Abstract
The objective was to evaluate the characteristics of exposure to OP pesticides and health status in Chilean farm workers from the Maule Region. An occupational health questionnaire was administered in 207 agricultural and non-agricultural workers. For the group of agricultural workers we asked about specific occupational exposure history and symptoms of OP pesticide poisoning. The main health problem of the exposed group was previous OP pesticide poisoning (p <0.001). Fifty-six percent of agricultural workers reported symptoms consistent with acute OP pesticide poisoning. The use of respiratory personal protective equipment and younger age were protective against these symptoms, and number of years of OP pesticide exposure was positively associated with reporting symptoms of poisoning. Of the pesticide applicators 47% reported using chlorpyrifos. The regulations regarding use and application of pesticides should be strengthened, as should training and intervention with workers to improve the use of personal protective equipment.
Keywords: Pesticides, organophosphates, exposure, agricultural workers, occupational hazards
1. Introduction
The exposure of agricultural workers to pesticides is a public health problem worldwide. The annual incidence of acute intoxication from pesticides is approximately 18 per 100,000 full-time farm workers (Thundiyil et al. 2008). A large body of scientific evidence supports the existence of both acute and chronic effects of exposure to organophosphate (OP) pesticides, the most commonly used in chemicals for agricultural pest control, in agricultural workers (Alavanja et al. 2004; Garry 2004; Kamel & Hoppin 2004; Bradman & Whyatt 2005; Rothlein et al. 2006; Engel et al. 2007; Handal et al. 2007; Eskenazi et al. 2008; Jurewicz & Hanke 2008; Rosas & Eskenazi 2008). Acute poisoning ranges from mild to fatal symptoms (Costa 2006), and manifests as headaches, nausea, respiratory problems, vomiting, bradycardia, miosis, dermatitis and burns. Neurotoxic effects are associated with chronic exposures, especially cognitive, motor and sensory deficiencies and neurological diseases (Alavanja et al. 2004; Roldaán-Tapia et al. 2005; Joshaghani et al. 2007). Studies have also found an association between OP pesticide use and emotional disorders (depression and anxiety), breathing difficulties, allergies, endocrine and immunotoxic effects, cancer, fetal abnormalities, and neurobehavioral and developmental delays in children of seasonal workers exposed to OP pesticides (Berkowitz et al. 2004; Eskenazi et al. 2004; Needham 2005; Engel et al. 2007; Eskenazi et al. 2007; Rosas & Eskenazi 2008; Muñoz-Quezada et al. 2013).
In Latin America, and specifically in Chile, there is limited data on OP pesticide exposure and health effects of the workers. Many OP pesticides used in Latin America are banned in the United States, Canada and Europe or their application is strictly regulated and controlled (Muñoz-Quezada et al. 2014). The Maule Region is one of the regions in Chile with the largest rural population and has high rates of OP poisoning (Vallebuona 2006; Muñoz-Quezada et al. 2012).
The main objective of this study was to characterize the exposure to OP pesticides and health status of agricultural and other workers from the Maule Region. Secondarily, variables related to pesticide poisoning symptoms were evaluated in the group of agricultural workers. This information may be used to guide the control and regulation of OP pesticides in Chile and other parts of Latin America.
2. Methods
This study is part of a larger project, which aims to assess the exposure to OP pesticides in agricultural and other workers in the Maule Region, and to estimate the association with neuropsychological and motor performance of workers.
We aimed to recruit a sample of 136 workers, based on a sample size estimation for the detection of mean differences of five points in cognitive functioning between exposed and non exposed workers, as reported by Mackenzie et al. (Mackenzie et al. 2010). The total sample size was based on an estimated 56 workers for each group (n = 112), plus 20% oversampling. Support from public and private institutions was requested to generate a sampling frame for each group. The Agricultural Development Institute (INDAP), a government institution that supports agricultural micro-enterprises, was contacted for the identification of agricultural workers. The group of non-agricultural workers was composed of INDAP’s non-agricultural workers and other educational and health institutions’ workers. Randomly selected workers were administered an informed consent and occupational health questionnaire. The questionnaire was developed based on an examination of exposure to pesticides of the Institute of Public Health of Chile (ISPCH), adding other items to assess exposure characteristics and working conditions of agricultural workers. The Scientific Ethics Committee of the Catholic University of Maule reviewed and approved all contact with human subjects.
