Abstract
Cardiac disease in pregnancy is a challenging clinical problem. The number of women pursuing pregnancy and the underlying complexity of their cardiac disease is increasing, such that heart disease is now the leading cause of maternal mortality in developed countries. Women with congenital heart disease make up the majority of these cases and although maternal mortality is infrequent, a good outcome is only achieved though meticulous multidisciplinary care, beginning with pre-pregnancy counselling. All women with congenital heart disease should be assessed and be referred for pre-conception counselling prior to pregnancy and should receive thorough clinical assessment prior to pregnancy. In some conditions, such as pulmonary hypertension or severe/progressive aortic dilatation, pregnancy is of very high risk and women should be made aware of such risks. In such circumstances, if women choose to proceed with pregnancy, it is paramount that they are cared for by multidisciplinary teams who have experience and expertise of managing such conditions to minimise risks and optimise outcome.
Keywords: Maternal–fetal medicine, cardiology, high-risk pregnancy
Background
The success of surgical techniques and perioperative care have enabled many more babies born with congenital heart disease (CHD) to survive to adulthood.1 Half of these individuals will be women, many of whom will have the desire to start a family themselves. Whilst heart disease is currently the leading cause of direct maternal death in developed countries such as the United Kingdom, most deaths are related to acquired disease and the number of women with CHD who die during pregnancy or the puerperium remains relatively small.2 Indeed, many women who would have been discouraged from considering pregnancy 20 years ago can now be reassured that with appropriate care and expertise, they can expect a successful pregnancy.3 Nevertheless, contemporary data would suggest both obstetric and cardiac complications are much greater than average in this group of women. In this review, we discuss how pre-conception counselling (PCC) should be delivered, what pre-pregnancy diagnostic tools might be employed to better inform PCC and how pregnancy may affect the natural course of different congenital heart lesions, in terms of both immediate and longer term function and prognosis.
Pre-conception counselling
PCC should be offered to all women but particularly to those with underlying medical disorders that may impact upon pregnancy, and when pregnancy may alter the natural disease of their disorder. At present, the evidence that PCC improves outcomes remains limited.4 Furthermore, there are few studies that have assessed how women respond to PCC and whether they themselves find it beneficial.5 Nevertheless, because heart disease remains the leading cause of maternal death in the developed world and because both obstetric and cardiac complications are relatively common in women with CHD,2,3 PCC in this group should be made readily available. Deciding the optimum point at which women should be imparted with this information is unclear, because about one-sixth of all pregnancies in the United Kingdom are unplanned.6 Data from one centre in the United States suggest rates of unplanned pregnancy in women with CHD may exceed 40%.7 This highlights the importance of giving all girls with CHD information regarding pregnancy and contraception as soon as they reach their reproductive years. Every effort should be made to ensure that the transition from paediatric to adult CHD services occurs at the appropriate time and is properly co-ordinated so that these women are not lost to follow-up and can engage with their new medical team as easily and effortlessly as possible.
Many women with CHD have a yearly review and it is important that this includes on each occasion a sensitive discussion regarding pregnancy and/or appropriate contraception, because attitudes often change markedly with time, and it is impossible to predict when each individual woman will become sexually active. Should women express a desire to plan for pregnancy in the near future, then referral to a specific pre-conception clinic is preferable. Work from our own centre has demonstrated that in a cohort of women with a previous Fontan repair many of these women will decide to embark upon pregnancy, even if the advice they are given is guarded.8 Furthermore, prior to our study, we hypothesised that women who had a greater number of complications as a result of their Fontan repair would opt to avoid pregnancy, when compared to those with less severe disease. In fact, there was no difference in the severity of their cardiac condition between those women who opted to try to conceive and those who did not. This implies that other factors may be of greater importance for women in timing their pregnancy other than the severity of their heart disease, for example, pursuing a career, the desire for financial independence before becoming pregnant, and being in a stable relationship.
