Abstract
Cholangiocarcinoma is an epithelial malignancy arising in the region between the intrahepatic bile ducts and the ampulla of Vater at the distal end of the common bile duct. The effect of current chemotherapy regimens against cholangiocarcinoma is limited, and the prognosis of patients with cholangiocarcinoma is poor. Aberrant DNA methylation and histone modification induce silencing of tumor suppressor genes and chromosomal instability during carcinogenesis. Studies have shown that the tumor suppressor genes and microRNAs (miRNAs) including MLH1, p14, p16, death-associated protein kinase (DAPK), miR-370 and miR-376c are frequently methylated in cholangiocarcinoma. Silencing of these tumor suppressor genes and miRNAs plays critical roles in the initiation and progression of cholangiocarcinoma. In addition, recent studies have demonstrated that DNA methylation inhibitors induce expression of endogenous retroviruses and exert the anti-tumor effect of via an anti-viral immune response. Aberrant DNA methylation of tumor suppressor genes and miRNAs could be a powerful biomarker for the diagnosis and treatment of cholangiocarcinoma. Epigenetic therapy with DNA methylation inhibitors holds considerable promise for the treatment of cholangiocarcinoma through the reactivation of tumor suppressor genes and miRNAs as well as the induction of an anti-viral immune response.
Keywords: cholangiocarcinoma, DNA methylation, tumor suppressor gene, microRNA, endogenous retrovirus, anti-viral immune response
1. Introduction
Cholangiocarcinoma is an epithelial malignancy arising in the region between the intrahepatic bile ducts and the ampulla of Vater at the distal end of the common bile duct. The classification of cholangiocarcinoma is based on the anatomical location of tumors and includes intrahepatic, perihilar and distal cholangiocarcinoma [1]. Intrahepatic cholangiocarcinoma is defined as a cholangiocarcinoma located proximally to the second degree bile ducts in the liver. Perihilar cholangiocarcinoma is located between the second degree bile ducts and the insertion of the cystic duct into the common bile duct, whereas distal cholangiocarcinoma is located between the origin of the cystic duct and the ampulla of Vater [1]. Regarding pathological findings, most cholangiocarcinomas are well, moderately, and poorly differentiated adenocarcinomas [1].
The number of cholangiocarcinoma patients is apparently increasing worldwide. Most of cholangiocarcinomas are clinically silent, which makes early diagnosis difficult. Several imaging modalities including computed tomography (CT) and magnetic resonance imaging (MRI) as well as serological tests including serum CA19-9 concentration are helpful for the diagnosis of cholangiocarcinoma. However, these imaging modalities are not always reliable for the diagnosis of cholangiocarcinoma, and the sensitivity and specificity of these biomarkers is low [2]. The five-year survival rates are approximately 20%, as most of patients are diagnosed at an advanced stage. Although patients with cholangiocarcinoma receive chemotherapy regimens including cisplatin and gemcitabine, the effect of these chemotherapies is limited. Thus, the development of new biomarkers and therapeutic strategies against cholangiocarcinoma is urgently needed [2].
Epigenetics is an acquired modification of chromatin DNA or histone proteins such as DNA methylation and histone modification, which regulates downstream gene expression without an alteration in the DNA sequence [3]. Epigenetic alterations can be induced by aging and chronic inflammation. Aberrant DNA methylation and histone modification induce silencing of tumor suppressor genes and chromosomal instability, leading to the initiation and progression of various cancers [4,5,6,7]. MicroRNAs (miRNAs) are small non-coding RNAs that act as endogenous silencers of various target genes. miRNAs are expressed in a tissue-specific manner and play important roles in cell proliferation, apoptosis, and differentiation. We and other groups have revealed that epigenetic alterations including DNA methylation regulate not only protein-coding genes but also non-coding genes such as miRNAs in cancer cells [8,9,10,11].
Epigenetic drugs such as DNA methylation inhibitors and histone deacetylase (HDAC) inhibitors have clinical promise for cancer therapy [3,12,13]. Aberrant DNA methylation at CpG island promoters of tumor suppressor genes is frequently observed in various human malignancies including cholangiocarcinoma. The DNA methylation inhibitor 5-aza-2′-deoxycytidine (5-Aza-CdR), which is an analog of cytidine, was recently approved for the treatment of myelodysplastic syndrome (MDS). However, the effect of DNA methylation inhibitors on patients with cholangiocarcinoma remains to be elucidated. In this review, we summarize the current knowledge regarding aberrant DNA methylation of important tumor suppressor genes and miRNAs in cholangiocarcinoma as well as effects of DNA methylation inhibitors on cholangiocarcinoma.
2. Aberrant DNA Methylation as a Biomarker of Cholangiocarcinoma
Malignant tumors developing in the biliary tract are difficult to diagnose at an early stage because of their anatomical locations. In addition, useful biomarkers for biliary tract cancers have not been developed. Most cholangiocarcinoma patients are diagnosed at an advanced stage, and aggressive cancers easily infiltrate surrounding organs and become unresectable. The early detection of cholangiocarcinoma might improve the prognosis of patients, and the development of useful biomarkers of cholangiocarcinoma would be beneficial for prompt and more effective treatment. One of the most powerful biomarkers in cancer is DNA methylation of tumor suppressor genes. We summarized genes frequently methylated in cholangiocarcinoma in Table 1.
Table 1.