The first section of the questionnaire was administered to all subjects and included demographic questions (age, sex, marital status, years of education, health insurance, life partner works in farm, membership in an occupational safety agency); lifestyle questions (alcohol consumption, drug use, smoking, alcoholism); questions about health outcomes (skin allergy, anemia, asthma, cancer, liver damage, depression, diabetes mellitus, epilepsy, arterial hypertension, kidney failure, heart problems, anxiety, previous pesticide poisoning and hospitalization for pesticide poisoning); questions about work history (previous pesticide exposure); and questions about housing (has greenhouse or crops at home, agricultural land owner, distance from home to agricultural land, use of pesticides at home, use of OP pesticides at home).
The second section was administered only to agricultural workers to assess specific occupational exposure to pesticides (whether work involved direct application of pesticides, use of personal protective equipment [PPE], sanitation facilities at work, training on pesticides and application of the acetylcholinesterase tests), and presence of symptoms associated with recent poisoning by exposure to OP pesticides (headache, abdominal pain, vomiting, insomnia, dizziness, lower limb weakness and cramps, shortness of breath, excessive salivation, blurred vision, mood changes, nausea, diarrhea, night sweats, skin lesions and fatigue). We considered a subject to have experienced recent (during the last year) OP pesticide poisoning if they had at least two symptoms associated with exposure to OP pesticides. Finally, a third section of 20 questions were asked only of those reporting work experience as a pesticide applicator.
Data analysis was based on descriptive statistics and frequency distributions. Chi-square tests were used to test whether there was a significant association between the socio-demographic, exposure and occupational variables and health outcomes. The farm-worker group was further divided into those that had a history of applying pesticides and those that did not. Multiple logistic regression models were developed to examine the association between occupational exposure to OP pesticides and reported symptoms of poisoning. Non-agricultural workers were used as the reference group. The variables included in the final model were those that were significantly associated with a p-value ≤ 0.10. STATA version 12.0 (College Station, TX) was used for analysis.
3. Results
We successfully recruited 207 workers, 114 agricultural workers (55.1%) and 93 non-agricultural (44.9%) workers. The mean age of the study population was 49 years and the mean monthly income was $358 USD. Of the agricultural workers, 76 (67%) reported applying pesticides in their work. The socio-demographic characteristics of participants are described in Table 1. The difference between the two groups was significant for all variables.
Table 1.
Socio-demographic characteristics of non-agricultural and agricultural workers of The Maule region, Chile. Frequency, percentage and p-value for the difference between the two groups as tested by the chi-square test are shown.
| Non-agricultural workers n = 93 | Agricultural workers n = 114 | Total n = 207 | P value (<0.05) | |
|---|---|---|---|---|
| n (%) | n (%) | n (%) | ||
| Gender | ||||
| - Male | 31(30) | 74(70) | 105(51) | <0,001 |
| - Female | 66(65) | 40(35) | 102(49) | |
| Marital status | ||||
| - Single or widow | 37(62) | 23(38) | 60(29) | 0.002 |
| - Married or cohabiting partner | 56(38) | 91(62) | 147(71) | |
| Partner works in agriculture | ||||
| - No | 58(54) | 50(46) | 108(53) | 0.007 |
| - Yes | 33(35) | 62(65) | 95(47) | |
| Years of formal education | ||||
| - ≥ 12 years | 57(61) | 36(39) | 93(45) | <0.001 |
| - < 12 years | 36(32) | 78(68) | 114(55) | |
| Health Insurance | ||||
| - Private | 6(88) | 2(12) | 8(4) | 0.018 |
| - Public | 75(47) | 83(53) | 158(79) | |
| - Does not have | 9(26) | 25(74) | 34(17) | |
| Occupational safety agency | ||||
| - Member | 32(67) | 16(33) | 48(23) | 0.002 |
| - Not member | 23(43) | 30(57) | 53(26) | |
| - Does not know | 38(36) | 68(64) | 106(51) | |
| Location where lives and works | ||||
| - Talca | 52(83) | 11(17) | 63(30) | <0.001 |
| - Curicó | 41(28) | 103(72) | 144(70) | |
Workers did not report situations of drug abuse or alcoholism, although 43% percent of workers reported alcohol use (no difference between agricultural versus non-agricultural workers, p= 0.617). With regards to smoking, 25% of non-agricultural workers identify as smokers, compared to 11% of agricultural workers (p = 0.012). Regarding working history, 31% of agricultural workers are seasonal workers, 25% percent are farmers, 18% percent are self-employed in areas non-agricultural, 10% percent are assistants or juniors and the remaining 16% are distributed amongst diverse other jobs.
