholar]
- 5.Cotton JA, Beatty JK, Buret AG. Host parasite interactions and pathophysiology in Giardia infections. Int J Parasitol. 2011;41(9):925–33. doi: 10.1016/j.ijpara.2011.05.002 . [DOI] [PubMed] [Google Scholar]
- 6.WHO guidelines for drinking water quality launched in 2004. http://www.who.int/water_sanitation_health/dwq/gdwq3/en/
- 7.Savioli L, Smith H, Thompson A. Giardia and Cryptosporidium join the 'Neglected Diseases Initiative'. Trends Parasitol. 2006;22(5):203–8. doi: 10.1016/j.pt.2006.02.015 . [DOI] [PubMed] [Google Scholar]
- 8.Feng Y, Xiao L. Zoonotic potential and molecular epidemiology of Giardia species and giardiasis. Clin Microbiol Rev. 2011;24(1):110–40. doi: 10.1128/CMR.00033-10 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Escobedo AA, Hanevik K, Almirall P, Cimerman S, Alfonso M. Management of chronic Giardia infection. Expert Rev Anti Infect Ther. 2014;12(9):1143–57. doi: 10.1586/14787210.2014.942283 . [DOI] [PubMed] [Google Scholar]
- 10.Oberhuber G, Kastner N, Stolte M. Giardiasis: a histologic analysis of 567 cases. Scand J Gastroenterol. 1997;32(1):48–51. . [DOI] [PubMed] [Google Scholar]
- 11.Farthing MJ. Giardiasis. Gastroenterol Clin North Am. 1996;25(3):493–515. . [DOI] [PubMed] [Google Scholar]
- 12.Halliez MC, Buret AG. Extra-intestinal and long term consequences of Giardia duodenalis infections. World J Gastroenterol. 2013;19(47):8974–85. doi: 10.3748/wjg.v19.i47.8974 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Buret AG, S K-E, Chin AC. Giardiasis: pathophysiology and pathogenesis Giardia, the cosmopolitan parasite. Wallingford, UK: CAB International; 2002. p. 109–27. [Google Scholar]
- 14.Cotton JA, Motta JP, Schenck LP, Hirota SA, Beck PL, Buret AG. Giardia duodenalis infection reduces granulocyte infiltration in an in vivo model of bacterial toxin-induced colitis and attenuates inflammation in human intestinal tissue. PLoS One. 2014;9(10):e109087 doi: 10.1371/journal.pone.0109087 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Troeger H, Epple HJ, Schneider T, Wahnschaffe U, Ullrich R, Burchard GD, et al. Effect of chronic Giardia lamblia infection on epithelial transport and barrier function in human duodenum. Gut. 2007;56(3):328–35. doi: 10.1136/gut.2006.100198 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cox FE. Concomitant infections, parasites and immune responses. Parasitology. 2001;122 Suppl:S23–38. . [DOI] [PubMed] [Google Scholar]
- 17.Rall G, Knoll LJ. Development of Complex Models to Study Co- and Polymicrobial Infections and Diseases. Plos Pathogens. 2016;12(9). doi: 10.1371/journal.ppat.1005858 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mukherjee AK, Chowdhury P, Rajendran K, Nozaki T, Ganguly S. Association between Giardia duodenalis and coinfection with other diarrhea-causing pathogens in India. Biomed Res Int. 2014;2014:786480 doi: 10.1155/2014/786480 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Becker-Dreps S, Bucardo F, Vilchez S, Zambrana LE, Liu L, Weber DJ, et al. Etiology of childhood diarrhea after rotavirus vaccine introduction: a prospective, population-based study in Nicaragua. Pediatr Infect Dis J. 2014;33(11):1156–63. doi: 10.1097/INF.0000000000000427 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ankarklev J, Hestvik E, Lebbad M, Lindh J, Kaddu-Mulindwa DH, Andersson JO, et al. Common coinfections of Giardia intestinalis and Helicobacter pylori in non-symptomatic Ugandan children. PLoS Negl Trop Dis. 2012;6(8):e1780 doi: 10.1371/journal.pntd.0001780 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hagel I, Cabrera M, Puccio F, Santaella C, Buvat E, Infante B, et al. Co-infection with Ascaris lumbricoides modulates protective immune responses against Giardia duodenalis in school Venezuelan rural children. Acta Trop. 2011;117(3):189–95. doi: 10.1016/j.actatropica.2010.12.001 . [DOI] [PubMed] [Google Scholar]