Many centres including our own now run dedicated clinics where women and their partners can discuss pregnancy in the presence of a cardiologist specialising in adult CHD and an obstetrician specialising in heart disease and pregnancy.9 Wiles et al.5 evaluated this form of combined counselling for women with chronic kidney disease and found that patients reported high levels of satisfaction. During this consultation, women and their partners can be provided with individualised counselling. A recent UK ruling has demonstrated that it is the duty of the healthcare professional to provide women with information about all known risks so that she can make a value judgement of whether to proceed with a pregnancy.10 The ruling said that the level of detail that should be provided must be determined by the patient, and not by the doctor. This is challenging with regard to CHD because of the paucity of large prospective studies, which are underpowered to determine many of the specific risks of pregnancy.11–13
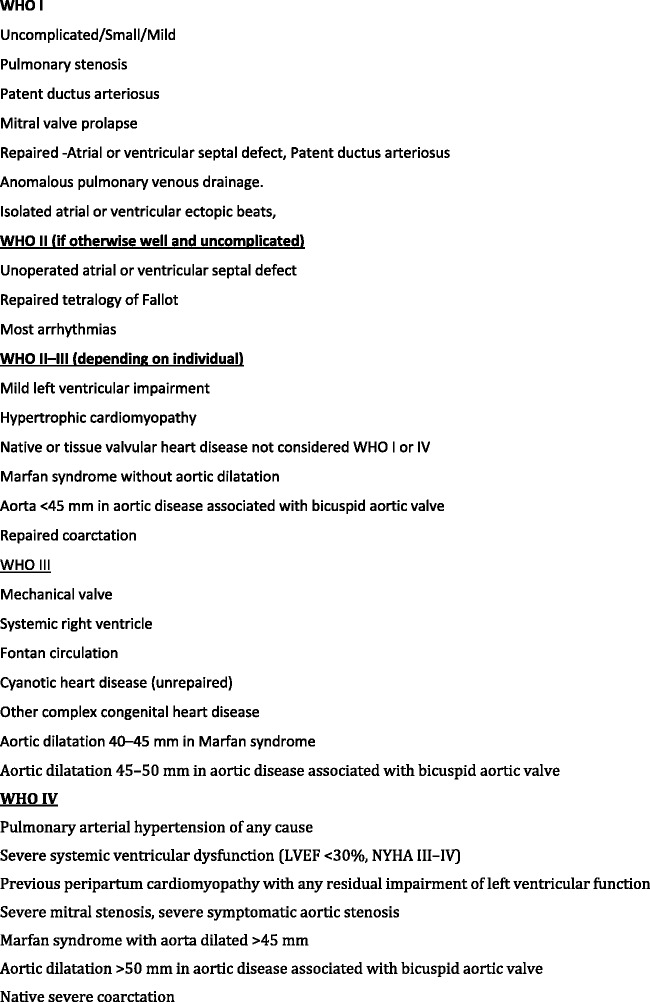
A number of risk stratification systems have been proposed for use in pregnancy and these may aid in counselling. The European Society of Cardiology has suggested its own classification system,14 adapted from the recommendations of a British working group.15 In turn, the latter was based on the WHO classification (Figure 1). Counselling should not only involve a discussion regarding the mother but also the consequences for the fetus, baby and child. Some cardiac lesions such as a Fontan repair are associated with high rates of miscarriage.16 Women who are cyanotic with resting saturations of 85% to 90% have live birth rate of only 45%; this falls to about 12% when saturations are below 85%.17 A recent mutlticentre study from Europe and Asia suggested that rates of miscarriage and stillbirth in women with CHD disease maybe higher than previously reported.18
Figure 1.
Modified World Health Organisation Scoring System (taken from ESC Guideline – Pregnancy and Heart Disease14).
Furthermore, women with CHD are more likely to have a baby born small for gestational age, and preterm delivery is also more common, increasing the risk of neonatal morbidity and mortality.19,20 The chance of the baby being affected by CHD should always be discussed, and some women with CHD will need referral to a geneticist prior to pregnancy. Autosomal dominant conditions where there is a 50% recurrence rate of the condition in the child include Marfans Loeyz Dietz, and Holt–Oram syndromes, and 22q11.2 microdeletion.