In reviewing the health status of workers (Table 2), significant differences were observed between the groups only for previous OP pesticide poisoning (p <0.0001).
Table 2.
Health status in non-agricultural (n= 93) and agricultural workers (n= 114) of the Maule region, Chile (frequency, percentage and chi-square test).
| Non-agricultural workers n = 93 | Agricultural workers n = 114 | Total n = 207 | P-value (<0.05) | |
|---|---|---|---|---|
| n (%) | n (%) | n (%) | ||
| Allergies | 9(50) | 9(50) | 18(9) | 0.651 |
| Anemia | 4(57) | 3(43) | 7(3) | 0.509 |
| Asthma | 3(38) | 5(62) | 8(4) | 0.667 |
| Depression | 13(57) | 10(43) | 23(11) | 0.236 |
| Diabetes | 6(43) | 8(57) | 14(7) | 0.872 |
| Hypertension | 18(42) | 25(58) | 43(21 | 0.650 |
| Kidney failure | 2(33) | 4(67) | 6(3) | 0.562 |
| Heart Problems | 4(40) | 6(60) | 10(5) | 0.748 |
| Anxiety | 21(53) | 19(47) | 40(19) | 0.284 |
| Congenital malformation in children | 7(64) | 4(36) | 11(5) | 0.211 |
| Pesticide poisoning | 11(22) | 40(78) | 51(25) | <0.0001 |
| Hospitalization for pesticide poisoning | 1(17) | 5(83) | 6(3) | 0.158 |
Most (98%) agricultural workers reported previous exposure to pesticides, compared to only half of other workers reporting exposure (Table 3).
Table 3.
Occupational exposure and use of pesticides at home in non-agricultural and agricultural workers in the Maule Region, Chile (frequencies, percentages and chi square test).
| Non agricultural workers n = 93 | Agricultural workers n = 114 | Total n = 207 | p-value (<0.05) | |
|---|---|---|---|---|
| n (%) | n (%) | n (%) | ||
| Previous pesticide exposure | 48(30) | 112(70) | 160(77) | <0.0001 |
| Greenhouse or orchard at home | 33(32) | 71(68) | 104(51) | <0.0001 |
| Agricultural land owner | 31(21) | 83(79) | 114(57) | <0.0001 |
| Distance from home to farms <500m (vs. ≥500m) | 46(33) | 93(67) | 139(70) | <0.0001 |
| Pesticide use at home, orchard or garden | 43(30) | 99(70) | 142(69) | <0.0001 |
| OP use at home, orchard or garden | 18(26) | 52(74) | 70(34) | <0.0001 |
When asked about use to particular pesticides, 105 agricultural workers (92%) reported use to one or more pesticides, including OPs (64%), herbicides (32%), pyrethroids (8%), fungicides (11%), other pesticides (14%) or chemicals (copper, fertilizers, hormones, carbamates, etc.) and unspecified pesticides (8.5%). At home, 50% had used pesticides, and 43% used organophosphates. The most frequently reported pesticide used (17.9%) at home was Lorsban, which is a trade name of chlorpyrifos considered as moderately hazardous (Thundiyil et al. 2008; CDC 2009; SAG 2012) and 8.7% reported use of the highly dangerous OP pesticide methamidophos (trade names MTD 600, Tamaron and Monitor) (Thundiyil et al. 2008; CDC 2009; SAG 2012). On average, agricultural workers were exposed to pesticides for 21 (± 1.6) years, compared to 5 (± 0.9) years in other workers (p <0.0001).
The characteristics of both groups and their use of PPE are described in Table 4. Fifty-six percent of agricultural workers showed symptoms of recent (during the last year) OP pesticide poisoning. The most common symptoms included headache (46%), dizziness (19%), blurred vision (15%), lower limb cramps (12%) and shortness of breath (11%). No statistically significant differences in the symptoms of recent poisoning among pesticide applicators versus non-applicators were observed. However, the use of respiratory PPE and younger age were protective factors from symptoms of acute pesticide poisoning, while a greater number of years of exposure to pesticides was associated with a higher likelihood of having symptoms of intoxication for OP pesticides (Table 5).
