Figure 3. Examples of Regulated and Dysregulated Inflammatory Reactions in the Pancreas.
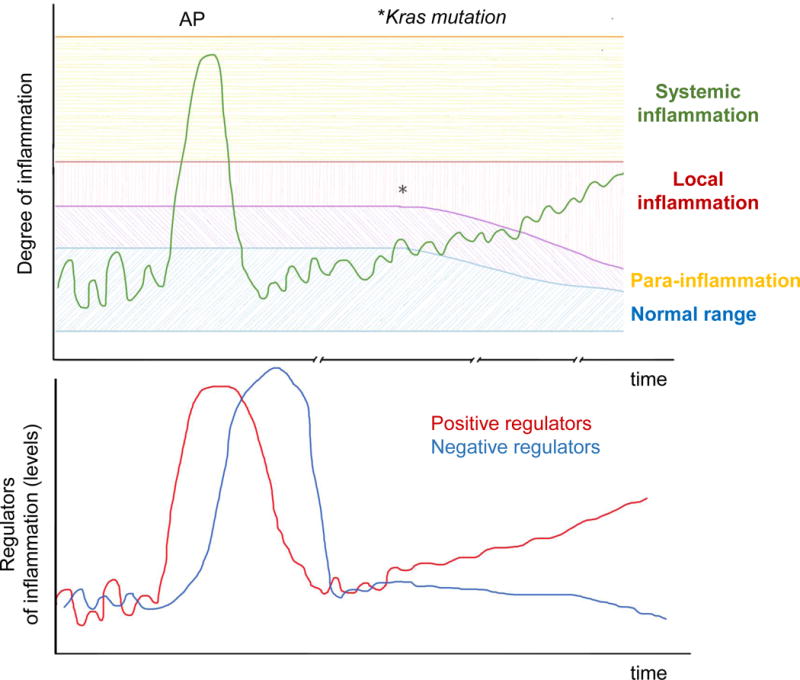
The output of a homeostatic system (e.g. degree of inflammation in the pancreas) can be plotted in a graph against time (top). In healthy tissues, pro-inflammatory mediators and downstream immune responses fluctuate within a narrow “normal range” that are not sufficient to trigger inflammation at the steady state. Cellular stress or injury can trigger an inflammatory reaction of variable magnitude, which can range from a minimal reaction to tissue stress (para-inflammation); to a more pronounced inflammatory reaction to overt cellular injury, as in mild acute pancreatitis (AP), characterized by local inflammation; to a full-blown systemic inflammatory response as seen in severe AP. The inflammatory response is driven by positive regulators (e.g. IL-6), but is eventually tuned down by negative regulators of the system (e.g. IL-10; bottom graph). Therefore, inflammation eventually subsides and the system returns back to normal (homeostasis).
When Kras is mutated, this balance is disturbed in two ways: (i) Kras mutant cells have a lower threshold for release of pro-inflammatory mediators; and (ii) the balance of positive and negative regulators of inflammation is tilted towards one that favors a sustained activation of immunosuppressive and pro-tumorigenic subsets.
Besides pro-inflammatory signals from transformed cells, the tumor-enabling inflammation is further perpetuated by (i) soluble mediators released by stressed non-transformed epithelial cells within the tumor microenvironment; and (ii) systemic promoters of low-grade inflammatory states such as smoking, obesity, and microbial dysbiosis.
