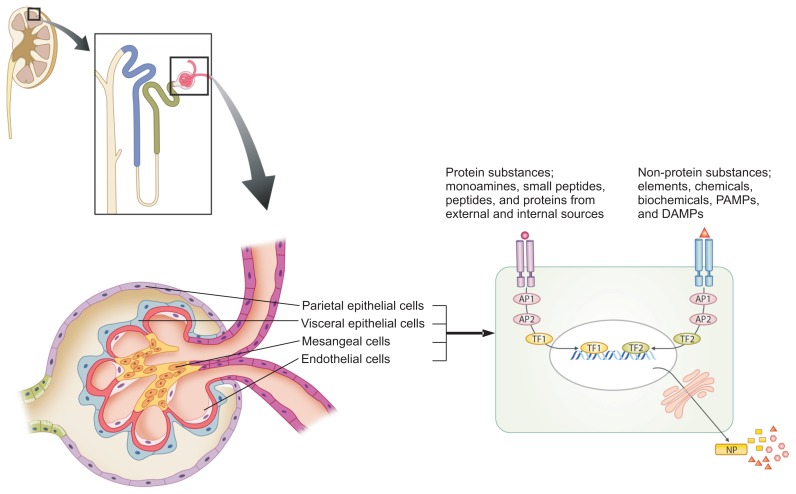
Figure 1. Immunopathogenesis of renal diseases.
All biological phenomena in organisms are controlled by a network termed the protein-homeostasis-system (PHS), and the immune system is one aspect of the PHS of the host. Each renal cell has its own receptors for intercellular communication. There are toxic or etiologic substances that have an affinity to renal cells and induce renal cell injury in every renal disease. These substances have various sizes and biochemical characteristics, and they can largely be classified as protein substances and non-protein substances. The protein substances include monoamines, neuropeptides, peptides (12–30 amino acids) and proteins, and each of them originates from external sources such as pathogens and natural toxins or from internal sources such as injured host cells or activated immune cells including heat shock proteins and proinfliammatory cytokines. The non-protein substances include elements (pure oxygen, carbon monoxide, and others), chemicals and biochemicals (drugs, vitamins, fatty acids, and others), PAMPs (lipopolysaccharides, pathogen DNAs and RNAs, and others), and DAMPs from the host cells. Each immune cell and immune protein may recognize and act on these substances, based on the size and biochemical characteristics of the substances; innate immune system cells control non-protein substances, and adaptive immune cells control protein substances including pathogenic proteins and pathogenic peptides. The severity, chronicity or prognosis of renal diseases depends on the amount of etiologic substances with corresponding immune reactions, the duration of the appearance of specific immune cells, or the existence of specific immune cell repertoires that control the substances.
AP, adaptor protein; DAMPs, damage-associated molecular pattern; NP, new protein; PAMPs, pathogen-associated molecular patterns; TF, transcriptional factor.