Genes frequently methylated in cholangiocarcinoma.
| Gene | Function | Sample | Reference |
|---|---|---|---|
| MLH1 | DNA repair | tissue | [14,15] |
| DCLK1 | stemness | tissue | [16] |
| CDO1 | growth | tissue | [16] |
| ZSCAN18 | unknown | tissue | [16] |
| ZNF331 | growth invasion |
tissue | [16] |
| p14 (ARF) | cell cycle regulator | tissue | [17,18,19] |
| p16 (INK4a, CDKN2A) | cell cycle regulator | tissue QBC939 cell line | [17,18,19,20,21] |
| DAPK | apoptosis | tissue QBC939 cell line | [19,20,22] |
| CCND2 | growth | bile fluid | [23] |
| CDH13 | growth invasion |
bile fluid | [23] |
| GRIN2B | growth | bile fluid | [23] |
| RUNX3 | growth differentiation |
bile fluid | [23] |
| TWIST1 | migration invasion |
bile fluid | [23] |
| EGFR | growth | Mz-ChA-1 cell line | [24] |
| LKB1 | growth migration invasion |
tissue HuH-28 cell line RBE cell line SSP-25 cell line |
[25] |
MLH1 protein is one component of a system of seven DNA mismatch repair (MMR) proteins that work coordinately in sequential steps to initiate the repair of DNA mismatches in humans. Several studies have demonstrated that DNA hypermethylation on the promoter region of the hMLH1 gene is associated with a poor prognosis of patients with cholangiocarcinoma [14,15]. The DCLK1, CDO1, ZSCAN18, and ZNF331 genes have been identified as novel biomarkers of colorectal cancers, and these genes are frequently methylated across gastrointestinal cancers including cholangiocarcinoma [16]. A negative correlation between promoter DNA methylation and gene expression has been observed for the DCLK1, CDO1, ZSCAN18, and ZNF331 genes, suggesting that aberrant DNA methylation of these genes indicates epigenetic similarities among gastrointestinal cancers such as colon, pancreatic, and bile duct cancer. The INK4a-ARF (CDKN2A) locus on chromosome 9p21 encodes two tumor suppressor proteins, p16 (INK4a) and p14 (ARF), whose functions are inactivated in many human cancers. Recent studies have shown that p16 (INK4a) and p14 (ARF) are inactivated by DNA hypermethylation in cholangiocarcinoma, which may result in cell cycle dysregulation [17,18]. Liu et al. demonstrated that the death-associated protein kinase (DAPK) gene is suppressed by promoter hypermethylation in cholangiocarcinoma. Silencing of the DAPK gene by DNA hypermethylation results in resistance to apoptosis and immunological surveillance [22]. In addition, it has been reported that p53 mutation combined with DNA methylation of the DAPK, p14 (ARF), and ASC genes correlates with malignancy and poor prognosis of patients with cholangiocarcinoma [19].
Cancer cells are considered to be heterogeneous with a hierarchy of “stemness” in solid cancer tissues. Stem cells have the ability to self-renew and to generate mature cells of various tissues through differentiation. Cancer stem cells, a subpopulation of cancer cells with distinct stem-like properties, is responsible for tumor initiation, invasive growth, and metastasis formation [26]. As cancer stem cells are resistant to conventional chemotherapies and radiation therapy, it would be desirable to develop a therapeutic strategy specifically targeting cancer stem cells. Sriraksa et al. reported that hypermethylation of multiple CpG sites of genes associated with a stem cell-like phenotype is a common molecular aberration in cholangiocarcinoma [27], indicating that aberrant DNA methylation plays a critical role in “cancer stemness” of cholangiocarcinoma.
Early diagnosis is very important for patients with refractory cancers, but detection of cholangiocarcinoma at an early stage is still challenging because it is difficult to visualize biliary tract tumors by existing imaging modalities [28]. In order to overcome this problem, Shin et al. developed a useful method for the detection of cholangiocarcinoma cells using bile fluid [23]. This method involving DNA methylation assay consisting of a five-gene panel (CCND2, CDH13, GRIN2B, RUNX3 and TWIST1) is able to detect cholangiocarcinoma cells with a sensitivity of 83% and a specificity of 100%. Less invasive examinations such as this method using bile fluid are important for minimizing the burden on the patient. These studies have shown that detection of DNA methylation is a powerful diagnostic strategy for patients with cholangiocarcinoma.
3. DNA Methylation Inhibitors Are Promising Therapeutic Agents against Cholangiocarcinoma
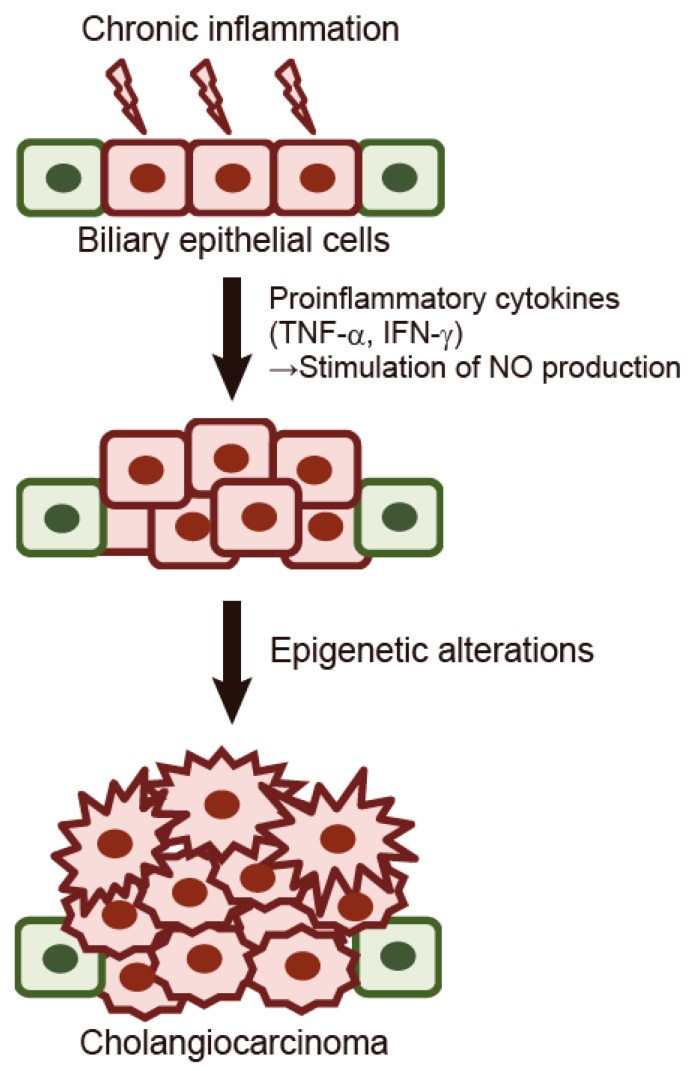