Table 4.
Socio-demographic characteristics, use of personal protective equipment (PPE) and working conditions of agricultural workers in the Maule Region, Chile. Applicator indicates subjects who reported applying pesticides OP in their work (frequency, percentage and chi square test).
| Non-applicator n = 38 | Applicator n = 76 | Total n = 114 | p-value (0.05) | |
|---|---|---|---|---|
| n (%) | n (%) | n (%) | ||
| Gender | ||||
| - Male | 14(19) | 60(81) | 74(65) | <0.0001 |
| - Female | 24(60) | 16(40) | 40(35) | |
| Age | ||||
| - 49 years or less | 16(33) | 32(67) | 48(42) | 0.999 |
| - More than 49 years | 22(33) | 44(67) | 66(58) | |
| Years of education | ||||
| - Secondary education or higher | 16(44) | 20(56) | 36(32) | 0.087 |
| - Secondary not finished or lower | 22(28) | 56(72) | 78(68) | |
| Use PPE body | 9(20) | 37(80) | 46(41) | 0.013 |
| Use PPE head | 21(34) | 40(66) | 61(54) | 0.791 |
| Use PPE hands | 12(27) | 33(73) | 45(39) | 0.223 |
| Use PPE respiratory | 10(22) | 35(78) | 45(39) | 0.042 |
| Use PPE eyes | 13(28) | 34(72) | 47(41) | 0.282 |
| Use PPE feet | 15(22) | 54(78) | 69(61) | 0.001 |
| PPE frequency of use | ||||
| - Always | 13(48) | 14(52) | 27(24) | 0.150 |
| - Sometimes | 15(31) | 33(69) | 48(42) | |
| - Never | 10(26) | 29(74) | 39(34) | |
| Sanitation facilities | 23(47) | 34(53) | 49(43) | 0.593 |
| Training on pesticide use from occupational safety agency | 8(44) | 10(56) | 18(16) | 0.289 |
| Occupational safety agency tested for Acetyl cholinesterase activity | 12(29) | 30(71) | 42(37) | 0.410 |
Table 5.
Association between symptoms of recent organophosphate (OP) pesticide poisoning* and independent variables (use of respiratory personal protective equipment (PPE), age, years of OP pesticide exposure and whether subject reports application of pesticides for work).
| Poisoning symptoms | OR | P-value (<0.05) | Confidence Interval (95%) | |
|---|---|---|---|---|
| Use of respiratory PPEa | 0.338 | 0.013 | 0.143 | 0.797 |
| Ageb | 0.356 | 0.032 | 0.138 | 0.917 |
| Years of OP pesticide exposurec | 1.030 | 0.043 | 1,000 | 1.060 |
| Applicator status d | 0.935 | 0.887 | 0.373 | 2.343 |
We considered a subject to have poisoning symptoms if they reported at least two symptoms associated with exposure to OP pesticides during the last year.
1= Does not use PPE; 0= Use PPE
0= ≤49 years old, 1= > 49 years old
Continuous variable
1= Pesticide applicator; 0= Non-applicator
In applicators, the mean number of years applying pesticides was 16 (± 1.5). Seventy-nine percent had no pesticide applicator license credentials, 84% performed the mixing and preparation of pesticides, with 88% of those doing so in an open area, and 48% of those used PPE while doing so. Eighty-seven percent work as applicator during the agricultural production season.
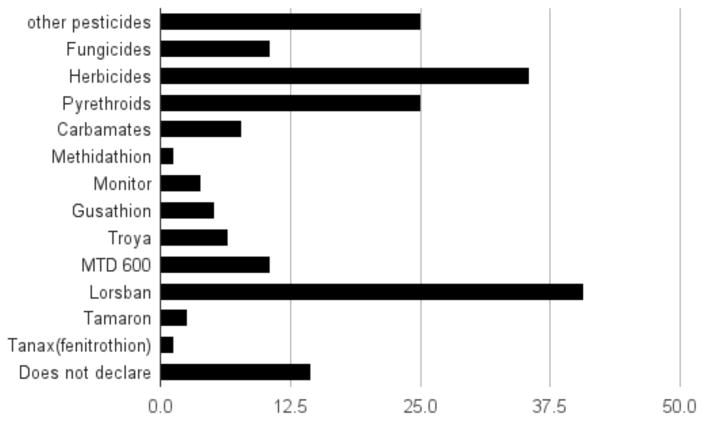
Of the applicators that knew the trade names of pesticides used in 2014, 72.4% reported use of OP pesticides. Figure 1 shows the percentage of pesticides type and OP pesticides reported by the subjects as applied during work. Of the reported pesticides used, 17% reported using the highly dangerous OP methamidophos and 47.4% reported using chlorpyrifos.