- 22.Wang L, Xiao L, Duan L, Ye J, Guo Y, Guo M, et al. Concurrent infections of Giardia duodenalis, Enterocytozoon bieneusi, and Clostridium difficile in children during a cryptosporidiosis outbreak in a pediatric hospital in China. PLoS Negl Trop Dis. 2013;7(9):e2437 doi: 10.1371/journal.pntd.0002437 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Oberhelman RA, Flores-Abuxapqui J, Suarez-Hoil G, Puc-Franco M, Heredia-Navarrete M, Vivas-Rosel M, et al. Asymptomatic salmonellosis among children in day-care centers in Merida, Yucatan, Mexico. Pediatr Infect Dis J. 2001;20(8):792–7. . [DOI] [PubMed] [Google Scholar]
- 24.Fletcher SM, Stark D, Harkness J, Ellis J. Enteric protozoa in the developed world: a public health perspective. Clin Microbiol Rev. 2012;25(3):420–49. doi: 10.1128/CMR.05038-11 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bhavnani D, Goldstick JE, Cevallos W, Trueba G, Eisenberg JN. Synergistic effects between rotavirus and coinfecting pathogens on diarrheal disease: evidence from a community-based study in northwestern Ecuador. Am J Epidemiol. 2012;176(5):387–95. doi: 10.1093/aje/kws220 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cotton JA, Bhargava A, Ferraz JG, Yates RM, Beck PL, Buret AG. Giardia duodenalis cathepsin B proteases degrade intestinal epithelial interleukin-8 and attenuate interleukin-8-induced neutrophil chemotaxis. Infect Immun. 2014;82(7):2772–87. doi: 10.1128/IAI.01771-14 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Veenemans J, Mank T, Ottenhof M, Baidjoe A, Mbugi EV, Demir AY, et al. Protection against diarrhea associated with Giardia intestinalis Is lost with multi-nutrient supplementation: a study in Tanzanian children. PLoS Negl Trop Dis. 2011;5(6):e1158 doi: 10.1371/journal.pntd.0001158 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Muhsen K, Cohen D, Levine MM. Can Giardia lamblia infection lower the risk of acute diarrhea among preschool children? J Trop Pediatr. 2014;60(2):99–103. doi: 10.1093/tropej/fmt085 . [DOI] [PubMed] [Google Scholar]
- 29.Haque R. Human intestinal parasites. J Health Popul Nutr. 2007;25(4):387–91. [PMC free article] [PubMed] [Google Scholar]
- 30.Donowitz JR, Alam M, Kabir M, Ma JZ, Nazib F, Platts-Mills JA, et al. A Prospective Longitudinal Cohort to Investigate the Effects of Early Life Giardiasis on Growth and All Cause Diarrhea. Clin Infect Dis. 2016;63(6):792–7. doi: 10.1093/cid/ciw391 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Griffiths EC, Pedersen AB, Fenton A, Petchey OL. The nature and consequences of coinfection in humans. J Infect. 2011;63(3):200–6. doi: 10.1016/j.jinf.2011.06.005 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zhang SX, Zhou YM, Xu W, Tian LG, Chen JX, Chen SH, et al. Impact of co-infections with enteric pathogens on children suffering from acute diarrhea in southwest China. Infect Dis Poverty. 2016;5(1):64 doi: 10.1186/s40249-016-0157-2 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cotton JA, Amat CB, Buret AG. Disruptions of Host Immunity and Inflammation by Giardia Duodenalis: Potential Consequences for Co-Infections in the Gastro-Intestinal Tract. Pathogens. 2015;4(4):764–92. doi: 10.3390/pathogens4040764 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bevins CL, Salzman NH. Paneth cells, antimicrobial peptides and maintenance of intestinal homeostasis. Nat Rev Microbiol. 2011;9(5):356–68. doi: 10.1038/nrmicro2546 . [DOI] [PubMed] [Google Scholar]