Chronic inflammation in the liver may contribute to malignant transformation of cholangiocytes [29]. It is assumed that persistent inflammation promotes carcinogenesis through DNA damage and tissue repair as well as activation of cytokines and other growth factors [30]. A previous study demonstrated that cholangiocyte-derived cytokines, such as interleukin 6 (IL-6), transforming growth factor-α (TGF-α), and tumor necrosis factor-α (TNF-α) regulate cholangiocyte intracellular signaling and promote carcinogenesis [31]. Spirli et al. demonstrated that proinflammatory cytokines such as TNF-α and interferon (IFN)-γ stimulate the biliary epithelium to generate nitric oxide (NO) via induction of nitric oxide synthase 2 (NOS2) [32]. They also showed that NOS2 expression is significantly increased in the biliary epithelium of patients with primary sclerosing cholangitis (PSC) [32]. Moreover, recent studies have shown that NO directly and indirectly affects numerous epigenetic mechanisms. NO has been shown to alter DNA methylation and histone modifications by altering epigenetic enzymes [33]. Figure 1 shows the molecular mechanism underlying the initiation and progression of cholangiocarcinoma. When chronic inflammation and cholestasis arise due to liver injury, proinflammatory cytokines such as TNF-α and IFN-γ stimulate the biliary epithelium to generate NO. NO alters epigenetic regulation including DNA methylation, which leads to accelerated growth of biliary epithelial cells. Accelerated proliferation of biliary epithelial cells promotes aberrant DNA methylation of tumor suppressor genes, leading to the initiation of cholangiocarcinoma. Wehbe et al. previously reported that IL-6 contributes to the growth of cholangiocarcinoma cells through aberrant DNA methylation on the promoter region of tumor suppressor genes [24]. IL-6 decreased DNA methylation level on the promoter region of the EGFR gene, which leads to the increased expression of the EGFR protein. These findings suggest that persistent cytokine stimulation in biliary epithelial cells could promote the initiation and progression of tumors via epigenetic alterations. Wang et al. showed that suppression of the tumor suppressor liver kinase B1 (LKB1) due to aberrant DNA methylation is associated with enhanced Wnt signaling and malignant characteristics of human cholangiocarcinoma [25]. The expression of the LKB1 gene was suppressed in cholangiocarcinoma tissues relative to adjacent normal tissues and knockdown of LKB1 enhanced the growth, migration, and invasion of tumors, along with the activation of Wnt signaling.
Figure 1.
The molecular mechanism underlying the initiation of cholangiocarcinoma. When chronic inflammation and cholestasis arise due to liver injury, proinflammatory cytokines such as tumor necrosis factor-α (TNF-α) and interferon-γ (IFN-γ) stimulate the biliary epithelium to generate nitric oxide (NO). NO alters epigenetic regulation including DNA methylation, which leads to accelerated growth of biliary epithelial cells. Accelerated proliferation of biliary epithelial cells promotes aberrant DNA methylation of tumor suppressor genes, leading to the initiation of cholangiocarcinoma. Green cells, normal biliary epithelial cells; Red cells, precancerous biliary epithelial cells; Jagged-shaped red cells, cholangiocarcinoma cells.
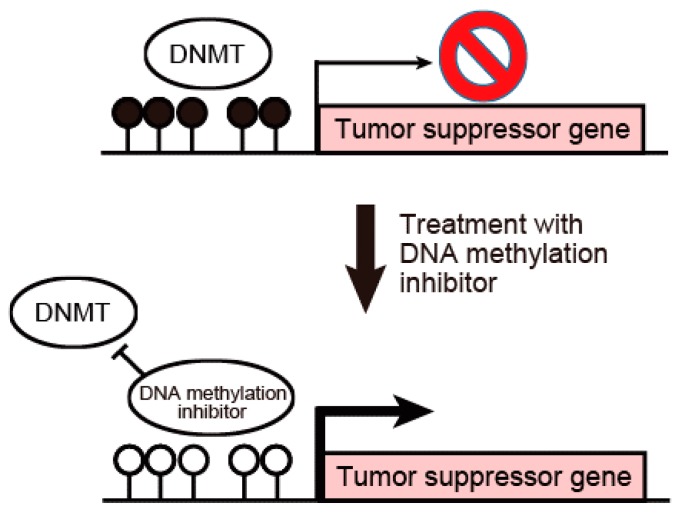
Figure 2 shows a scheme for the activation of tumor suppressor genes by the inhibition of DNA methylation on their promoter regions. In cancer cells, tumor suppressor genes are silenced by DNA hypermethylation on CpG island promoter regions. DNA methylation inhibitors such as 5-Aza-CdR can reactivate epigenetically silenced tumor suppressor genes by the inhibition of DNA methylation on promoter regions. Several studies have evaluated the effect of DNA methylation inhibitors on cholangiocarcinoma. The DNA methylation inhibitor zebularine inhibited human cholangiocarcinoma cells through the alteration of DNA methylation status [34]. Zebularine exerted an anti-tumor effect on cholangiocarcinoma cells through the suppression of DNA methyltransferases. Zebularine altered the DNA methylation status and suppressed the Wnt signaling pathway, resulting in the decreased expression of CTNNB1. Several reports have indicated that tumor suppressor genes that were silenced in cholangiocarcinoma could be reactivated by the DNA methylation inhibitor 5-Aza-CdR [20,35]. Liu et al. reported that treatment of cholangiocarcinoma cells with 5-Aza-CdR inhibited cell growth and induced apoptosis by the reactivation of p53-BAX mitochondrial apoptosis genes [20]. Xiang et al. demonstrated that knockdown of the major DNA methyltransferase DNMT1 restores the expression levels of tumor suppressor genes, which results in the inhibition of the proliferation of cholangiocarcinoma cells [21]. These findings suggest that various tumor suppressor genes are inhibited by DNMT1-induced DNA hypermethylation in their promoter regions, which enhances the proliferation, migration and invasion of cholangiocarcinoma