Figure 1. Percentages of pesticide type and organophosphate (OP) pesticides* used by applicators (n= 76).
*OP Pesticides: Methidathion, Monitor (Methamidophos), Gusathion (Azinphos methyl), Troya (Chlorpyrifos), MTD 600 (Methamidophos), Lorsban (Chlorpyrifos), Tamaron (Methamidophos) and Tanax (Feniotrothion).
The majority (75%) of pesticide applicators reported that they know the risks of applying pesticides, although only 50% reported receiving training on those risks. With respect to best practices, 91% of applicators used manual backpack sprayers, 50% used a motorized knapsack; 44% cleaned their equipment in a specially equipped location, with the other 56% cleaning their equipment in the yard, orchard or irrigation canals; 70% stored pesticides in a warehouse, 83% reported eating food or smoking when applying pesticides, 28% reported immediately changing work clothes at the end of the application. The average time reported between the end of the application and taking a shower or bath was 52 (± 8.6) minutes.
4. Discussion
The results of this study suggest that agricultural workers from the Maule region, Chile, are exposed to substantial amounts of OP pesticides and a number of other pesticides, many of them without proper protection. Pesticide poisoning is seen primarily in agricultural workers, and almost all agricultural workers reported exposure to pesticides, compared to only half of other workers, with 64% reporting exposure to OPs.
That most workers in this survey do not belong or are unaware of their membership in job security agencies (Table 1) is an indicator of the vulnerability they experience in the workplace. Another socio-demographic characteristic of agricultural workers indicating vulnerability compared to non-agricultural workers are the number of years of formal education. Most have incomplete secondary education or less. Their exposure to neurotoxins, prevention of health effects, and handling of pesticides may be affected by not being able to understand instructions, not knowing how to read or not having information about the effects of these pesticides in the human body and the environment. The results of our survey suggest that many agricultural workers are not fully trained (only 50% of the applicators of pesticides) about the health effects of pesticides, do not use PPE, and store pesticides or clean machinery in unsuitable places for such activities.
With respect to the health status of workers, both groups (agricultural and non-agricultural) have similar health indicators except cigarette smoking, which is higher in non-agricultural workers. The lower consumption of cigarettes in agricultural workers may be explained by their lower earnings compared to other workers, and also the greater accessibility to tobacco in urban areas.
Interestingly, non-agricultural workers also reported some cases of pesticide poisoning. This could be explained possibly by previous employment in the agricultural sector, as even non-agricultural workers report a mean of 5 (± 0.9) years of exposure to pesticides. Our data suggest that the use of PPE is key to preventing symptoms of poisoning, a situation also observed in other studies with similar populations (Lehtola et al. 2008; Salvatore et al. 2009). Regardless of whether an agricultural worker was classified as an applicator or non-applicator of pesticides, the presence of recent (during the last year) symptoms of OP pesticide poisoning was significantly associated with not wearing respiratory PPE, more years of exposure to pesticides, and older age. Most workers use OP pesticides classified as highly or moderately dangerous (Thundiyil et al. 2008; CDC 2009; SAG 2012), these pesticides are associated with symptoms such as neurological disorders and cognitive dysfunctions (Alavanja et al. 2004; Rothlein et al. 2006; Costa 2006). Our results also indicate that the majority of workers receive little training on the effects of pesticides. We suggest that training in safe pesticide handling be carried out amongst all agricultural workers, and respecting the specific cultural context of those workers, as suggested by previous literature (Lehtola et al. 2008; Salvatore et al. 2009; Ospina et al. 2009; Orozco et al. 2011).
Our study was limited by the socio-demographic differences observed between agricultural and non-agricultural workers (gender, years of education, geographic location and socioeconomic status) that make it difficult to compare between the groups. Also, gender differences were observed among agricultural workers between pesticide applicators and non-applicators.
