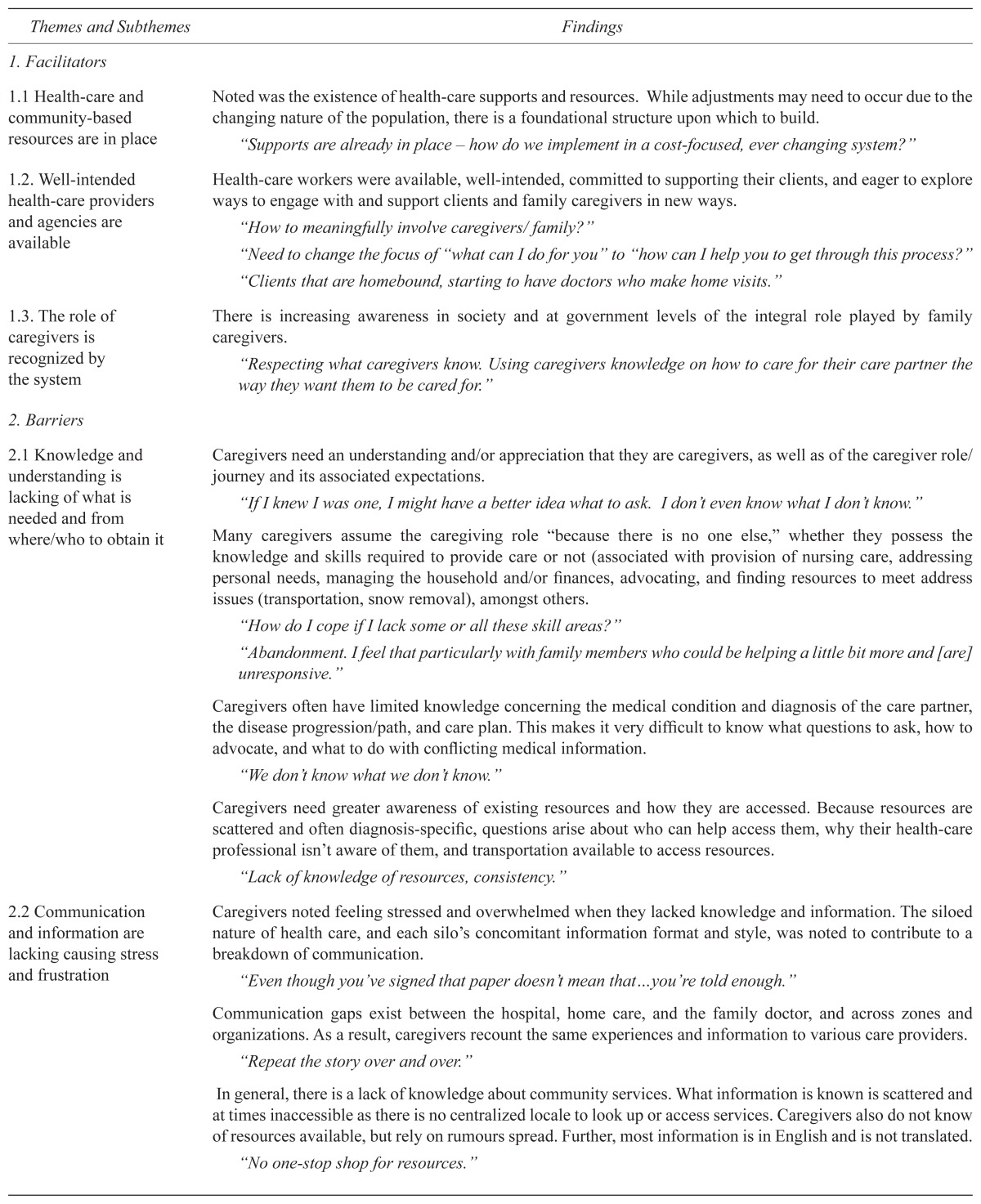
TABLE 2.
