Abstract
Objective
The aim of this retrospective study was to identify the significant risk factors that contribute towards postoperative infection in patients recovering from orthognathic surgery.
Methods
Retrospective records of 522 patients who underwent orthognathic surgery over 9 year period were evaluated for postoperative infection within 3 months of surgery and after 3 months of surgery. The variables of interest included age, gender, habits like smoking and alcohol consumption and incidence of postoperative infection.
Results
The overall infection rate was 4.60%. Patients who underwent bilateral sagittal split osteotomy to advance the mandible had an infection rate of 10.4%. Statistically significant predictor variables (P < 0.05) included patients who had the smoking habit, and those that received bone grafts in both the time periods.
Conclusion
In conclusion, the occurrence of infection after orthognathic surgery is influenced by multiple factors, among which are the type of osteotomy, smoking habit and bone grafting procedures.
Keywords: Orthognathic surgery, Risk factors, Infection, Plate removal, Antibiotics
Introduction
It is highly desirable in any form of surgery, that the period of postoperative healing be as short and uneventful as possible. A myriad of factors influence this and it is imperative to ensure a smooth and problem free healing period. One of the chief postoperative complications is postoperative infection.
In the field of orthognathic surgery, the risk of infection to the surgical site, especially around the osteosynthesis material is of great concern to the clinician. Various studies report varying rates of postoperative infection in patients treated for dentofacial deformity using semi rigid fixation, and multiple risk factors have been postulated towards contributing to the overall rate of postoperative infection in such patients [1, 2].
The aim of this retrospective study was to identify the significant risk factors that contribute towards postoperative infection in patients recovering from orthognathic surgery.
Methods
This retrospective study was approved by the institutional scientific review board. The clinical records of patients who underwent single piece osteotomy procedure (Lefort 1, Bilateral Sagittal Split Osteotomy, Anterior Maxillary Osteotomy, Lower Anterior Segmental Osteotomy or genioplasty) over a 9 year period from June 2006 to May 2015 were obtained and reviewed retrospectively. Patients were excluded if they underwent bi-maxillary surgery, had single dose antibiotics, multiple osteotomy cuts, cleft lip and palate patients or comorbid medical problems.
A total of 522 patient records were obtained, out of which 310 were male and 212 were female. Mean age of the patients was 24.21 years (Range between 17 and 38 years). The variables of interest included age, gender, habits like smoking and alcohol consumption, the usage of bone grafts, type of osteotomy, and incidence of postoperative infection. No postoperative drains were utilized for any of the included patients. All patients received a standard postoperative antibiotic regimen for 5 days (Ampicillin and Metronidazole). The incidence of infection for the sample of patients was divided based on occurrence into 2 time periods: within 3 months after surgery (T1) and more than 3 months after surgery (T2). Method of fixation for all patients was with stainless steel miniplates and screws. In our sample, only autogenous bone grafts were used.
Postoperative infection was defined as either mucopurulent drainage from the surgical site or signs and symptoms of infection, which includes tenderness, persistent swelling or redness. Wound dehiscence, granulation tissue formation at site of plating, or the presence of a draining fistula with pus was also considered as an infectious reaction. Surgical sites which exhibited with doubtful diagnosis was usually opened over the surgical incision and sent for microbiological culture and antibiotic sensitivity. Culture negative patients in this regard were grouped as absence of infection.
The associations between the outcome and predictor variables were evaluated using Chi square test. Logistic regression analysis was fitted for the outcome and the results were presented along with Odds ratio. Level of significance was set at P < 0.05. Statistical calculations were done using Statistical Package for the Social Sciences 17 (SPSS 17.0).