Several options are available to detect potentially affected children. For well-characterized genetic disorders, PCC regarding in vitro fertilization and pre-implantation genetic diagnosis may be considered, although invasive and expensive. Once pregnancy has occurred, options to detect congenital heart defects include detailed ultrasound scan imaging usually at 18- to 22-week or genetic analysis with in vitro fertilisation using pre-implantation genetic diagnosis or chorionic villous sampling or amniocentesis (see Table 1). If women choose antenatal testing, they need to understand the importance of prompt attendance to allow these tests to be performed at an appropriate time. In all cases, women and their families should receive appropriate pretest counselling by the relevant experts to ensure they understand the implications of a positive diagnosis.
Table 1.
Modalities for detecting congenital fetal abnormalities.
| Pre-implantation genetic diagnoses |
| Arrhythmogenic Right Ventricular Cardiomyopathy/Dysplasia (ARVC/D), autosomal dominant |
| Catecholaminergic Polymorphic Ventricular Tachycardia (CPVT1) |
| Classical Ehlers–Danlos syndrome |
| Dilated cardiomyopathy and left ventricular noncompaction 5 |
| Dilated cardiomyopathy caused by a mutation in the tropomyosin alpha-1 chain |
| Holt–Oram syndrome |
| Familial hypertrophic cardiomyopathy type 1, 4, 3, 7 and 10 |
| Loeys–Dietz syndrome types 1 and 2 |
| Long QT syndrome types 1, 2, 3, 5 and 6 |
| Marfan syndrome |
| Turner’s syndrome (Mosaic) |
| Fetal Echo |
| Large VSD/complete partial AVSD |
| Aortic stenosis |
| Coarctation |
| Transposition great arteries |
| Pulmonary stenosis |
| Tetralogy of Fallot |
| Hypoplastic left heart |
| Tricuspid atresia |
| Double inlet ventricle |
| Single ventricle circulation |
Those in bold can also be detected via invasive testing.
AVSD: atrioventricular septal defect; VSD: ventricular septal defect.
Subfertility appears to disproportionately affect some groups of women with CHD, such as those with a Fontan repair.21 Although IVF can be successfully undertaken in many women with CHD, the safety of the medications used needs careful consideration. Furthermore, some congenital heart lesions will tolerate poorly the physiological consequences of ovarian hyperstimulation.
In more severe cases, when the risks of going through pregnancy are disproportionately high, clinicians will also need to discuss options such as surrogacy and adoption. Support and referral to the relevant experts and services should be offered in a compassionate manner. Women with more severe forms of CHD will also have a reduced life expectancy and this needs consideration when discussing pregnancy as well as surrogacy and adoption.
Pre-pregnancy assessment
As part of PCC in women with CHD, regular pre-pregnancy cardiovascular assessment and adjustment of management is important to ensure the woman is in the optimum condition to cope with pregnancy. This may involve patient education so that they are aware of which medications need to be discontinued in pregnancy and which may be safely continued. Published data from the Registry of Heart Disease in Pregnancy (ROPAC) would suggest that up to 45% of women with CHD will require cardiac medications during pregnancy. The most commonly used are betablockers, which may be associated with a modest reduction in fetal birthweight.19 Baseline and serial serum B-type natriuretic peptide levels during pregnancy may identify patients with CHD who are more likely to develop heart failure and such measurements can usefully be incorporated into pre-pregnancy assessment.22 Additionally, New York Heart Association functional class and baseline oxygen saturations are also important as they will often guide how well an individual will tolerate the haemodynamic burden of pregnancy.
Echocardiographic assessment forms the core management modality. Being readily available and reproducible, it permits a clear assessment of ventricular function and the underlying severity of cardiac lesions. Women who have an impaired systemic ventricular function (ejection fraction <40%) prior to pregnancy are at greater risk of encountering adverse events during pregnancy.23 Both systolic as well as diastolic function also needs assessment, particularly in lesions associated with left ventricular hypertrophy (e.g. severe aortic stenosis), as the increase in blood volume as a result of pregnancy may be poorly tolerated.