Supporting family caregivers of seniors with complex needs: facilitators/barriers to the provision of caregiver support
| Themes and Subthemes | Findings |
|---|---|
| 1. Facilitators | |
| 1.1 Health-care and community-based resources are in place | Noted was the existence of health-care supports and resources. While adjustments may need to occur due to the changing nature of the population, there is a foundational structure upon which to build. “Supports are already in place – how do we implement in a cost-focused, ever changing system?” |
| 1.2. Well-intended health-care providers and agencies are available | Health-care workers were available, well-intended, committed to supporting their clients, and eager to explore ways to engage with and support clients and family caregivers in new ways. “How to meaningfully involve caregivers/ family?” “Need to change the focus of “what can I do for you” to “how can I help you to get through this process?” “Clients that are homebound, starting to have doctors who make home visits.” |
| 1.3. The role of caregivers is recognized by the system | There is increasing awareness in society and at government levels of the integral role played by family caregivers. “Respecting what caregivers know. Using caregivers knowledge on how to care for their care partner the way they want them to be cared for.” |
| 2. Barriers | |
| 2.1 Knowledge and understanding is lacking of what is needed and from where/who to obtain it | Caregivers need an understanding and/or appreciation that they are caregivers, as well as of the caregiver role/journey and its associated expectations. “If I knew I was one, I might have a better idea what to ask. I don’t even know what I don’t know.” Many caregivers assume the caregiving role “because there is no one else,” whether they possess the knowledge and skills required to provide care or not (associated with provision of nursing care, addressing personal needs, managing the household and/or finances, advocating, and finding resources to meet address issues (transportation, snow removal), amongst others. “How do I cope if I lack some or all these skill areas?” “Abandonment. I feel that particularly with family members who could be helping a little bit more and [are] unresponsive.” Caregivers often have limited knowledge concerning the medical condition and diagnosis of the care partner, the disease progression/path, and care plan. This makes it very difficult to know what questions to ask, how to advocate, and what to do with conflicting medical information. “We don’t know what we don’t know.” Caregivers need greater awareness of existing resources and how they are accessed. Because resources are scattered and often diagnosis-specific, questions arise about who can help access them, why their health-care professional isn’t aware of them, and transportation available to access resources. “Lack of knowledge of resources, consistency.” |
| 2.2 Communication and information are lacking causing stress and frustration | Caregivers noted feeling stressed and overwhelmed when they lacked knowledge and information. The siloed nature of health care, and each silo’s concomitant information format and style, was noted to contribute to a breakdown of communication. “Even though you’ve signed that paper doesn’t mean that…you’re told enough.” Communication gaps exist between the hospital, home care, and the family doctor, and across zones and organizations. As a result, caregivers recount the same experiences and information to various care providers. “Repeat the story over and over.” In general, there is a lack of knowledge about community services. What information is known is scattered and at times inaccessible as there is no centralized locale to look up or access services. Caregivers also do not know of resources available, but rely on rumours spread. Further, most information is in English and is not translated. “No one-stop shop for resources.” |