Results
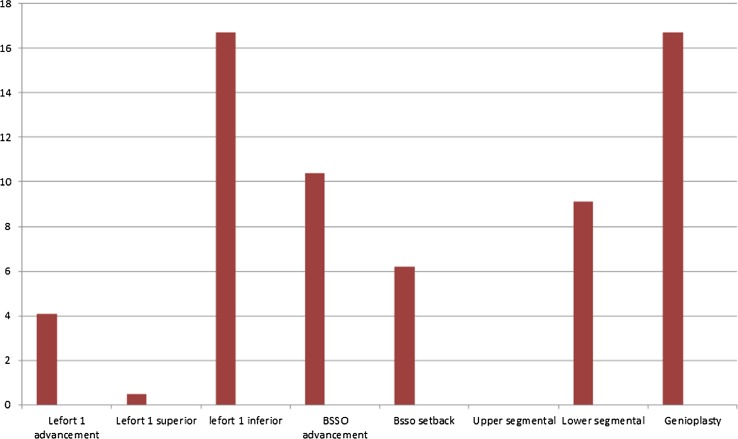
Out of 522 patients, patients who received mandibular advancement via bilateral sagittal split osteotomy reported with an infection rate of 10.4% out of 67 patients. Although genioplasty and inferior repositioning of maxilla by Lefort 1 osteotomy recorded a higher percentage of infection (16.7%), the sample size for those two groups was only 6 and 12 respectively. Table 1 and Fig. 1 provide a summary of infection percentages with regard to osteotomy type.
Table 1.
Infection percentages with regard to type of osteotomy
| Osteotomy type (N = 522) | Total number | No. of infected patients |
|---|---|---|
| Lefort 1 advancement | 121 | 5 |
| Lefort 1 superior repositioning | 189 | 1 |
| Lefort 1 inferior repositioning | 12 | 2 |
| BSSO advancement | 67 | 7 |
| BSSO setback | 97 | 6 |
| Upper anterior segmental | 8 | 0 |
| Lower anterior segmental | 22 | 2 |
| Genioplasty | 6 | 1 |
Fig. 1.
Infection percentages among different osteotomy types
Out of the various predictor variables of interest, patients who smoked showed a higher percentage of infection. In our case series, 62 patients were smokers. In the first time period, 4.8% of these patients reported with postoperative infection. 16.1% of them reported with postoperative infection in the second time period (Table 2).
Table 2.
Association between infection and predictor variables
| Number of patients | Presence of infection | ||||
|---|---|---|---|---|---|
| T1 | % | T2 | % | ||
| Gender | |||||
| Male | 310 | 4 | 1.3 | 13 | 4.2 |
| Female | 212 | 4 | 1.9 | 3 | 1.4 |
| P value | 0.169 | ||||
| Smoking habit | |||||
| No | 460 | 5 | 1.1 | 6 | 1.3 |
| Yes | 62 | 3 | 4.8 | 10 | 16.1 |
| P value | <0.001 | ||||
| Alcohol | |||||
| No | 479 | 6 | 1.3 | 12 | 2.5 |
| Yes | 43 | 2 | 4.7 | 4 | 9.3 |
| P value | 0.011 | ||||
| Bone graft | |||||
| No | 493 | 6 | 1.2 | 11 | 2.2 |
| Yes | 29 | 2 | 6.9 | 5 | 17.2 |
| P value | 0.001 | ||||
On further analysis of the results, bone graft placement also showed a statistically significant result with regard to infection. Out of 19 patients who underwent mandibular advancement via bilateral sagittal split along with bone grafting procedure, 3 of the patients reported with postoperative infection. Out of 6 patients who underwent inferior repositioning of the maxilla via Lefort 1 osteotomy, 2 patients reported with postoperative infection. All in all, 7 patients out of 29 who underwent bone grafting procedures had postoperative infection. Table 3 provides a summary of results with relation to bone grafting and osteotomy type.
Table 3.
Cross tabulation of bone grafts and incidence of infection with regard to osteotomy type
| Bone grafts | Osteotomy types | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Lefort 1 Advancement | Lefort 1 superior | Lefort 1 inferior | BSSO advancement | BSSO setback | Upper segmental | Lower segmental | Genioplasty | Total | |||
| No | Infection | No | 114 | 188 | 6 | 44 | 91 | 8 | 20 | 5 | 476 |
| T2 | 1 | 0 | 0 | 4 | 5 | 0 | 1 | 0 | 11 | ||
| T1 | 2 | 1 | 0 | 0 | 1 | 0 | 1 | 1 | 6 | ||
| Total | 117 | 189 | 6 | 48 | 97 | 8 | 22 | 6 | 493 | ||
| Yes | Infection | No | 2 | 4 | 16 | 22 | |||||
| T2 | 1 | 2 | 2 | 5 | |||||||
| T1 | 1 | 0 | 1 | 2 | |||||||
| Total | 4 | 6 | 19 | 29 | |||||||
On using a logistic regression model taking into consideration the two different time periods, a statistically significant analysis was obtained for smoking and bone grafting in both time periods (Table 4).