Exercise stress testing in women with CHD prior to pregnancy has shown that women with an abnormal chronotropic response are more likely to an adverse event (both cardiac and neonatal) suggesting impaired adaptation to pregnancy.24 Furthermore, maximum oxygen uptake is a surrogate for cardiac output and may assist risk stratification of the individual patient. Pre-conception exercise stress testing is therefore recommended for women who are NYHA 2 or more.
Estimation of pulmonary pressures is particularly important in women with pulmonary hypertension who choose to embark upon pregnancy (even if they have been advised against pregnancy) because the risk of morbidity is very high.25 Whilst cardiac catheterization prior to pregnancy is not commonly employed, it can assess pulmonary arterial pressure and pulmonary vascular resistance more accurately, which in turn permits better risk stratification for the patient and guides therapy.
Cardiac magnetic resonance (CMR) imaging is another valuable pre-conception investigation, especially in the assessment of women with aortopathy.26 It can be used to determine baseline and any progressive aortic dilatation which assists in risk stratification. If aortic diameter is 50 mm or greater pre-conception surgery may be appropriate, but earlier intervention may be necessary in disorders such as Marfan or Loeys–Dietz syndrome.27
Impact of pregnancy on cardiac function
Providing comprehensive care and advice for women with CHD goes beyond the immediate pregnancy. Women need (and usually want) to know how many healthy years they have ahead of them, and the risks attached to any subsequent pregnancy. This has major implications for the whole family, not just for the woman herself.
Immediate effect of pregnancy on cardiac function
Atrial arrhythmia is commonly encountered and well usually well tolerated in most women with CHD during pregnancy. Atrial ectopy and to a lesser degree supraventricular tachycardias are more common in pregnancy if a patient has reported them previously. Drug therapy may need to be instigated in some cases. Data from ROPAC reveal that heart failure, and ventricular arrhythmia are more common in women with CHD when compared to healthy controls.28 Eight percent of the women with CHD in their study developed heart failure whilst 2.3% developed arrhythmia during pregnancy or the puerperium.29 Further studies have shown that an increased incidence of heart failure during pregnancy is predicted by heart failure prior to pregnancy, a NYHA Score ≥2, and/or the presence of pulmonary hypertension.23 ROPAC demonstrated that median onset of heart failure was 31 weeks, but this was not the peak time of incidence, the incidence was bimodal with two periods of most likely onset, one between 23–30 weeks and the other 1 week postpartum.28 Maternal mortality was higher in women who developed heart failure. In another study, ventricular tachyarrhythmia (VTA) was less common and complicated about 1.4% of all pregnancies with cardiac disease, the majority of these being in women with CHD.29 VTA mainly occurs in the third trimester and may be predicted by women who have a baseline NYHA Score >1. In their study, the ROPAC investigators did not observe an increase in maternal mortality in pregnancy as a result of VTA.29
Longer term effect
At present, prospective studies are still small and underpowered and do not have sufficient length of follow-up to reveal the true impact of pregnancy on long-term cardiovascular function in women with CHD. Recent work from the ZAHARA group showed that when women with CHD were followed longitudinally during pregnancy and up to one year postnatally and were compared with women without CHD, the changes observed during and after pregnancy with regard to ventricular function were comparable.30 Whilst this study was prospective and a control group was identified, follow-up was limited to a year. In the medium term, Balint et al.31 demonstrated that for women with CHD, adverse cardiac events (such as arrhythmias and congestive heart failure) during pregnancy were associated with an increased risk of another cardiac event occurring up to five years later. Unfortunately, the study did not have a control group so the overall risk that pregnancy contributed to these events could not be accurately assessed.