- 35.Muniz LR, Knosp C, Yeretssian G. Intestinal antimicrobial peptides during homeostasis, infection, and disease. Front Immunol. 2012;3:310 doi: 10.3389/fimmu.2012.00310 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Tumanov AV, Koroleva EP, Guo X, Wang Y, Kruglov A, Nedospasov S, et al. Lymphotoxin controls the IL-22 protection pathway in gut innate lymphoid cells during mucosal pathogen challenge. Cell Host Microbe. 2011;10(1):44–53. doi: 10.1016/j.chom.2011.06.002 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.O'Neil DA, Porter EM, Elewaut D, Anderson GM, Eckmann L, Ganz T, et al. Expression and regulation of the human beta-defensins hBD-1 and hBD-2 in intestinal epithelium. J Immunol. 1999;163(12):6718–24. . [PubMed] [Google Scholar]
- 38.Ogushi K, Wada A, Niidome T, Mori N, Oishi K, Nagatake T, et al. Salmonella enteritidis FliC (flagella filament protein) induces human beta-defensin-2 mRNA production by Caco-2 cells. J Biol Chem. 2001;276(32):30521–6. doi: 10.1074/jbc.M011618200 . [DOI] [PubMed] [Google Scholar]
- 39.Hamanaka Y, Nakashima M, Wada A, Ito M, Kurazono H, Hojo H, et al. Expression of human beta-defensin 2 (hBD-2) in Helicobacter pylori induced gastritis: antibacterial effect of hBD-2 against Helicobacter pylori. Gut. 2001;49(4):481–7. doi: 10.1136/gut.49.4.481 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wehkamp J, Schauber J, Stange EF. Defensins and cathelicidins in gastrointestinal infections. Curr Opin Gastroenterol. 2007;23(1):32–8. doi: 10.1097/MOG.0b013e32801182c2 . [DOI] [PubMed] [Google Scholar]
- 41.Bals R, Wang X, Meegalla RL, Wattler S, Weiner DJ, Nehls MC, et al. Mouse beta-defensin 3 is an inducible antimicrobial peptide expressed in the epithelia of multiple organs. Infect Immun. 1999;67(7):3542–7. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Burd RS, Furrer JL, Sullivan J, Smith AL. Murine beta-defensin-3 is an inducible peptide with limited tissue expression and broad-spectrum antimicrobial activity. Shock. 2002;18(5):461–4. . [DOI] [PubMed] [Google Scholar]
- 43.Taupin D, Podolsky DK. Trefoil factors: initiators of mucosal healing. Nat Rev Mol Cell Biol. 2003;4(9):721–32. doi: 10.1038/nrm1203 . [DOI] [PubMed] [Google Scholar]
- 44.Mashimo H, Wu DC, Podolsky DK, Fishman MC. Impaired defense of intestinal mucosa in mice lacking intestinal trefoil factor. Science. 1996;274(5285):262–5. . [DOI] [PubMed] [Google Scholar]
- 45.Kindon H, Pothoulakis C, Thim L, Lynch-Devaney K, Podolsky DK. Trefoil peptide protection of intestinal epithelial barrier function: cooperative interaction with mucin glycoprotein. Gastroenterology. 1995;109(2):516–23. . [DOI] [PubMed] [Google Scholar]
- 46.Wlodarska M, Willing BP, Bravo DM, Finlay BB. Phytonutrient diet supplementation promotes beneficial Clostridia species and intestinal mucus secretion resulting in protection against enteric infection. Sci Rep-Uk. 2015;5 doi: 10.1038/srep09253 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kutta H, May J, Jaehne M, Munscher A, Paulsen FP. Antimicrobial defence mechanisms of the human parotid duct. Journal of Anatomy. 2006;208(5):609–19. doi: 10.1111/j.1469-7580.2006.00567.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Devine DA. Antimicrobial peptides in defence of the oral and respiratory tracts. Mol Immunol. 2003;40(7):431–43. doi: 10.1016/S0161-5890(03)00162-7 [DOI] [PubMed] [Google Scholar]