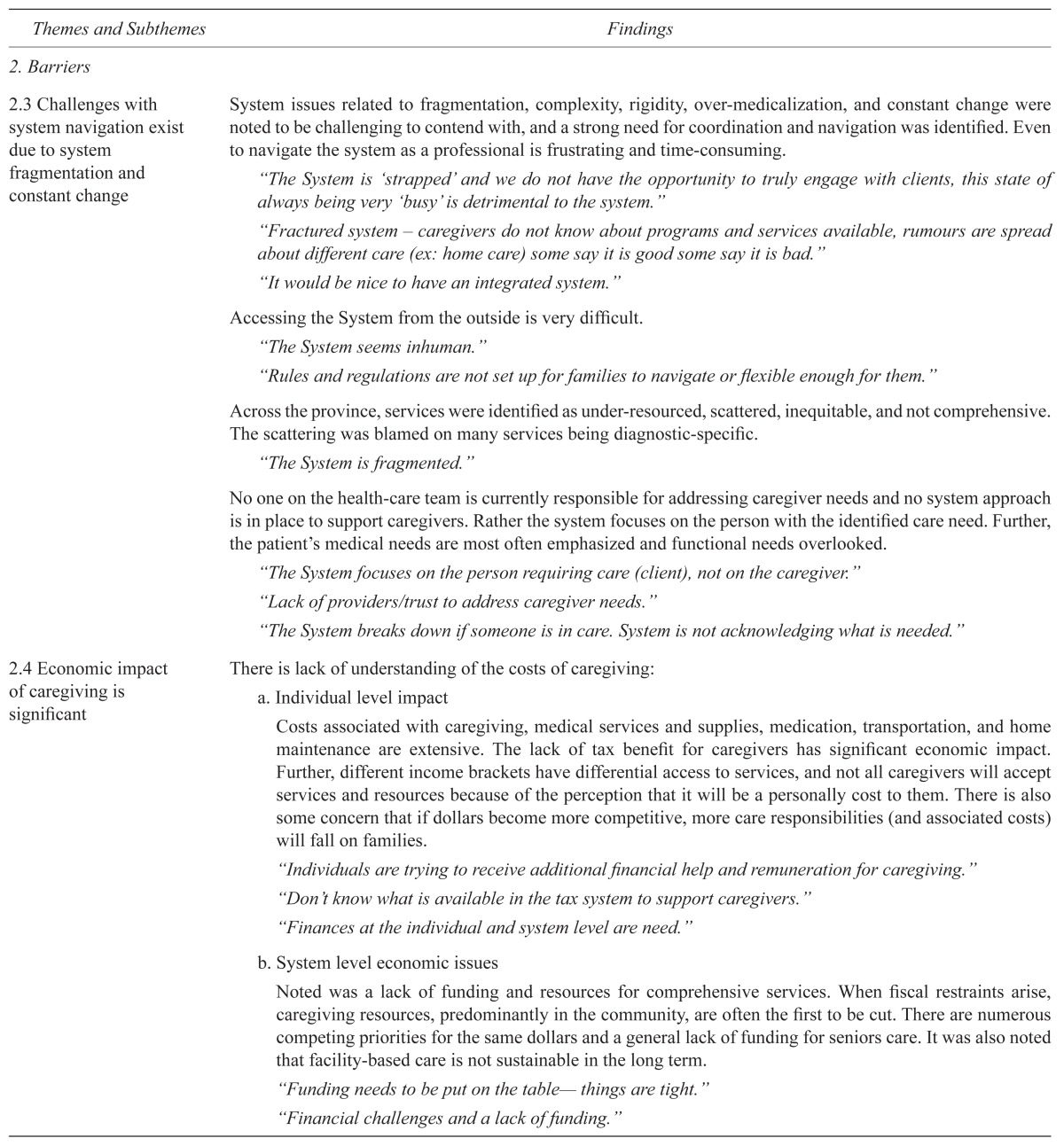
| 2.3 Challenges with system navigation exist due to system fragmentation and constant change | System issues related to fragmentation, complexity, rigidity, over-medicalization, and constant change were noted to be challenging to contend with, and a strong need for coordination and navigation was identified. Even to navigate the system as a professional is frustrating and time-consuming. “The System is ‘strapped’ and we do not have the opportunity to truly engage with clients, this state of always being very ‘busy’ is detrimental to the system.” “Fractured system – caregivers do not know about programs and services available, rumours are spread about different care (ex: home care) some say it is good some say it is bad.” “It would be nice to have an integrated system.” Accessing the System from the outside is very difficult. “The System seems inhuman.” “Rules and regulations are not set up for families to navigate or flexible enough for them.” Across the province, services were identified as under-resourced, scattered, inequitable, and not comprehensive. The scattering was blamed on many services being diagnostic-specific. “The System is fragmented.” No one on the health-care team is currently responsible for addressing caregiver needs and no system approach is in place to support caregivers. Rather the system focuses on the person with the identified care need. Further, the patient’s medical needs are most often emphasized and functional needs overlooked. “The System focuses on the person requiring care (client), not on the caregiver.” “Lack of providers/trust to address caregiver needs.” “The System breaks down if someone is in care. System is not acknowledging what is needed.” |
| 2.4 Economic impact of caregiving is significant | There is lack of understanding of the costs of caregiving:
|
| 2.5 Policies, processes and procedures can create barriers | There is a clear need to consider the whole picture, avoid repetition, and understand the needs of the community before changing the system. “We need to set caregiving in the policy context, and show how it will save politicians money. The current system focuses on addressing acute health-care conditions versus the whole picture. The needs of individuals with chronic health conditions are less resourced and underserved. Policies are rigid and not adapted to meet client/caregiver needs; rules and regulations are not set up to support families. Inconsistent and conflicting policies need to be examined. “Government policy seems to be random.” Regarding physician involvement, the question of resources was raised particularly regarding: 1) whether or not there are a sufficient number of physicians with expert knowledge who work with and are willing to support such a complex population of patients, 2) time required to provide care, and 3) remuneration. Changing the physician pay structure was identified as a need so that doctors have time to care for elderly persons with complex needs. “More doctors, pay structure for doctors – salary rather than fee for services.” “Family doctor is consistent, but there are often 6 family doctors as a group. Trust issues arise when there are of different opinions.” “Family physicians are a “key to unlock the door.” The Freedom of Information and Protection of Privacy Act (FOIP) is a barrier to caregivers in advocating for the care recipient, as it does not allow for sharing of information. “FOIP is a limitation/barrier when caring for a family member. Some professionals will bend the rules and share information and some will not.” |