cells. The biological effects of tumor suppressor genes frequently methylated in cholangiocarcinoma are summarized in Table 1. DNA methylation inhibitors such as 5-Aza-CdR and zebularine might have great promise for the treatment of cholangiocarcinoma. However, these DNA methylation inhibitors affect without gene specificity. Lee et al. showed that human N-α-acetyltransferase 10 protein (hNaa10p) contributes to tumorigenesis by facilitating DNMT1-mediated tumor suppressor gene silencing [36]. They confirmed that the oncogenic potential of hNaa10p depends on its interaction with DNMT1. hNaa10p positively regulates DNMT1 enzymatic activity by facilitating its binding to DNA and recruitment to the promoters of tumor suppressor genes such as E-cadherin. These data suggest that DNMT1-induced gene silencing may affect tumor suppressor genes rather than oncogenes in cancer cells. Further studies are necessary to develop DNA methylation inhibitors that specifically affect only the CpG island promoter region of tumor suppressor genes to reduce the side effects of epigenetic therapy.
Figure 2.
Activation of tumor suppressor genes by the inhibition of DNA methylation on their promoter regions. In cancer cells, tumor suppressor genes are silenced by DNA hypermethylation on CpG island promoter regions. DNA methylation inhibitors such as 5-Aza-CdR can reactivate epigenetically silenced tumor suppressor genes by the inhibition of DNA methylation on promoter regions. Solid circle, methylated DNA; clear circle, unmethylated DNA.
4. Suppression of Tumor Suppressor miRNAs by DNA Methylation in Cholangiocarcinoma
The deregulation of miRNAs induces the initiation and progression of cancers by modifying their target tumor suppressor genes or oncogenes [37]. Braconi et al. showed that IL-6 can regulate the activity of DNMT1 by miRNAs in cholangiocarcinoma cells [38]. They verified that miR-148a and miR-152 regulate DNMT1 expression as their targets. They also showed that IL-6 can regulate the activity of DNMT1 and expression of DNA methylation-dependent tumor suppressor genes by modulation of miR-148a and miR-152. These findings provide a link between this inflammation-associated cytokine and oncogenesis in cholangiocarcinoma. In addition, several studies have shown that tumor suppressor miRNAs are regulated by DNA methylation. Meng et al. reported that the expression of DNA methyltransferases was increased by IL-6 overexpression and the tumor suppressor miR-370 was inactivated by DNA methylation in cholangiocarcinoma cells [39]. The oncogene mitogen-activated protein kinase kinase kinase 8 (MAP3K8) was identified as a target of miR-370. 5-Aza-CdR increased the expression of miR-370 in malignant cells, while the expression in non-malignant cells was unchanged. Thus, IL-6 may contribute to tumor growth by the modulation of miR-370 expression in cholangiocarcinoma cells. These findings define a mechanism by which inflammation-associated cytokines can epigenetically modulate gene expression and contribute to the initiation and development of cholangiocarcinoma.
Iwaki et al. also showed that miR-376c was regulated by DNA methylation and associated with tumor suppression by targeting growth factor receptor-bound protein 2 (GRB2) [40]. They found higher methylation levels of CpG sites upstream of the miR-376c gene in cholangiocarcinoma cells relative to normal intrahepatic biliary epithelial cells. The direct target genes and biological functions of miRNAs frequently methylated in cholangiocarcinoma are summarized in Table 2. Since miRNAs regulate several target genes including cancer-related genes, the replacement of tumor suppressor miRNAs might have implications for the treatment of cholangiocarcinoma as well as the activation of tumor suppressor miRNAs by epigenetic therapy using chromatin-modifying agents.
Table 2.
miRNAs frequently methylated in cholangiocarcinoma.
5. Therapeutic Perspectives of DNA Methylation Inhibitors against Cholangiocarcinoma
Other anti-tumor effects of chromatin-modifying drugs have been demonstrated in cancers including colon cancer. One of these other anti-tumor effects is the induction of tumor cell differentiation. Hatano et al. previously showed that DNA demethylation exerts a tumor-suppressive effect on colon cancers by inducing tumor differentiation [41]. They found that the promoter region of the Caudal type homeobox 1 (CDX1) gene was methylated specifically in colon cancer cells. The upregulation of CDX1 increased the expression of genes related to intestinal differentiation. This suggested that the promoters of transcriptional factor genes regulating cell differentiation were silenced by DNA hypermethylation in colon cancer cells to sustain their undifferentiated status.