- 49.Wilson M, McNab R, Henderson B. Mucosal antibacterial defenses In: Wilson M., Macnab R., Henderson B.. Bacterial disease mechanisms: An introduction to cellular microbiology. UK: Cambridge University Press, 2002. pp. 246–54. [Google Scholar]
- 50.Aley SB, Zimmerman M, Hetsko M, Selsted ME, Gillin FD. Killing of Giardia lamblia by cryptdins and cationic neutrophil peptides. Infect Immun. 1994;62(12):5397–403. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Tako EA, Hassimi MF, Li E, Singer SM. Transcriptomic analysis of the host response to Giardia duodenalis infection reveals redundant mechanisms for parasite control. MBio. 2013;4(6):e00660–13. doi: 10.1128/mBio.00660-13 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Aurrecoechea C, Brestelli J, Brunk BP, Carlton JM, Dommer J, Fischer S, et al. GiardiaDB and TrichDB: integrated genomic resources for the eukaryotic protist pathogens Giardia lamblia and Trichomonas vaginalis. Nucleic Acids Res. 2009;37(Database issue):D526–30. doi: 10.1093/nar/gkn631 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Ma'ayeh SY, Brook-Carter PT. Representational difference analysis identifies specific genes in the interaction of Giardia duodenalis with the murine intestinal epithelial cell line, IEC-6. Int J Parasitol. 2012;42(5):501–9. doi: 10.1016/j.ijpara.2012.04.004 . [DOI] [PubMed] [Google Scholar]
- 54.DuBois KN, Abodeely M, Sakanari J, Craik CS, Lee M, McKerrow JH, et al. Identification of the major cysteine protease of Giardia and its role in encystation. J Biol Chem. 2008;283(26):18024–31. doi: 10.1074/jbc.M802133200 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Bhargava A, Cotton JA, Dixon BR, Gedamu L, Yates RM, Buret AG. Giardia duodenalis Surface Cysteine Proteases Induce Cleavage of the Intestinal Epithelial Cytoskeletal Protein Villin via Myosin Light Chain Kinase. PLoS One. 2015;10(9):e0136102 doi: 10.1371/journal.pone.0136102 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Amat C., Motta J-P., Bhargava A., Chadee K., Buret A. Giardia duodenalis depletes goblet cells mucins and degrades MUC2, facilitating bacterial translocation. FASEB 2015; 507.1. [Google Scholar]
- 57.Collins JW, Keeney KM, Crepin VF, Rathinam VA, Fitzgerald KA, Finlay BB, et al. Citrobacter rodentium: infection, inflammation and the microbiota. Nat Rev Microbiol. 2014;12(9):612–23. doi: 10.1038/nrmicro3315 . [DOI] [PubMed] [Google Scholar]
- 58.Willing BP, Vacharaksa A, Croxen M, Thanachayanont T, Finlay BB. Altering host resistance to infections through microbial transplantation. PLoS One. 2011;6(10):e26988 doi: 10.1371/journal.pone.0026988 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Scott KG, Yu LC, Buret AG. Role of CD8+ and CD4+ T lymphocytes in jejunal mucosal injury during murine giardiasis. Infect Immun. 2004;72(6):3536–42. doi: 10.1128/IAI.72.6.3536-3542.2004 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Scott KG, Meddings JB, Kirk DR, Lees-Miller SP, Buret AG. Intestinal infection with Giardia spp. reduces epithelial barrier function in a myosin light chain kinase-dependent fashion. Gastroenterology. 2002;123(4):1179–90. . [DOI] [PubMed] [Google Scholar]
- 61.Bergstrom KS, Kissoon-Singh V, Gibson DL, Ma C, Montero M, Sham HP, et al. Muc2 protects against lethal infectious colitis by disassociating pathogenic and commensal bacteria from the colonic mucosa. PLoS Pathog. 2010;6(5):e1000902 doi: 10.1371/journal.ppat.1000902 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Acosta AM, Chavez CB, Flores JT, Olotegui MP, Pinedo SR, Trigoso DR, et al. The MAL-ED Study: A Multinational and Multidisciplinary Approach to Understand the Relationship Between Enteric Pathogens, Malnutrition, Gut Physiology, Physical Growth, Cognitive Development, and Immune Responses in Infants and Children Up to 2 Years of Age in Resource-Poor Environments. Clinical Infectious Diseases. 2014;59:S193–S206. doi: 10.1093/cid/ciu653 [DOI] [PubMed] [Google Scholar]
