Figure 1.
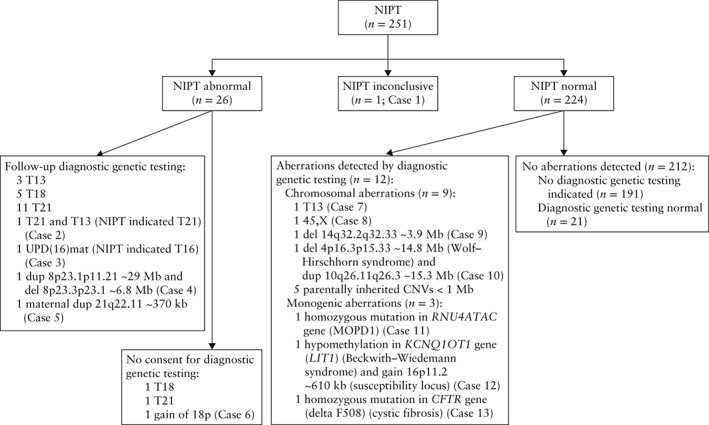
Flowchart of results of non‐invasive prenatal testing (NIPT) in 251 pregnancies with ultrasound anomaly. NIPT was by massively parallel sequencing of cell‐free DNA in maternal plasma. Diagnostic genetic testing was by quantitative fluorescent polymerase chain reaction, karyotyping, microarray analysis or targeted DNA testing of fetal or maternal tissue. Case 1: genetic testing indicated by polyhydramnios, NIPT did not meet quality criteria, however, visual inspection of plots repeatedly showed suspect chromosome 22 profile. Mother had mild intellectual disability, shortened palate, mild hearing impairment, common variable immunodeficiency. Maternal array was 22q11.21(18,970,562‐21,465,660)×1, ∼2.5 megabases (Mb). No further genetic testing. Resulted in live birth with no congenital anomaly. Postnatal microarray of newborn revealed 22q11.21(18,648,867‐21,798,908)×1 mat, ∼2.8 Mb. Case 2: multiple pregnancy, genetic testing indicated by multiple structural anomalies (intrauterine growth restriction, holoprosencephaly, omphalocele, megacystis with bilateral hydro‐nephrosis) in one fetus. No structural anomaly was observed in other fetus. NIPT showed T21. Follow‐up ultrasound at 17 weeks' gestation revealed atrioventricular septal defect and absent nasal bone in fetus without previously detected anomalies. Amniocentesis and genetic testing showed 47,XY + 21 and 47,XY + 13. Pregnancy was terminated. Cases 3–13 summarized in Tables 2 and 3. CNV, copy number variant; del, deletion; dup, duplication; kb, kilobases; MOPD1, microcephaly osteodysplastic primordial dwarfism Type I; T13, trisomy 13 (Patau syndrome); T16, trisomy 16; T18, trisomy 18 (Edwards syndrome); T21, trisomy 21 (Down syndrome); UPD(16)mat, maternal uniparental disomy of chromosome 16.