In women with repaired Tetralogy of Fallot, Uebing et al.32 showed on echocardiography at a mean follow-up interval of 2.9 years that there was an increase in right ventricular size as a result of pregnancy not seen in control women who had not been pregnant.32 However, this study was retrospective, utilized solely echocardiography and involved a relatively small number of subjects. More recently, Assenza et al.33 demonstrated with CMR that there is an accelerated rate of right ventricular remodelling as a result of pregnancy compared to controls, particularly seen in women with dilated right ventricular volumes prior to pregnancy. Unpublished data from our group suggests a minimal change in ventricular volumes in this cohort, but that women who have large right ventricular volumes going into pregnancy have a greater degree of right ventricular change after pregnancy.34 For women who have bioprosthetic valves, current evidence suggests no medium-term adverse effect on valve function as a result of pregnancy.35 Progressive aortic dilatation is a well-recognized feature of pregnancy in women with Marfan’s syndrome, where the mean increase in diameter during pregnancy is 3 mm.36 Aortic diameters fell post-pregnancy but remained greater than baseline. Prior reports have raised concerns regarding the ability of a systemic right ventricle to support the additional volume load of pregnancy, and previous studies have shown clinical deterioration during pregnancy in these patients.37 Bowater et al.37 demonstrated that at a mean 51-month post-pregnancy follow-up, women with systemic RV had a decline in RV function measured by echocardiography, and worse NYHA scores when compared with matched non-pregnant controls. However, their study only included 18 women, some of whom had repeated pregnancies, which may influenced their findings. As the spectrum of CHD is vast, for many women such as those with a Fontan palliation, we lack adequate follow-up data to understand what the medium to long-term impact of pregnancy is on single ventricular function.38
Summary
Management of CHD and pregnancy is an evolving field. We need to improve access to services to enable all women to attend PCC. For women with severe heart disease, this can be literally vital. Most women can be reassured that a positive pregnancy outcome is likely, although the risk of (manageable) complications is relatively high and they need to take into account the increased likelihood of preterm birth and fetal growth restriction. An in-depth pre-pregnancy assessment is highly advisable to optimise the women’s condition prior to pregnancy and to assist in planning pregnancy care. Greater collaboration and much more research into the impact of pregnancy on heart function and prognosis is necessary. The work of groups such as ROPAC is to be commended. Going forward, the emphasis should be on prospective multicentre studies with longer period of follow-up of the effects of pregnancy on long-term cardiovascular health.
Declaration of conflicting interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Guarantor
MC
Contributorship
MC conceived the article and wrote the first draft, PJ revised this draft as did MG. All authors approved the final version.
References
- 1.Gilboa SM, Salemi JL, Nembhard WN, et al. Mortality resulting from congenital heart disease among children and adults in the United States, 1999 to 2006. Circulation 2010; 122: 2254–2263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.EMBRRACE UK – Mothers and babies reducing risks through audit and confidential enquiries across the UK, https://www.npeu.ox.ac.uk/mbrrace-uk/reports (accessed 10 September 2016).
- 3.Roos-Hesselink JW, Ruys TP, Stein JI, et al. ROPAC Investigators. Outcome of pregnancy in patients with structural or ischaemic heart disease: results of a registry of the European Society of Cardiology. Eur Heart J 2013; 34: 657–665. [DOI] [PubMed] [Google Scholar]
- 4.Shannon GD, Alberg C, Nacul L, et al. Preconception healthcare and congenital disorders: systematic review of the effectiveness of preconception care programs in the prevention of congenital disorders. Matern Child Health J 2014; 18: 1354–1379. [DOI] [PubMed] [Google Scholar]
- 5.Wiles KS, Bramham K, Vais A, et al. Pre-pregnancy counselling for women with chronic kidney disease: a retrospective analysis of nine years’ experience. BMC Nephrol 2015; 16: 28–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wellings K, Jones KG, Mercer CH, et al. The prevalence of unplanned pregnancy and associated factors in Britain: findings from the third National Survey of Sexual Attitudes and Lifestyles (Natsal-3). Lancet 2013; 382: 1807–1816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lindley KJ, Madden T, Cahill AG, et al. Contraceptive use and unintended pregnancy in women with congenital heart disease. Obstet Gynecol 2015; 126: 363–369. [DOI] [PubMed] [Google Scholar]
- 8.Cauldwell M, Von Klemperer K, Uebing A, et al. A cohort study of women with a Fontan circulation undergoing preconception counselling. Heart 2016; 102: 534–540. [DOI] [PubMed] [Google Scholar]
- 9.Cauldwell M, Patel R, Steer P, et al. A time for greater investment into care for pregnancy and heart disease. Int J Cardiol 2016; 221: 642–643. [DOI] [PubMed] [Google Scholar]
- 10.Montgomery (Appellant) v Lanarkshire Health Board (Respondent) (Scotland), 2015, UKSC, https://www.supremecourt.uk/decided-cases/docs/UKSC_2013_0136_Judgment.pdf.
