Figure 6. Aortic root motion and expansion during the cardiac cycle.
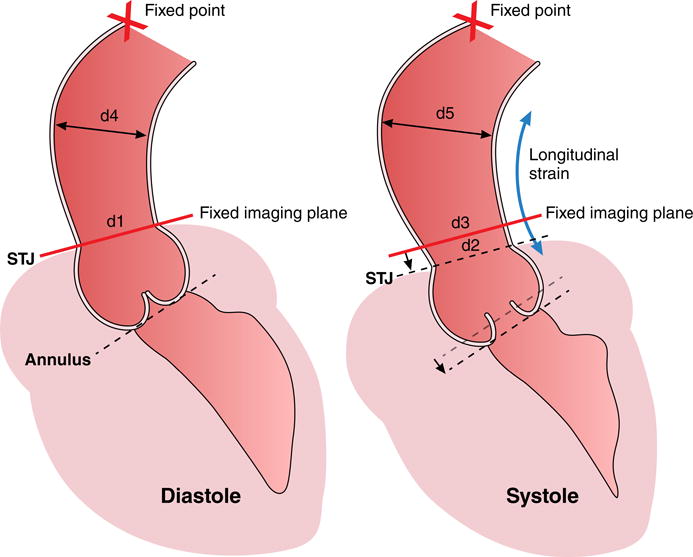
The sinotubular junction (STJ) and annulus show longitudinal strain from diastole to systole as compared to a relative stationary point at the level of the aortic arch (X=fixed point). A fixed imaging plane (as used in MRI) at the level of the STJ in diastole will intersect the ascending aorta more cranially to the STJ in systole due to longitudinal strain of the aortic root. The section of aorta that lies within the diastolic and systolic image planes is flaring out (d4>d1 in diastole and d5>d2 and d3>d2, respectively in systole), leading to overestimation of strain if through-plane motion is ignored. The fixed imaging plane would compute strain as (d3 - d1)/d1. The correct calculation should take (d2 - d1)/d1 and then adjust circumferential strain for longitudinal strain.
A correction for longitudinal strain is not really relevant to PWV but is highly relevant to cross-sectional compliance. Most studies measure the aortic arch length in late diastole, when the aorta is relative static. The arch will get a bit longer in systole, but assuming there is 10% stretch of the ascending segment only (and possibly even a bit of compression of the descending segment since the root is being pulled downward), the error in transit distance will be small (less than half of 10%), so maybe a 5% error in resulting PWV. Furthermore, the foot of the aortic flow wave (used in the transit time method) propagates effectively at diastolic pressure, therefore the diastolic length of the arch is used to compute PWV. On the other hand, if raw circumferential strain is 5% and there is 10% longitudinal strain in the ascending aorta, the true effective circumferential strain would be 5% + (10%/2) = 10%, meaning this results in 100% error.