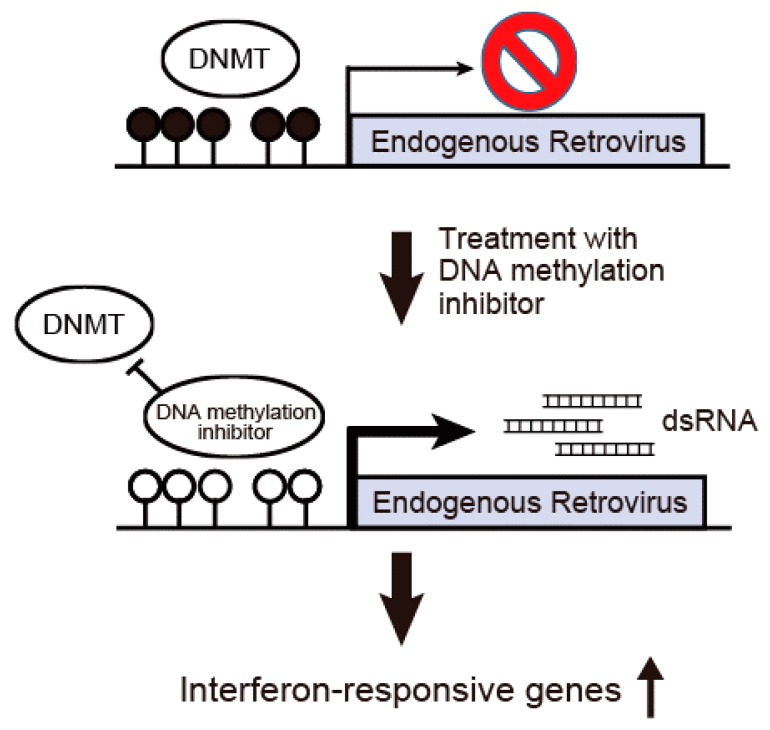
Recent studies have proved that the major effect of DNA methylation inhibitors is to induce interferon-responsive genes by increasing double-stranded RNA (dsRNA) containing endogenous retrovirus (ERV) [42,43]. Different ERV gene families constitute about 8% of the human genome and are considered to be long terminal repeat [44] retrotransposons. Innate immune responses are activated by the expression of ERV-producing nucleic acids or proteins with viral signatures [45]. Roulois et al. recently proposed that 5-Aza-CdR could be used to target colorectal cancer stem cells by inducing viral mimicry [42]. Their data suggested that the induction of dsRNAs is derived at least in part from ERV elements, which activate the MDA5/MAVS RNA recognition pathway. Figure 3 shows a scheme for the activation of an anti-viral immune response induced by the inhibition of DNA methylation. In a normal state, the 5′ long terminal repeat (LTR) sequences of ERVs are heavily methylated and the expression of ERVs is silenced. When DNA methylation at the 5′ LTR sequences is inhibited by DNA methylation inhibitors, the expression of ERVs is induced. Increased expression of dsRNAs derived from ERVs leads to the induction of an anti-viral immune response such as the activation of interferon-responsive genes.
Figure 3.
Activation of an anti-viral immune response induced by the inhibition of DNA methylation. In a normal state, the 5′ LTR sequences of endogenous retrovirus (ERVs) are heavily methylated and the expression of ERVs is silenced. When DNA methylation at the 5′ LTR sequences is inhibited by DNA methylation inhibitors, the expression of ERVs is induced. Increased expression of dsRNAs derived from ERVs leads to the induction of an anti-viral immune response such as the activation of interferon-responsive genes.
We also reported that DNA methylation inhibition suppresses intestinal tumor organoids by inducing anti-viral response [46]. We established tumor organoids derived from the Apcmin/+ mouse, a model of colon cancer, using a new 3D culture system that allows Lgr5-positive stem cells to form cyst-like structures (organoids) [47]. This organoid culture system closely recapitulates the properties of the original tumors, and is useful for drug screening and precision medicine [48]. We demonstrated that 5-Aza-CdR shrinks intestinal tumor organoids derived from Apcmin/+ mice [46]. We revealed that the expression of interferon-responsive genes such as Irf7, Rig1 and Mda5 was increased by DNA methylation inhibition in tumor organoids after 5-Aza-CdR treatment or Dnmt1 knockdown. The expression of murine ERVs was significantly upregulated after the treatment of tumor organoids with 5-Aza-CdR. These findings suggested that treatment with DNA methylation inhibitors to activate an innate immune response would be beneficial for patients with various types of cancers including cholangiocarcinoma. Wrangle et al. showed that DNA methylation inhibitors can upregulate transcripts and protein of PD-L1, a key ligand mediator of immune tolerance [49]. Through analysis of samples from The Cancer Genome Atlas (TCGA), they also demonstrated that a significant proportion of primary non-small cell lung cancers (NSCLCs) have a low expression of DNA methylation inhibitor-induced immune genes such as PD-L1. Their data suggested that a combination of chromatin-modifying agents with immune checkpoint blockade therapies would activate the immune response of the host to cancer cells.
The development of anti-metabolite drugs that are dependent on the cell cycle of cancer cells has revealed a serious problem in that they also act on normal cells and normal stem cells. Therefore, molecular targeting therapeutic agents have been developed to avoid seriously damaging normal cells. One such molecular targeting therapeutic agent is herceptin, approved for the treatment of breast cancer. Although herceptin has improved the relapse-free survival of patients with breast cancer [50], it is still very difficult to eliminate the cancer completely, because cancers have various mutations and different forms of aberrant epigenetic status. In this respect, chromatin-modifying drugs have great promise for cancer therapy because the modification of epigenetic status alone can inhibit various tumor characteristics such as proliferation, migration, invasion, and dedifferentiation. It has been demonstrated that reprofiling of food and drug administration (FDA)-approved drugs in combination with chromatin-modifying drugs can be implemented into clinical trials for colon cancer [51].