- 11.Heuvelman HJ, Arabkhani B, Cornette JM, et al. Pregnancy outcomes in women with aortic valve substitutes. Am J Cardiol 2013; 111: 382–387. [DOI] [PubMed] [Google Scholar]
- 12.Hassan N, Patenaude V, Oddy L, et al. Pregnancy outcomes in Marfan syndrome: a retrospective cohort study. Am J Perinatol 2015; 30: 123–130. [DOI] [PubMed] [Google Scholar]
- 13.Gelson E, Curry R, Gatzoulis MA, et al. Pregnancy in women with a systemic right ventricle after surgically and congenitally corrected transposition of the great arteries. Eur J Obstet Gynecol Reprod Biol 2011; 155: 146–149. [DOI] [PubMed] [Google Scholar]
- 14.Regitz-Zagrosek V, Blomstrom Lundqvist C, Borghi C, et al. ESC Guidelines on the management of cardiovascular diseases during pregnancy: the Task Force on the Management of Cardiovascular Diseases during Pregnancy of the European Society of Cardiology (ESC). Eur Heart J 2011; 32: 3147–3197. [DOI] [PubMed] [Google Scholar]
- 15.Thorne S, Nelson-Piercy C, MacGregor A, et al. Pregnancy and contraception in heart disease and pulmonary arterial hypertension. J Fam Plann Reprod Health Care 2006; 32: 75–81. [DOI] [PubMed] [Google Scholar]
- 16.Pundi KN, Pundi K, Johnson JN, et al. Contraception practices and pregnancy outcome in patients after fontan operation. Congenit Heart Dis 2016; 11: 63–70. [DOI] [PubMed] [Google Scholar]
- 17.Presbitero P, Somerville J, Stone S, et al. Pregnancy in cyanotic congenital heart disease. Outcome of mother and fetus. Circulation 1994; 89: 2673–2676. [DOI] [PubMed] [Google Scholar]
- 18.Koerten MA, Niwa K, Szatmári A, et al. Frequency of Miscarriage/stillbirth and terminations of pregnancy among women with congenital heart disease in Germany, Hungary and Japan. Circ J 2016; 80: 1846–1851. [DOI] [PubMed] [Google Scholar]
- 19.Gelson E, Curry R, Gatzoulis MA, et al. Effect of maternal heart disease on fetal growth. Obstet Gynecol 2011; 117: 886–891. [DOI] [PubMed] [Google Scholar]
- 20.de Laat MW, Pieper PG, Oudijk MA, et al. The clinical and molecular relations between idiopathic preterm labor and maternal congenital heart defects. Reprod Sci 2013; 20: 190–201. [DOI] [PubMed] [Google Scholar]
- 21.Drenthen W, Pieper PG, Roos-Hesselink JW, et al. ZAHARA Investigators. Pregnancy and delivery in women after Fontan palliation. Heart 2006; 92: 1290–1294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kampman MA, Balci A, van Veldhuisen DJ, et al. ZAHARA II Investigators. N-terminal pro-B-type natriuretic peptide predicts cardiovascular complications in pregnant women with congenital heart disease. Eur Heart J 2014; 35: 708–715. [DOI] [PubMed] [Google Scholar]
- 23.Siu SC, Sermer M, Colman JM, et al. Prospective multicenter study of pregnancy outcomes in women with heart disease. Circulation 2001; 104: 515–521. [DOI] [PubMed] [Google Scholar]
- 24.Lui GK, Silversides CK, Khairy P, et al. Heart rate response during exercise and pregnancy outcome in women with congenital heart disease. Circulation 2011; 123: 242–248. [DOI] [PubMed] [Google Scholar]