- 63.Eckmann L, Laurent F, Langford TD, Hetsko ML, Smith JR, Kagnoff MF, et al. Nitric oxide production by human intestinal epithelial cells and competition for arginine as potential determinants of host defense against the lumen-dwelling pathogen Giardia lamblia. J Immunol. 2000;164(3):1478–87. . [DOI] [PubMed] [Google Scholar]
- 64.Bilenko N, Levy A, Dagan R, Deckelbaum RJ, El-On Y, Fraser D. Does co-infection with Giardia lamblia modulate the clinical characteristics of enteric infections in young children? Eur J Epidemiol. 2004;19(9):877–83. . [DOI] [PubMed] [Google Scholar]
- 65.Bartelt LA, Roche J, Kolling G, Bolick D, Noronha F, Naylor C, et al. Persistent G. lamblia impairs growth in a murine malnutrition model. J Clin Invest. 2013;123(6):2672–84. doi: 10.1172/JCI67294 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Solaymani-Mohammadi S, Singer SM. Host immunity and pathogen strain contribute to intestinal disaccharidase impairment following gut infection. J Immunol. 2011;187(7):3769–75. doi: 10.4049/jimmunol.1100606 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.von Allmen N, Christen S, Forster U, Gottstein B, Welle M, Muller N. Acute trichinellosis increases susceptibility to Giardia lamblia infection in the mouse model. Parasitology. 2006;133(Pt 2):139–49. doi: 10.1017/S0031182006000230 . [DOI] [PubMed] [Google Scholar]
- 68.Beatty JK, Ackierman SV, Motta J-P, Workentine M, Harrison JJ, Bhargava A, et al. Giardia duodenalis induces dysbiosis of human intestinal microbiota biofilms. Int J Parasitol 2017; online http://dx.doi.org/10.1016/j.ijpara.2016.11.010 [DOI] [PubMed] [Google Scholar]
- 69.Stecher B, Hardt WD. The role of microbiota in infectious disease. Trends Microbiol. 2008;16(3):107–14. doi: 10.1016/j.tim.2007.12.008 . [DOI] [PubMed] [Google Scholar]
- 70.Keselman A, Li E, Maloney J, Singer SM. The Microbiota Contributes to CD8+ T Cell Activation and Nutrient Malabsorption following Intestinal Infection with Giardia duodenalis. Infect Immun. 2016;84(10):2853–60. doi: 10.1128/IAI.00348-16 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Reti KL, Tymensen LD, Davis SP, Amrein MW, Buret AG. Campylobacter jejuni increases flagellar expression and adhesion of noninvasive Escherichia coli: effects on enterocytic Toll-like receptor 4 and CXCL-8 expression. Infect Immun. 2015;83(12):4571–81. doi: 10.1128/IAI.00970-15 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Martinez-Medina M, Denizot J, Dreux N, Robin F, Billard E, Bonnet R, et al. Western diet induces dysbiosis with increased E coli in CEABAC10 mice, alters host barrier function favouring AIEC colonisation. Gut. 2014;63(1):116–24. doi: 10.1136/gutjnl-2012-304119 . [DOI] [PubMed] [Google Scholar]
- 73.Schubert AM, Sinani H, Schloss PD. Antibiotic-Induced Alterations of the Murine Gut Microbiota and Subsequent Effects on Colonization Resistance against Clostridium difficile. MBio. 2015;6(4):e00974 doi: 10.1128/mBio.00974-15 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Walker CR, Hautefort I, Dalton JE, Overweg K, Egan CE, Bongaerts RJ, et al. Intestinal intraepithelial lymphocyte-enterocyte crosstalk regulates production of bactericidal angiogenin 4 by Paneth cells upon microbial challenge. PLoS One. 2013;8(12):e84553 doi: 10.1371/journal.pone.0084553 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Wilson CL, Ouellette AJ, Satchell DP, Ayabe T, Lopez-Boado YS, Stratman JL, et al. Regulation of intestinal alpha-defensin activation by the metalloproteinase matrilysin in innate host defense. Science. 1999;286(5437):113–7. . [DOI] [PubMed] [Google Scholar]