In conclusion, aberrant DNA methylation of tumor suppressor genes and miRNAs could be a powerful biomarker for the diagnosis and treatment of cholangiocarcinoma. Epigenetic therapy with DNA methylation inhibitors hold considerable promise for the treatment of cholangiocarcinoma through the reactivation of tumor suppressor genes and miRNAs as well as the induction of an anti-viral immune response.
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Razumilava N., Gores G.J. Cholangiocarcinoma. Lancet. 2014;383:2168–2179. doi: 10.1016/S0140-6736(13)61903-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Blechacz B., Komuta M., Roskams T., Gores G.J. Clinical diagnosis and staging of cholangiocarcinoma. Nat. Rev. Gastroenterol. Hepatol. 2011;8:512–522. doi: 10.1038/nrgastro.2011.131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kelly T.K., de Carvalho D.D., Jones P.A. Epigenetic modifications as therapeutic targets. Nat. Biotechnol. 2010;28:1069–1078. doi: 10.1038/nbt.1678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jones P.A., Baylin S.B. The epigenomics of cancer. Cell. 2007;128:683–692. doi: 10.1016/j.cell.2007.01.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gal-Yam E.N., Saito Y., Egger G., Jones P.A. Cancer epigenetics: Modifications, screening, and therapy. Annu. Rev. Med. 2008;59:267–280. doi: 10.1146/annurev.med.59.061606.095816. [DOI] [PubMed] [Google Scholar]
- 6.Baylin S.B., Jones P.A. A decade of exploring the cancer epigenome-biological and translational implications. Nat. Rev. Cancer. 2011;11:726–734. doi: 10.1038/nrc3130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Saito Y., Hibino S., Saito H. Alterations of epigenetics and microRNA in hepatocellular carcinoma. Hepatol. Res. 2014;44:31–42. doi: 10.1111/hepr.12147. [DOI] [PubMed] [Google Scholar]
- 8.Saito Y., Liang G., Egger G., Friedman J.M., Chuang J.C., Coetzee G.A., Jones P.A. Specific activation of microRNA-127 with downregulation of the proto-oncogene BCL6 by chromatin-modifying drugs in human cancer cells. Cancer Cell. 2006;9:435–443. doi: 10.1016/j.ccr.2006.04.020. [DOI] [PubMed] [Google Scholar]
- 9.Saito Y., Jones P.A. Epigenetic activation of tumor suppressor microRNAs in human cancer cells. Cell Cycle. 2006;5:2220–2222. doi: 10.4161/cc.5.19.3340. [DOI] [PubMed] [Google Scholar]
- 10.Takaki Y., Saito Y., Takasugi A., Toshimitsu K., Yamada S., Muramatsu T., Kimura M., Sugiyama K., Suzuki H., Arai E., et al. Silencing of microRNA-122 is an early event during hepatocarcinogenesis from non-alcoholic steatohepatitis. Cancer Sci. 2014;105:1254–1260. doi: 10.1111/cas.12498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Saito Y., Saito H., Liang G., Friedman J.M. Epigenetic alterations and microRNA misexpression in cancer and autoimmune diseases: A critical review. Clin. Rev. Allergy Immunol. 2014;47:128–135. doi: 10.1007/s12016-013-8401-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wakabayashi K., Saito H., Kaneko F., Nakamoto N., Tada S., Hibi T. Gene expression associated with the decrease in malignant phenotype of human liver cancer cells following stimulation with a histone deacetylase inhibitor. Int. J. Oncol. 2005;26:233–239. doi: 10.3892/ijo.26.1.233. [DOI] [PubMed] [Google Scholar]
- 13.Hibino S., Saito Y., Muramatsu T., Otani A., Kasai Y., Kimura M., Saito H. Inhibitors of enhancer of zeste homolog 2 (EZH2) activate tumor-suppressor microRNAs in human cancer cells. Oncogenesis. 2014;3:e104. doi: 10.1038/oncsis.2014.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Limpaiboon T., Khaenam P., Chinnasri P., Soonklang M., Jearanaikoon P., Sripa B., Pairojkul C., Bhudhisawasdi V. Promoter hypermethylation is a major event of hMLH1 gene inactivation in liver fluke related cholangiocarcinoma. Cancer Lett. 2005;217:213–219. doi: 10.1016/j.canlet.2004.06.020. [DOI] [PubMed] [Google Scholar]
- 15.Abraham S.C., Lee J.H., Boitnott J.K., Argani P., Furth E.E., Wu T.T. Microsatellite instability in intraductal papillary neoplasms of the biliary tract. Mod. Pathol. 2002;15:1309–1317. doi: 10.1097/01.MP.0000038461.80167.34. [DOI] [PubMed] [Google Scholar]
- 16.Vedeld H.M., Andresen K., Eilertsen I.A., Nesbakken A., Seruca R., Gladhaug I.P., Thiis-Evensen E., Rognum T.O., Boberg K.M., Lind G.E. The novel colorectal cancer biomarkers CDO1, ZSCAN18 and ZNF331 are frequently methylated across gastrointestinal cancers. Int. J. Cancer. 2015;136:844–853. doi: 10.1002/ijc.29039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Taniai M., Higuchi H., Burgart L.J., Gores G.J. p16INK4a promoter mutations are frequent in primary sclerosing cholangitis (PSC) and PSC-associated cholangiocarcinoma. Gastroenterology. 2002;123:1090–1098. doi: 10.1053/gast.2002.36021. [DOI] [PubMed] [Google Scholar]