Table 4.
Adjusted Odds ratio with 95% confidence interval for occurrence of postoperative infection utilising a multinomial logistic regression
| Time interval | Predictor | Odds ratio | 95% CI | P value |
|---|---|---|---|---|
| T1 | Age | 1.123 | 0.996–1.265 | 0.057 |
| Male gender | 0.267 | 0.041–1.735 | 0.167 | |
| Smoking | 9.358 | 1.14–76.808 | 0.037 | |
| Alcohol | 1.197 | 0.111–12.925 | 0.882 | |
| Bone graft | 9.166 | 1.512–55.569 | 0.016 | |
| T2 | Age | 1.105 | 0.989–1.235 | 0.077 |
| Male gender | 1.581 | 0.293–8.543 | 0.594 | |
| Smoking | 21.732 | 4.358–108.365 | <0.001 | |
| Alcohol | 0.277 | 0.057–1.35 | 0.113 | |
| Bone grafts | 17.814 | 3.578–88.706 | <0.001 |
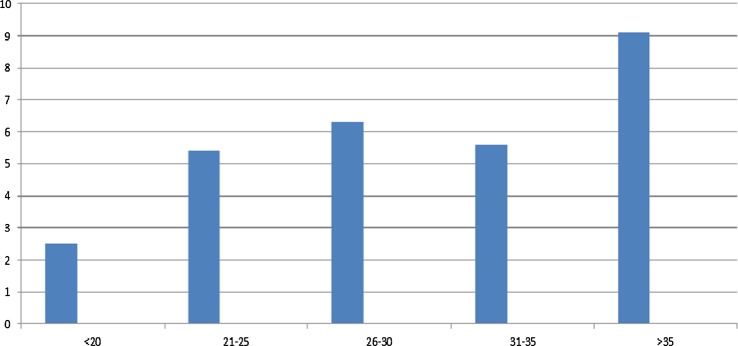
Figure 2 depicts the incidence of infection with respect to the various age groups of patients in this series. Patients beyond the age of 35 had an increased percentage of infection. However the predictor variable age was not statistically significant in our sample of patients.
Fig. 2.
Infection percentages among different age groups
Discussion
In this study we attempted to evaluate the various risk factors that contribute to the occurrence of postoperative infections in patients who undergo orthognathic surgery. The evaluation period was divided into two: early (T1) and late (T2). This was done to identify risk factors for both periods. Moreover, the majority of patients that require removal of osteosynthesis plates and screws usually report in the later period. As such, different factors might lead to postoperative infection between the two periods. Eight patients (1.5%) had infection within the 3 months of follow up, and 16 patients (3.1%) had infection during the second evaluation period. No patient had infection in both time periods.
The overall rate of infection over the study period was 4.60%, which is lower than the infection rates reported in studies by Kuhlefelt et al. [3] and Spaey et al. [4]; which stand at 9.1 and 6.8% respectively. There was no use of intraoral drains, which might lead to contamination of the surgical site during their removal [4]. Also in our series we utilised stainless steel instead of titanium miniplates which may have contributed to the overall infection rate [5]. Even the design of the said miniplates might play a role as a risk factor contributing to infection [6].
In our series, patients who underwent an osteotomy that resulted in a wide gap between bone segments, like maxillary or mandibular advancements or inferior repositioning of the maxilla, had an increased incidence of postoperative infection. This can be attributed to the lodgment of foreign bodies like food particles in between the bony segments; which in turn promotes bacterial growth. The increased gap between the bony osteotomy segments also results in increased healing time. This anatomical dead space because of lack of bony contacts between such segments could lead to an increase in infection rates [7]. Also observed was a higher degree of postoperative infection in mandibular procedures, which could be due to the relatively lower blood supply in the mandible compared to the maxilla [8], as well as the natural gravity pull which results in salivary stasis in the mandible instead of the maxilla [9].