- 76.Ayabe T, Satchell DP, Wilson CL, Parks WC, Selsted ME, Ouellette AJ. Secretion of microbicidal alpha-defensins by intestinal Paneth cells in response to bacteria. Nat Immunol. 2000;1(2):113–8. doi: 10.1038/77783 . [DOI] [PubMed] [Google Scholar]
- 77.Dann SM, Manthey CF, Le C, Miyamoto Y, Gima L, Abrahim A, et al. IL-17A promotes protective IgA responses and expression of other potential effectors against the lumen-dwelling enteric parasite Giardia. Exp Parasitol. 2015;156:68–78. doi: 10.1016/j.exppara.2015.06.003 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Zarepour M, Bhullar K, Montero M, Ma C, Huang T, Velcich A, et al. The mucin Muc2 limits pathogen burdens and epithelial barrier dysfunction during Salmonella enterica serovar Typhimurium colitis. Infect Immun. 2013;81(10):3672–83. doi: 10.1128/IAI.00854-13 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Bergstrom KS, Morampudi V, Chan JM, Bhinder G, Lau J, Yang H, et al. Goblet Cell Derived RELM-beta Recruits CD4+ T Cells during Infectious Colitis to Promote Protective Intestinal Epithelial Cell Proliferation. PLoS Pathog. 2015;11(8):e1005108 doi: 10.1371/journal.ppat.1005108 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Beck PL, Ihara E, Hirota SA, MacDonald JA, Meng D, Nanthakumar NN, et al. Exploring the interplay of barrier function and leukocyte recruitment in intestinal inflammation by targeting fucosyltransferase VII and trefoil factor 3. Am J Physiol Gastrointest Liver Physiol. 2010;299(1):G43–53. doi: 10.1152/ajpgi.00228.2009 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Hendrich B, Guy J, Ramsahoye B, Wilson VA, Bird A. Closely related proteins MBD2 and MBD3 play distinctive but interacting roles in mouse development. Genes Dev. 2001;15(6):710–23. doi: 10.1101/gad.194101 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Li Z, Bell C, Buret A, Robins-Browne R, Stiel D, O'Loughlin E. The effect of enterohemorrhagic Escherichia coli O157:H7 on intestinal structure and solute transport in rabbits. Gastroenterology. 1993;104(2):467–74. . [DOI] [PubMed] [Google Scholar]
- 83.Lewis SB, Prior A, Ellis SJ, Cook V, Chan SS, Gelson W, et al. Flagellin Induces beta-Defensin 2 in Human Colonic Ex vivo Infection with Enterohemorrhagic Escherichia coli. Front Cell Infect Microbiol. 2016;6:68 doi: 10.3389/fcimb.2016.00068 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Mortimer L, Moreau F, Cornick S, Chadee K. The NLRP3 Inflammasome Is a Pathogen Sensor for Invasive Entamoeba histolytica via Activation of alpha5beta1 Integrin at the Macrophage-Amebae Intercellular Junction. PLoS Pathog. 2015;11(5):e1004887 doi: 10.1371/journal.ppat.1004887 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Knodler LA, Crowley SM, Sham HP, Yang H, Wrande M, Ma C, et al. Noncanonical inflammasome activation of caspase-4/caspase-11 mediates epithelial defenses against enteric bacterial pathogens. Cell Host Microbe. 2014;16(2):249–56. doi: 10.1016/j.chom.2014.07.002 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Hirota SA, Ng J, Lueng A, Khajah M, Parhar K, Li Y, et al. NLRP3 inflammasome plays a key role in the regulation of intestinal homeostasis. Inflamm Bowel Dis. 2011;17(6):1359–72. doi: 10.1002/ibd.21478 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Chin AC, Teoh DA, Scott KG, Meddings JB, Macnaughton WK, Buret AG. Strain-dependent induction of enterocyte apoptosis by Giardia lamblia disrupts epithelial barrier function in a caspase-3-dependent manner. Infect Immun. 2002;70(7):3673–80. doi: 10.1128/IAI.70.7.3673-3680.2002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Diamond LS, Harlow DR, Cunnick CC. A new medium for the axenic cultivation of Entamoeba histolytica and other Entamoeba. Trans R Soc Trop Med Hyg. 1978;72(4):431–2. . [DOI] [PubMed] [Google Scholar]