The results of this study demonstrate the lack of health and occupational safety of Chilean farm workers, a finding similar to other developing country contexts (Ospina et al. 2009). Whereas Chile recently was incorporated into the group of developed countries by The World Bank (2015), the status of environmental health in the country still lags behind (Pino et al. 2015). With respect to the safety of agricultural workers, there are no clear policies of protection, exposure control and prevention activities for pesticide handling appropriate to the cultural level and income of rural farmers. Some OP pesticides mentioned by farmers (MTD 600, Tamaron and Monitor, all methamidophos) are classified as highly dangerous (Thundiyil et al. 2008; CDC 2009; SAG 2012), and are banned in other Latin American countries, USA, Canada and Europe (Muñoz-Quezada et al. 2014) due to their high level of toxicity and chronic effects associated with cancer and neurological diseases. In addition, in many countries pesticides like chlorpyrifos are highly regulated and cannot be applied or purchased by any individual. In contrast, in Chile the requirements for a certified applicator license is not linked to permission for restricted purchase of and access to these pesticides, and currently anyone can buy them.
We conclude that in Chile development of policies to address the current vulnerability and risk of farm workers is sorely needed. It is also important to more broadly evaluate the hazards associated with pesticide exposure in agricultural settings, as poor regulation and education in the management of these chemicals can also endanger the environment and consequently the general population (Lehtola et al. 2008; CDC 2009; Salvatore et al. 2009; Oliveira et al. 2012; SAG 2012). This could occur, for example, via inadequate practices in cleaning machines or disposing of pesticide residues into irrigation canals, which could subsequently contaminate crops, humans and animals. Enhanced training and awareness is therefore needed for all those who work in agriculture, not only in pesticide applicators (Salvatore el al. 2009; Oliveira et al. 2012; SAG 2012). Health and agriculture authorities should come together to develop a multidisciplinary task force to address these issues and create clear and specific guidelines and protocols for each stage of the use and handling of pesticides, and not only for the moment of application, which is where interventions have focused to date. This would allow, for example, enhancing the assessment of compliance with restricted entry intervals (REI) and pre-harvest intervals (PHI) and highlight the importance of regulation and control of the reduction of pesticide waste (containers and unused residues).
We also recommend the development of regulations at the legislative level that restrict the use of highly hazardous pesticides, as has already been implemented in developed countries, as well as strict guidelines about the fulfillment of basic requirements for the sale of pesticides, and greater record-keeping requirements, which would enable monitoring of pesticide use nationally.
References
- Alavanja M, Hoppin J, Kamel F. Health effects of chronic pesticide exposure: cancer and neurotoxicity. Annual Review of Public Health. 2004;25:155–197. doi: 10.1146/annurev.publhealth.25.101802.123020. [DOI] [PubMed] [Google Scholar]
- Berkowitz GS, Wetmur JG, Birman-Deych E, Obel J, Lapinski RH, Godbold JH, Holzman IR, Wolff MS. In utero pesticide exposure, maternal paraoxonase activity, and head circumference. Environ Health Perspect. 2004;112: 388–391. doi: 10.1289/ehp.6414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bradman A, Whyatt R. Characterizing Exposures to Nonpersistent Pesticides during Pregnancy and Early Childhood in the National Children’s Study: A Review of Monitoring and Measurement Methodologies. Environ Health Perspect. 2005;113: 1092–1099. doi: 10.1289/ehp.7769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC) [Internet] Fourth National report on human exposure to environmental chemicals. 2009 [cited 2015 oct 20]. Available from: http://www.cdc.gov/exposurereport/pdf/FourthReport.pdf.