Smoking was identified as an important risk factor that contributes significantly to the healing of postoperative wound. The cocktail of toxins contained in tobacco smoke cumulatively result in decreased tissue oxygenation and may also have direct effects on the healing process at a cellular level [10]. In this study, tobacco smoking in patients exhibited a strong correlation with postoperative infection. Other studies show that smoking may result in delays in healing of bony fracture sites which could contribute to surgical site infection [11]. Healing of other oral surgical procedures are also adversely affected by smoking [12, 13]. In the first postoperative time period, smoking might have an adverse effect on the initial bony healing responses at the osteotomy sites, leading to an infection over the site of surgery. In the second postoperative period, the adverse effects on smoking, especially when there is hardware complications like screw loosening or biomaterial incompatibility might predispose the patient to developing an infection over the site of plating.
Although the study did not report on the oral hygiene status, it is to the investigator’s experience that poor maintenance of oral hygiene also contributes to the incidence of postoperative infection. As our records make no mention of this variable, the investigators were unable to shed more light on the subject. Also we observed an increase in infection rate in patients that were placed under intermaxillary fixation which may be due to the difficulty in maintaining oral hygiene.
In this series of patients 29 of them underwent bone grafting procedures, all of which were autogenous grafts harvested from the iliac crest. 5 patients reported with postoperative infection during T1 and 2 during T2. However, the small sample size might not give an accurate picture of the rate of infection in patients who receive bone grafting procedures for orthognathic surgery. In this institution, hardware removal was advised only after a minimum of 3 months. One of the main reasons for removal of plates and screws in this sample if a patients was infection [1, 14, 15]. Manor et al. [16] analyzed the risk factors contributing to symptomatic plate removal and concluded that age is a primary risk factor, with gender and material being secondary. We also observed a trend of increased frequency of patients requiring plate removal as the age increased. All patients were treated by removal of hardware and appropriate antibiotic cover, following which the infection resolved spontaneously.
In conclusion, the occurrence of infection following orthognathic surgical procedures is influenced by multiple factors, and cannot be accurately predicted by a single variable. Variables include proper follow up care, abstinence from patient habits like smoking, the proper and correct usage of antibiotics [9, 17], drill speed, types of plates and screws [18, 19], and the presence of systemic disease among others. Future studies should aim at assessing correct treatment protocols for patients undergoing orthognathic surgery, and prospective study designs towards identification of risk factors with reference to various osteotomies, along with the evaluation of factors like oral hygiene, habits and hardware type.
Compliance with Ethical Standards
Conflict of interest
None.
References
- 1.Alpha C, O’Ryan F, Silva A, Poor D. The incidence of postoperative wound healing problems following sagittal ramus osteotomies stabilized with miniplates and monocortical screws. J Oral Maxillofac Surg. 2006;64:659–668. doi: 10.1016/j.joms.2005.12.013. [DOI] [PubMed] [Google Scholar]
- 2.Bhatt V, Langford RJ. Removal of miniplates in maxillofacial surgery: University Hospital Birmingham experience. J Oral Maxillofac Surg. 2003;61:553. doi: 10.1053/joms.2003.50108. [DOI] [PubMed] [Google Scholar]
- 3.Kuhlefelt M, Laine P, Suominen-Taipale L, Ingman T, Lindqvist C, Thoren H. Risk factors contributing to sympotomatic miniplate removal: a retrospective study of 153 bilateral sagittal split osteotomy patients. Int J Oral Maxillofac Surg. 2010;39:430–435. doi: 10.1016/j.ijom.2010.01.016. [DOI] [PubMed] [Google Scholar]