- 89.Keister DB. Axenic culture of Giardia lamblia in TYI-S-33 medium supplemented with bile. Trans R Soc Trop Med Hyg. 1983;77(4):487–8. . [DOI] [PubMed] [Google Scholar]
- 90.Motta JP, Bermudez-Humaran LG, Deraison C, Martin L, Rolland C, Rousset P, et al. Food-grade bacteria expressing elafin protect against inflammation and restore colon homeostasis. Sci Transl Med. 2012;4(158):158ra44 doi: 10.1126/scitranslmed.3004212 . [DOI] [PubMed] [Google Scholar]
- 91.Nataro JP, Kaper JB. Diarrheagenic Escherichia coli. Clin Microbiol Rev. 1998;11(1):142–201. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Khan MA, Ma C, Knodler LA, Valdez Y, Rosenberger CM, Deng W, et al. Toll-like receptor 4 contributes to colitis development but not to host defense during Citrobacter rodentium infection in mice. Infect Immun. 2006;74(5):2522–36. doi: 10.1128/IAI.74.5.2522-2536.2006 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Barthel M, Hapfelmeier S, Quintanilla-Martinez L, Kremer M, Rohde M, Hogardt M, et al. Pretreatment of mice with streptomycin provides a Salmonella enterica serovar Typhimurium colitis model that allows analysis of both pathogen and host. Infect Immun. 2003;71(5):2839–58. doi: 10.1128/IAI.71.5.2839-2858.2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Chong KT, Thangavel RR, Tang X. Enhanced expression of murine beta-defensins (MBD-1, -2, -3, and -4) in upper and lower airway mucosa of influenza virus infected mice. Virology. 2008;380(1):136–43. doi: 10.1016/j.virol.2008.07.024 . [DOI] [PubMed] [Google Scholar]
- 95.Bergstrom KS, Guttman JA, Rumi M, Ma C, Bouzari S, Khan MA, et al. Modulation of intestinal goblet cell function during infection by an attaching and effacing bacterial pathogen. Infect Immun. 2008;76(2):796–811. doi: 10.1128/IAI.00093-07 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Zhao Z, Mu ZL, Liu XW, Liu XJ, Jia J, Cai L, et al. Expressions of Antimicrobial Peptides LL-37, Human Beta Defensin-2 and -3 in the Lesions of Cutaneous Tuberculosis and Tuberculids. Chin Med J (Engl). 2016;129(6):696–701. doi: 10.4103/0366-6999.178011 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Huang YG, Li YF, Wang LP, Zhang Y. Aberrant expression of trefoil factor 3 is associated with colorectal carcinoma metastasis. J Cancer Res Ther. 2013;9(3):376–80. doi: 10.4103/0973-1482.119308 . [DOI] [PubMed] [Google Scholar]
- 98.Arndt H., K P, Grisham MB, Gonzalez E, Grander DN. Granulocyte turnover in the feline intestine. Inflammation 1992. p. 549–59. [DOI] [PubMed] [Google Scholar]
- 99.Motta JP, Flannigan KL, Agbor TA, Beatty JK, Blackler RW, Workentine ML, et al. Hydrogen sulfide protects from colitis and restores intestinal microbiota biofilm and mucus production. Inflamm Bowel Dis. 2015;21(5):1006–17. doi: 10.1097/MIB.0000000000000345 . [DOI] [PubMed] [Google Scholar]
