FIGURE 3. Myocardial Inflammation and Impaired Myocardial Perfusion Reserve by CMR.
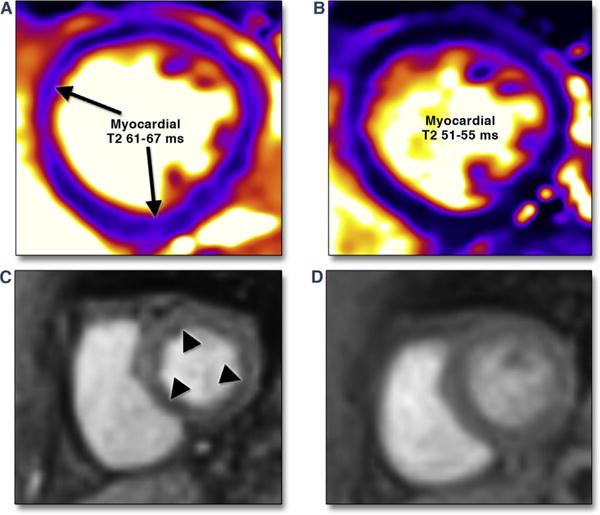
A 37-year-old female was admitted with visual changes. Serologic testing and neuroimaging yielded a diagnosis of lupus cerebritis. Significant resting tachycardia (heart rate 120 to 130 beats/min) raised concern of lupus myocarditis, confirmed by CMR examination that showed significantly elevated myocardial T2 values (A). Immunomodulatory therapy was initiated, with both improvement visual symptoms and normalization of heart rate. She returned to the hospital approximately 5 months later with chest pain and lack of inflammatory markers with a resting heart rate of 75 beats/min. ECG and serial troponin-I measurements were negative for myocardial injury. CMR showed normalized T2 values (B); vasodilator stress adenosine infusion produced severe chest pain, and concomitant first-pass perfusion imaging showed diffuse subendocardial hypoperfusion (C). Minimal residual chest pain was present upon termination of adenosine, with near-complete normalization of perfusion (D). Chest pain attributed to impaired myocardial perfusion reserve has reduced with angiotensin converting enzyme inhibitor therapy.