- 25.Ladouceur M, Benoit L, Radojevic J, et al. Pregnancy outcomes in patients with pulmonary arterial hypertension associated with congenital heart disease. Heart 2016. DOI: 10.1136/heartjnl-2016-310003. [DOI] [PubMed]
- 26.Stewart FM. Marfan’s syndrome and other aortopathies in pregnancy. Obstet Med 2013; 6: 112–119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Nejatian A, Yu J, Geva T, et al. Aortic measurements in patients with aortopathy are larger and more reproducible by cardiac magnetic resonance compared with echocardiography. Pediatr Cardiol 2015; 36: 1761–1773. [DOI] [PubMed] [Google Scholar]
- 28.Ruys TP, Roos-Hesselink JW, Hall R, et al. Heart failure in pregnant women with cardiac disease: data from the ROPAC. Heart 2014; 100: 231–238. [DOI] [PubMed] [Google Scholar]
- 29.Ertekin E, van Hagen IM, Salam AM, et al. Ventricular tachyarrhythmia during pregnancy in women with heart disease: data from the ROPAC, a registry from the European Society of Cardiology. Int J Cardiol 2016; 220: 131–136. [DOI] [PubMed] [Google Scholar]
- 30.Kampman MA, Valente MA, van Melle JP, et al. ZAHARA II investigators. Cardiac adaption during pregnancy in women with congenital heart disease and healthy women. Heart 2016; 102: 1302–1308. [DOI] [PubMed] [Google Scholar]
- 31.Balint OH, Siu SC, Mason J, et al. Cardiac outcomes after pregnancy in women with congenital heart disease. Heart 2010; 96: 1656–1661. [DOI] [PubMed] [Google Scholar]
- 32.Uebing A, Arvanitis P, Li W, et al. Effect of pregnancy on clinical status and ventricular function in women with heart disease. Int J Cardiol 2010; 139: 50–59. [DOI] [PubMed] [Google Scholar]
- 33.Assenza GE, Cassater D, Landzberg M, et al. The effects of pregnancy on right ventricular remodeling in women with repaired Tetralogy of Fallot. Int J Cardiol 2013; 168: 1847–1852. [DOI] [PubMed] [Google Scholar]
- 34.Cauldwell M, Quail M, Heng E, et al. Effect of pregnancy on ventricular and aortic dimensions in repaired Tetralogy of Fallot. In: Presented at MacDonald obstetric medicine society, Oxford, 21 September 2016.
- 35.Lawley CM, Lain SJ, Algert CS, et al. Prosthetic heart valves in pregnancy, outcomes for women and their babies: a systematic review and meta-analysis. BJOG 2015; 122: 1446–1455. [DOI] [PubMed] [Google Scholar]
- 36.Roman MJ, Pugh NL, Hendershot TP, et al. Aortic complications associated with pregnancy in Marfan Syndrome: the NHLBI National Registry of genetically triggered thoracic aortic aneurysms and cardiovascular conditions (GenTAC). J Am Heart Assoc 2016; 5: e004052–e004052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bowater SE, Selman TJ, Hudsmith LE, et al. Long-term outcome following pregnancy in women with a systemic right ventricle: is the deterioration due to pregnancy or a consequence of time? Congenit Heart Dis 2013; 8: 302–307. [DOI] [PubMed] [Google Scholar]
- 38.Zentner D, Kotevski A, King I, et al. Fertility and pregnancy in the Fontan population. Int J Cardiol 2016; 208: 97–101. [DOI] [PubMed] [Google Scholar]