- 100.Hernandez C, Santamatilde E, McCreath KJ, Cervera AM, Diez I, Ortiz-Masia D, et al. Induction of trefoil factor (TFF)1, TFF2 and TFF3 by hypoxia is mediated by hypoxia inducible factor-1: implications for gastric mucosal healing. Br J Pharmacol. 2009;156(2):262–72. doi: 10.1111/j.1476-5381.2008.00044.x . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Varoga D, Tohidnezhad M, Paulsen F, Wruck CJ, Brandenburg L, Mentlein R, et al. The role of human beta-defensin-2 in bone. J Anat. 2008;213(6):749–57. doi: 10.1111/j.1469-7580.2008.00992.x . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Wang J, Qin R, Ma Y, Wu H, Peters H, Tyska M, et al. Differential gene expression in normal esophagus and Barrett's esophagus. J Gastroenterol. 2009;44(9):897–911. doi: 10.1007/s00535-009-0082-2 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Wan LYM, Chen ZJ, Shah NP, El-Nezami H. Modulation of Intestinal Epithelial Defense Responses by Probiotic Bacteria. Crit Rev Food Sci. 2016;56(16):2628–41. doi: 10.1080/10408398.2014.905450 [DOI] [PubMed] [Google Scholar]
- 104.Wang YH, Kirpich I, Liu YL, Ma ZH, Barve S, McClain CJ, et al. Lactobacillus rhamnosus GG Treatment Potentiates Intestinal Hypoxia-Inducible Factor, Promotes Intestinal Integrity and Ameliorates Alcohol-Induced Liver Injury. Am J Pathol. 2011;179(6):2866–75. doi: 10.1016/j.ajpath.2011.08.039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Podolsky DK, Gerken G, Eyking A, Cario E. Colitis-Associated Variant of TLR2 Causes Impaired Mucosal Repair Because of TFF3 Deficiency. Gastroenterology. 2009;137(1):209–20. doi: 10.1053/j.gastro.2009.03.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Male C57/Bl6 mice (7–8 week old) were infected with G. muris and C. rodentium (C.r.) separately and in co-infection. On 14th day post-infection, colonic samples were collected and stained. (A-D) Hematoxylin eosin (H&E) staining of colon tissues, representatives from all four groups. (Original magnification = 100x. Scale bar = 100 μm). (E-F) H&E staining of colon tissues, represents data from C. rodentium-infected mice and co-infected group. (Original magnification = 200 x. Scale bar = 50 μm).
(TIF)
Male C57/Bl6 mice (7–8 week old) were infected with G. muris and C. rodentium (C.r.) separately and in co-infection. Colonic samples were collected and analyzed on 14th day post-infection. Anti-GFP-C. rodentium staining represents C. rodentium burden of colon (attachment and translocation). Mucosal surface is indicated by a white dash line (Original magnification = 400x. Scale bar represents 25 μm. Red—bacteria, Green—DAPI). Arrows indicate deep crypt invasion of bacteria to host tissues. All data are representative of n = 5–10/group.
(TIF)
Male C57/Bl6 mice (7–8 week old) were infected with G. muris and C. rodentium (C.r.) separately and in co-infection. On 14th day post-infection, liver samples were plated on lysogeny broth (LB) agar to reveal and count translocated bacteria. All data are representative of n = 5–10/group and represented as mean±SEM. * p<0.05, ** p<0.01, *** p<0.001– compared to control group (CTR) # p<0.05 versus the corresponding group, indicated by line; n.d. means not detected, that is equivalent to 0.
(TIF)
G. duodenalis co-infection with EPEC increased mRNA expression of HBD-2. Cells were incubated with G. duodenalis for 3 hours and co-incubated with EPEC for 2 hours. (A) mRNA level of HBD-2. (B) IF staining for HBD-2. (C) mRNA level of TFF3. (D) IF staining for TFF3. Data is represented as fold change means relative to the control group ± SEM. (Original magnification = 400x. Scale bar = 25 μm. Blue-DAPI, Yellow-HBD-2, Green-Human TFF3). All data are representative of n = 5–10/group and represented as mean±SEM. * p<0.05, ** p<0.01, *** p<0.001– compared to control group (CTR); G.d. means G. duodenalis.
(TIF)
(DOCX)
Data Availability Statement
All relevant data are within the paper and its Supporting Information file.