- 4.Spaey YJE, Bettens RMA, Mommaerts MY, Adriaens J, van Landuyt HW, Abeloos JVS, de Clercq CAS, Lamoral PRB, Neyt LF. A prospective study on infectious complications in orthognathic surgery. J Cranio Maxillofac Surg. 2005;33:24–29. doi: 10.1016/j.jcms.2004.06.008. [DOI] [PubMed] [Google Scholar]
- 5.Uhthoff HK, Bardow DI, Liskova-Kiar M. The advantages of titanium alloy over stainless steel plates for the fixation of fractures: an experimental study in dogs. J Bone Joint Surg Br. 1981;63-B(3):427–484. doi: 10.1302/0301-620X.63B3.7263759. [DOI] [PubMed] [Google Scholar]
- 6.Ellis E, Graham J. Use of a 2.0-mm locking plate/screw system for mandibular fracture surgery. J Oral Maxillofac Surg. 2002;60:642–645. doi: 10.1053/joms.2002.33110. [DOI] [PubMed] [Google Scholar]
- 7.Falter B, Schepers S, Vrielinck L, Lambrichts I, Politis C. Plate removal after orthognathic surgery. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;112:737–743. doi: 10.1016/j.tripleo.2011.01.011. [DOI] [PubMed] [Google Scholar]
- 8.Kuhlefelt M, Laine P, Suominen AL, Lindqvist C, Thoren H. Smoking as a siginificant risk factor for infections after orthognatic surgery. J Oral Maxillofac Surg. 2012;70:1643–1647. doi: 10.1016/j.joms.2011.06.224. [DOI] [PubMed] [Google Scholar]
- 9.Wahab PUA, Narayanan V, Nathan S, Madhulaxmi Antibiotic prophylaxis for bilateral sagittal split osteotomies: a randomised, double blind clinical study. Int J Oral Maxillofac Surg. 2013;42:352–355. doi: 10.1016/j.ijom.2012.10.036. [DOI] [PubMed] [Google Scholar]
- 10.Whiteford L. Nicotine, CO and HCN: the detrimental effects on smoking on wound healing. Br J Community Nurs. 2003;8:22. doi: 10.12968/bjcn.2003.8.Sup6.12554. [DOI] [PubMed] [Google Scholar]
- 11.Sloan A, Hussain I, Maqsood M, et al. The effects of smoking on fracture healing. Surg. 2010;8:111–116. doi: 10.1016/j.surge.2009.10.014. [DOI] [PubMed] [Google Scholar]
- 12.Larrazabal C, Garcia B, Penarrocha M, Pennarocha M. Influence of oral hygiene and smoking on pain and swelling after surgical extraction of impacted mandibular third molars. J Oral Maxillofac Surg. 2010;68:43–46. doi: 10.1016/j.joms.2009.07.061. [DOI] [PubMed] [Google Scholar]
- 13.Garcia B, Penarrocha M, Marti E, Gay-Escodad C, von Arx T. Pain and swelling after periapical surgery related to oral hygiene and smoking. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;104:271–276. doi: 10.1016/j.tripleo.2007.01.025. [DOI] [PubMed] [Google Scholar]
- 14.O’Connell J, Murphy C, Ikeagwuani O, Adley C, Kearns G. The fate of titanium miniplates and screws used in maxillofacial surgery: a 10 year retrospective study. Int J Oral Maxillofac Surg. 2009;38:731–735. doi: 10.1016/j.ijom.2009.02.016. [DOI] [PubMed] [Google Scholar]
- 15.Thoren H, Snail J, Kormi E, Lindqvist C, Suominen-Taipale L, Tornwall J. Symptomatic plate removal after treatment of facial fractures. J Cranio Maxillofac Surg. 2010;38:505–510. doi: 10.1016/j.jcms.2010.01.005. [DOI] [PubMed] [Google Scholar]
- 16.Manor Y, Chaushu G, Taicher S. Risk factors contributing to symptomatic plate removal in orthognathic surgery patients. J Oral Maxillofac Surg. 1999;57:679–682. doi: 10.1016/S0278-2391(99)90430-5. [DOI] [PubMed] [Google Scholar]
- 17.Baqain ZH, Hyde N, Patrikidou A, Harris M. Antibiotic prophylaxis for orthognathic surgery: a prospective, randomised clinical trial. Br J Oral Maxillofac Surg. 2004;42:506–510. doi: 10.1016/S0266-4356(04)00114-7. [DOI] [PubMed] [Google Scholar]
- 18.Norholt SE, Pedersen TK, Jensen J. Lefort 1 miniplate osteosynthesis: a randomised, prospective study comparing resorbable PLLA/PGA with titanium. Int J Oral Maxillofac Surg. 2004;33:245–252. doi: 10.1006/ijom.2003.0505. [DOI] [PubMed] [Google Scholar]
- 19.Turvey TA, Bell RB, Tejera TJ, Profitt WR. The use of self-reinforced biodegradable bone plates and screws in orthognathic surgery. J Oral Maxillofac Surg. 2002;60:59–65. doi: 10.1053/joms.2002.28274. [DOI] [PubMed] [Google Scholar]