- 18.Tannapfel A., Busse C., Geissler F., Witzigmann H., Hauss J., Wittekind C. INK4a-ARF alterations in liver cell adenoma. Gut. 2002;51:253–258. doi: 10.1136/gut.51.2.253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Xiaofang L., Kun T., Shaoping Y., Zaiqiu W., Hailong S. Correlation between promoter methylation of p14(ARF), TMS1/ASC, and DAPK, and p53 mutation with prognosis in cholangiocarcinoma. World J. Surg. Oncol. 2012;10:5. doi: 10.1186/1477-7819-10-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Liu X.F., Jiang H., Zhang C.S., Yu S.P., Wang Z.Q., Su H.L. Targeted drug regulation on methylation of p53-BAX mitochondrial apoptosis pathway affects the growth of cholangiocarcinoma cells. J. Int. Med. Res. 2012;40:67–75. doi: 10.1177/147323001204000107. [DOI] [PubMed] [Google Scholar]
- 21.Xiang J., Luo F., Chen Y., Zhu F., Wang J. si-DNMT1 restore tumor suppressor genes expression through the reversal of DNA hypermethylation in cholangiocarcinoma. Clin. Res. Hepatol. Gastroenterol. 2014;38:181–189. doi: 10.1016/j.clinre.2013.11.004. [DOI] [PubMed] [Google Scholar]
- 22.Liu X.F., Kong F.M., Xu Z., Yu S.P., Sun F.B., Zhang C.S., Huang Q.X., Zhou X.T., Song Z.W. Promoter hypermethylation of death-associated protein kinase gene in cholangiocarcinoma. Hepatobiliary Pancreat. Dis. Int. 2007;6:407–411. [PubMed] [Google Scholar]
- 23.Shin S.H., Lee K., Kim B.H., Cho N.Y., Jang J.Y., Kim Y.T., Kim D., Jang J.J., Kang G.H. Bile-based detection of extrahepatic cholangiocarcinoma with quantitative DNA methylation markers and its high sensitivity. J. Mol. Diagn. 2012;14:256–263. doi: 10.1016/j.jmoldx.2012.01.014. [DOI] [PubMed] [Google Scholar]
- 24.Wehbe H., Henson R., Meng F., Mize-Berge J., Patel T. Interleukin-6 contributes to growth in cholangiocarcinoma cells by aberrant promoter methylation and gene expression. Cancer Res. 2006;66:10517–10524. doi: 10.1158/0008-5472.CAN-06-2130. [DOI] [PubMed] [Google Scholar]
- 25.Wang J., Zhang K., Wu X., Liu X., Li B., Zhu Y., Yu Y., Cheng Q., Hu Z., Guo C., et al. Underexpression of LKB1 tumor suppressor is associated with enhanced Wnt signaling and malignant characteristics of human intrahepatic cholangiocarcinoma. Oncotarget. 2015;6:18905–18920. doi: 10.18632/oncotarget.4305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kreso A., Dick J.E. Evolution of the cancer stem cell model. Cell Stem Cell. 2014;14:275–291. doi: 10.1016/j.stem.2014.02.006. [DOI] [PubMed] [Google Scholar]
- 27.Sriraksa R., Zeller C., Dai W., Siddiq A., Walley A.J., Limpaiboon T., Brown R. Aberrant DNA methylation at genes associated with a stem cell-like phenotype in cholangiocarcinoma tumors. Cancer Prev. Res. 2013;6:1348–1355. doi: 10.1158/1940-6207.CAPR-13-0104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ferrari Junior A.P., Lichtenstein D.R., Slivka A., Chang C., Carr-Locke D.L. Brush cytology during ERCP for the diagnosis of biliary and pancreatic malignancies. Gastrointest. Endosc. 1994;40:140–145. doi: 10.1016/S0016-5107(94)70155-5. [DOI] [PubMed] [Google Scholar]
- 29.Lazaridis K.N., Gores G.J. Cholangiocarcinoma. Gastroenterology. 2005;128:1655–1667. doi: 10.1053/j.gastro.2005.03.040. [DOI] [PubMed] [Google Scholar]
- 30.Schottenfeld D., Beebe-Dimmer J. Chronic inflammation: A common and important factor in the pathogenesis of neoplasia. CA Cancer J. Clin. 2006;56:69–83. doi: 10.3322/canjclin.56.2.69. [DOI] [PubMed] [Google Scholar]
- 31.Berthiaume E.P., Wands J. The molecular pathogenesis of cholangiocarcinoma. Semin. Liver Dis. 2004;24:127–137. doi: 10.1055/s-2004-828890. [DOI] [PubMed] [Google Scholar]
- 32.Spirli C., Fabris L., Duner E., Fiorotto R., Ballardini G., Roskams T., Larusso N.F., Sonzogni A., Okolicsanyi L., Strazzabosco M. Cytokine-stimulated nitric oxide production inhibits adenylyl cyclase and cAMP-dependent secretion in cholangiocytes. Gastroenterology. 2003;124:737–753. doi: 10.1053/gast.2003.50100. [DOI] [PubMed] [Google Scholar]
- 33.Socco S., Bovee R.C., Palczewski M.B., Hickok J.R., Thomas D.D. Epigenetics: The third pillar of nitric oxide signaling. Pharmacol. Res. 2017;121:52–58. doi: 10.1016/j.phrs.2017.04.011. [DOI] [PubMed] [Google Scholar]
- 34.Nakamura K., Nakabayashi K., Htet Aung K., Aizawa K., Hori N., Yamauchi J., Hata K., Tanoue A. DNA methyltransferase inhibitor zebularine induces human cholangiocarcinoma cell death through alteration of DNA methylation status. PLoS ONE. 2015;10:e0120545. doi: 10.1371/journal.pone.0120545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Uhm K.O., Lee E.S., Lee Y.M., Kim H.S., Park Y.N., Park S.H. Aberrant promoter CpG islands methylation of tumor suppressor genes in cholangiocarcinoma. Oncol. Res. 2008;17:151–157. doi: 10.3727/096504008785114110. [DOI] [PubMed] [Google Scholar]