- Costa LG. Current issues in organophosphate toxicology. Clin Chim Acta. 2006;366: 1–13. doi: 10.1016/j.cca.2005.10.008. [DOI] [PubMed] [Google Scholar]
- Engel S, Berkowitz G, Barr D, Teitelbaum S, Siskind J, Meisel S. Prenatal organophosphate metabolite and organochlorine levels and performance on the Brazelton Neonatal Behavioral Assessment Scale in a multiethnic pregnancy cohort. Am J Epidemiol. 2007;265: 1397–1404. doi: 10.1093/aje/kwm029. [DOI] [PubMed] [Google Scholar]
- Engel S, Berkowitz G, Barr D, Teitelbaum S, Siskind J, Meisel S. Prenatal organophosphate metabolite and organochlorine levels and performance on the Brazelton Neonatal Behavioral Assessment Scale in a multiethnic pregnancy cohort. Am J Epidemiol. 2007;265: 1397–1404. doi: 10.1093/aje/kwm029. [DOI] [PubMed] [Google Scholar]
- Eskenazi B, Harley K, Bradman A, Weltzien E, Jewell NP, Barr DB, Furlong CE, Holland NT. Association of in utero organophosphate pesticide exposure and fetal growth and length of gestation in an agricultural population. Environ Health Perspect. 2004;112: 1116–1124. doi: 10.1289/ehp.6789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eskenazi B, Marks AR, Bradman A, Harley K, Barr DB, Johnson C, Morgan N, Jewell N. Organophosphate pesticide exposure and neurodevelopment in young Mexican-American children. Environ Health Perspect. 2007;115: 792–798. doi: 10.1289/ehp.9828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eskenazi B, Rosas L, Marks A, Bradman A, Harley K, Holland N, Johnson C, Fenster L, Barr DB. Pesticide toxicology and the developing brain. Basic Clin Pharmacol Toxicol. 2008;102:228–236. doi: 10.1111/j.1742-7843.2007.00171.x. [DOI] [PubMed] [Google Scholar]
- Garry VF. Pesticides and children. Toxicol Appl Pharmacol. 2004;198: 152–163. doi: 10.1016/j.taap.2003.11.027. [DOI] [PubMed] [Google Scholar]
- Handal A, Lozoff B, Breilh J, Siobán H. Effect of community of residence on neurobehavioral development in infants and young children in a flower-growing region of Ecuador. Environ Health Perspect. 2007;115: 128–133. doi: 10.1289/ehp.9261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Instituto de Salud Pública de Chile (ISPCH) [Internet] Protocolo. Examen de salud para aplicaciones de plaguicidas. 2004 [cited 2015 oct 20]. Available from: http://www.ispch.cl/salud_ocup/doc/diagrama_datos.doc.
- Joshaghani HRH, Ahmadi ARA, Mansourian ARA. Effects of occupational exposure in pesticide plant on workers’s serum and erythrocyte cholinesterase activity. Int J Occup Environ Health. 2007;20: 381–385. doi: 10.2478/v10001-007-0039-8. [DOI] [PubMed] [Google Scholar]
- Jurewicz J, Hanke W. Prenatal and childhood exposure to pesticides and neurobehavioral development: Review of epidemiological studies. Int J Occup Med Environ Health. 2008;21: 121–132. doi: 10.2478/v10001-008-0014-z. [DOI] [PubMed] [Google Scholar]
- Kamel F, Hoppin JA. Association of pesticide exposure with neurologic dysfunction and disease. Environ Health Perspect. 2004;112: 950–958. doi: 10.1289/ehp.7135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lehtola MM, Rautiainen RH, Day LM, Schonstein E, Suutarinen J, Salminen S, Verbeek JH. Effectiveness of interventions in preventing injuries in agriculture: a systematic review and meta-analysis. Scand J Work Environ Health. 2008;34: 327–336. doi: 10.5271/sjweh.1279. [DOI] [PubMed] [Google Scholar]
- Mackenzie SJ, Brewin CR, Curran HV, Furlong CE, Abraham-Smith KM, Harrison V. Neuropsychological and psychiatric functioning in sheep farmers exposed to low levels of organophosphate pesticides. Neurotoxicol Teratol. 2010;32:452–459. doi: 10.1016/j.ntt.2010.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muñoz-Quezada MT, Iglesias V, Lucero B, Steenland K, Barr DB, Levy K, Ryan PB, Alvarado S, Concha C. Predictor of exposure to organophosphate pesticide in schoolchildren in the Province of Talca, Chile. Environ Int. 2012;46: 28–36. doi: 10.1016/j.envint.2012.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muñoz-Quezada MT, Lucero BA, Barr DB, Steenland K, Levy K, Ryan PB, Iglesias V, Alvarado S, Concha C, Rojas E, Vega C. Neurodevelopmental effects in children associated with exposure to organophosphate pesticides: A systematic review. Neurotoxicology. 2013;39: 158–168. doi: 10.1016/j.neuro.2013.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muñoz-Quezada MT, Lucero B, Iglesias V, Muñoz MP. Exposure pathways to pesticides in schoolchildren in the Province of Talca, Chile. Gac Sanit. 2014;28: 190–195. doi: 10.1016/j.gaceta.2014.01.003. [DOI] [PubMed] [Google Scholar]