- 36.Lee C.F., Ou D.S., Lee S.B., Chang L.H., Lin R.K., Li Y.S., Upadhyay A.K., Cheng X., Wang Y.C., Hsu H.S., et al. hNaa10p contributes to tumorigenesis by facilitating DNMT1-mediated tumor suppressor gene silencing. J. Clin. Investig. 2010;120:2920–2930. doi: 10.1172/JCI42275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Calin G.A., Croce C.M. MicroRNA signatures in human cancers. Nat. Rev. Cancer. 2006;6:857–866. doi: 10.1038/nrc1997. [DOI] [PubMed] [Google Scholar]
- 38.Braconi C., Huang N., Patel T. MicroRNA-dependent regulation of DNA methyltransferase-1 and tumor suppressor gene expression by interleukin-6 in human malignant cholangiocytes. Hepatology. 2010;51:881–890. doi: 10.1002/hep.23381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Meng F., Wehbe-Janek H., Henson R., Smith H., Patel T. Epigenetic regulation of microRNA-370 by interleukin-6 in malignant human cholangiocytes. Oncogene. 2008;27:378–386. doi: 10.1038/sj.onc.1210648. [DOI] [PubMed] [Google Scholar]
- 40.Iwaki J., Kikuchi K., Mizuguchi Y., Kawahigashi Y., Yoshida H., Uchida E., Takizawa T. MiR-376c down-regulation accelerates EGF-dependent migration by targeting GRB2 in the HuCCT1 human intrahepatic cholangiocarcinoma cell line. PLoS ONE. 2013;8:e69496. doi: 10.1371/journal.pone.0069496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hatano Y., Semi K., Hashimoto K., Lee M.S., Hirata A., Tomita H., Kuno T., Takamatsu M., Aoki K., Taketo M.M., et al. Reducing DNA methylation suppresses colon carcinogenesis by inducing tumor cell differentiation. Carcinogenesis. 2015;36:719–729. doi: 10.1093/carcin/bgv060. [DOI] [PubMed] [Google Scholar]
- 42.Roulois D., Loo Yau H., Singhania R., Wang Y., Danesh A., Shen S.Y., Han H., Liang G., Jones P.A., Pugh T.J., et al. DNA-Demethylating Agents Target Colorectal Cancer Cells by Inducing Viral Mimicry by Endogenous Transcripts. Cell. 2015;162:961–973. doi: 10.1016/j.cell.2015.07.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Chiappinelli K.B., Strissel P.L., Desrichard A., Li H., Henke C., Akman B., Hein A., Rote N.S., Cope L.M., Snyder A., Makarov V., et al. Inhibiting DNA Methylation Causes an Interferon Response in Cancer via dsRNA Including Endogenous Retroviruses. Cell. 2015;162:974–986. doi: 10.1016/j.cell.2015.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Abiru S., Migita K., Maeda Y., Daikoku M., Ito M., Ohata K., Nagaoka S., Matsumoto T., Takii Y., Kusumoto K., et al. Serum cytokine and soluble cytokine receptor levels in patients with non-alcoholic steatohepatitis. Liver Int. 2006;26:39–45. doi: 10.1111/j.1478-3231.2005.01191.x. [DOI] [PubMed] [Google Scholar]
- 45.Hurst T.P., Magiorkinis G. Activation of the innate immune response by endogenous retroviruses. J. Gen. Virol. 2015;96:1207–1218. doi: 10.1099/jgv.0.000017. [DOI] [PubMed] [Google Scholar]
- 46.Saito Y., Nakaoka T., Sakai K., Muramatsu T., Toshimitsu K., Kimura M., Kanai T., Sato T., Saito H. Inhibition of DNA Methylation Suppresses Intestinal Tumor Organoids by Inducing an Anti-Viral Response. Sci. Rep. 2016;6:25311. doi: 10.1038/srep25311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Sato T., Vries R.G., Snippert H.J., van de Wetering M., Barker N., Stange D.E., van Es J.H., Abo A., Kujala P., Peters P.J., et al. Single Lgr5 stem cells build crypt-villus structures in vitro without a mesenchymal niche. Nature. 2009;459:262–265. doi: 10.1038/nature07935. [DOI] [PubMed] [Google Scholar]
- 48.Van de Wetering M., Francies H.E., Francis J.M., Bounova G., Iorio F., Pronk A., van Houdt W., van Gorp J., Taylor-Weiner A., Kester L., et al. Prospective derivation of a living organoid biobank of colorectal cancer patients. Cell. 2015;161:933–945. doi: 10.1016/j.cell.2015.03.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Wrangle J., Wang W., Koch A., Easwaran H., Mohammad H.P., Vendetti F., Vancriekinge W., Demeyer T., Du Z., Parsana P., et al. Alterations of immune response of Non-Small Cell Lung Cancer with Azacytidine. Oncotarget. 2013;4:2067–2079. doi: 10.18632/oncotarget.1542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Vici P., Pizzuti L., Natoli C., Moscetti L., Mentuccia L., Vaccaro A., Sergi D., Di Lauro L., Trenta P., Seminara P., et al. Outcomes of HER2-positive early breast cancer patients in the pre-trastuzumab and trastuzumab eras: A real-world multicenter observational analysis. The RETROHER study. Breast Cancer Res. Treat. 2014;147:599–607. doi: 10.1007/s10549-014-3133-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Raynal N.J., Da Costa E.M., Lee J.T., Gharibyan V., Ahmed S., Zhang H., Sato T., Malouf G.G., Issa J.J. Repositioning FDA-Approved Drugs in Combination with Epigenetic Drugs to Reprogram Colon Cancer Epigenome. Mol. Cancer Ther. 2016 doi: 10.1158/1535-7163.MCT-16-0588. [DOI] [PMC free article] [PubMed] [Google Scholar]