- Needham LL. Assessing exposure to organophosphorus pesticides by biomonitoring in epidemiologic studies of birth outcomes. Environ Health Perspect. 2005;113: 494–498. doi: 10.1289/ehp.7490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oliveira J, Torres P, Roniery J, Zago B, Dutra E. Knowledge, attitudes, practices and biomonitoring of farmers and residents exposed to pesticides in Brazil. Int J Environ Res Public Health. 2012;9:3051–3068. doi: 10.3390/ijerph9093051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orozco F, Cole D, Ibrahim S, Wanigaratne S. Health promotion outcomes associated with a community-based program to reduce pesticide- related riks among small farm households. Health Promotion International. 2011;26: 432–446. doi: 10.1093/heapro/dar006. [DOI] [PubMed] [Google Scholar]
- Ospina J, Manrique-Abril F, Ariza N. Intervención educativa sobre los conocimientos y prácticas referidas a los riesgos laborales en cultivadores de papa en Boyacá, Colombia. Rev salud pública. 2009;11: 182–190. doi: 10.1590/s0124-00642009000200003. [DOI] [PubMed] [Google Scholar]
- Pino P, Iglesias V, Garreaud R, Cortés S, Canals M, Folch W, Burgos S, Levy K, Naeher LP, Steenland K. Chile confronts its environmental future after 25 years of accelerated growth. Annals of Global Health. 2015 doi: 10.1016/j.aogh.2015.06.008. [Internet] [cited 2015 oct 20]. Available from: http://www.annalsofglobalhealth.org/article/S2214-9996(15)01211-4/fulltext. [DOI] [PMC free article] [PubMed]
- Roldán-Tapia L, Parrón T, Sánchez-Santed F. Neuropsychological effects of long-term exposure to organophosphate pesticides. Neurotoxicol Teratol. 2005;27: 259–266. doi: 10.1016/j.ntt.2004.12.002. [DOI] [PubMed] [Google Scholar]
- Rosas L, Eskenazi B. Pesticides and child neurodevelopment. Curr Opin Pediatr. 2008;20: 191–197. doi: 10.1097/MOP.0b013e3282f60a7d. [DOI] [PubMed] [Google Scholar]
- Rosas L, Eskenazi B. Pesticides and child neurodevelopment. Curr Opin Pediatr. 2008;20: 191–197. doi: 10.1097/MOP.0b013e3282f60a7d. [DOI] [PubMed] [Google Scholar]
- Rothlein J, Rohlman D, Lasarev M, Phillips J, Muniz J, McCauley L. Organophosphate pesticide exposure and neurobehavioral performance in agricultural and nonagricultural Hispanic workers. Environ Health Perspect. 2006;114: 691–696. doi: 10.1289/ehp.8182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salvatore A, Chevrier J, Bradman A, Camacho J, López J, Kavanagh-Baird G, Minkler M, Eskenazi B. A community-based participatory worksite intervention to reduce pesticide exposures to farmworkers and their families. Am J Public Health. 2009;99: 578–581. doi: 10.2105/AJPH.2008.149146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Servicio Agrícola Ganadero (SAG). [Internet] Lista de plaguicidas autorizados. 2012 [cited 2015 oct 20]. Available from: http://www.sag.cl/OpenDocs/asp/pagDefault.asp?boton=Doc51&argInstanciaId=51&argCarpetaId=327&argTreeNodosAbiertos=(327)(-51)&argTreeNodoActual=327&argTreeNodoSel=7.
- The World Bank. [Internet] New country classifications. 2013 [cited 2015 oct 20]. Available from: http://data.worldbank.org/news/new-country-classifications.
- Thundiyil JG, Stober J, Besbelli N, Pronczuk J. Acute pesticide poisoning: a proposed classification tool. Bull World Health Organ. 2008;86: 205–209. doi: 10.2471/BLT.08.041814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vallebuona C. Boletin de vigilancia en salud pública. Ministerio de Salud de Chile; 2006. [accessed on 20 October 2015]. Vigilancia de intoxicaciones agudas por plaguicidas. [Internet] [cited 2015 oct 20]. Available from: http://www.rap-al.org/db_files/PlaguiAL_InfoPa_Chile_IntoxAg_2006_VigAmb_25_08.pdf. [Google Scholar]