Abstract
BACKGROUND:
Migraine is a common neurological condition that frequently presents to the emergency department (ED). Many medications are available to treat migraine. This study aims to characterize the demographics of patients who present to a large metropolitan ED with migraine, and to identify the medications used in treating this condition.
METHODS:
This study is a retrospective database interrogation of clinical records, used to collect quantitative data on patient demographics and medication prescriptions in the ED.
RESULTS:
A total of 2 228 patients were identified as being treated for migraine over a 10-year period. The proportion of the ED population presenting with migraine steadily increased in this time. Females (71%) more commonly presented to the ED with migraine than males. The migraine population was significantly younger (M=37.05, SD=13.23) than the whole ED population (M=46.17 SD=20.50) (P<0.001). A variety of medications were used in the treatment of migraine in the ED. Simple analgesics such as paracetamol and ibuprofen, anti-emetics and intravenous (IV) fluids with phenothiazine additives were commonly used. Over 20% of patients were prescribed oral or parenteral opiates (42 of 194 initial medication prescriptions, and 64 of 292 as required medication prescriptions). Triptans were very rarely used.
CONCLUSION:
Migraine is an increasingly common presentation to the ED. People presenting to the ED with migraine are more likely to be younger and female than the general ED population. Peak presentations for migraines occurred in January and February. The medications that are prescribed in the ED for migraine is varied and are not always in line with current evidence for the treatment of migraine. The excessive reliance on opiates and lack of the use of triptans denotes a significant variation from published guidelines.
KEY WORDS: Migraine, Headache, Pain, Emergency department, Analgesia
INTRODUCTION
Migraine is a common neurological condition affecting up to 12% of the general population.[1] Common symptoms include headache that is often throbbing and unilateral in nature, visual disturbance, nausea, and photophobia.[2] Migraine has a wide range of triggers which may include stress, heat, dehydration, fatigue and caffeine.[3]
Migraine-associated disability is substantial, with 90% of migraine patients reporting moderate to severe pain with a reduced ability to function during their migraine.[4] While migraine is not a life-threatening condition, the pain experienced can be severe and is a common presenting complaint to the emergency department (ED). Further understanding of the characteristics of the migraine patient presenting to the ED may minimize the duration and severity of symptoms.
Prevalence and impact
Migraine is a highly prevalent condition with a large burden on society. The Australian Bureau of Statistics reported 6% of Australians suffer from migraine, or 1.2 million people.[5] A major study conducted in the United States by Lipton et al[6] 2007 found that 18.2% of females suffered from migraine. Migraine-associated disability is substantial, with 53% of migraine patients reporting impairment in activities.[1] Migraine induced impairment has both indirect and direct costs. Indirect costs are through migraine induced disability which impacts on the patient’s work or study, and represents a loss in economic work force. Direct costs include outpatient visits, medications, emergency department visits, and hospital admissions. A study in the USA estimated that each ED visit for migraine costs $775, with annual costs of $700 million.[7]
Migraine emergency department demographic and arrival characteristics
Migraine is most common in women in their mid-thirties. An American study found that the prevalence of migraine in the ages between 30 and 39 was 28% in women and 9% in men.[6] The demographics of migraine patients who attend the ED is similar to the general migraine population. A study in 2011 conducted over 22 EDs in France noted that 75% of their ED migraine patients were female, with a mean age of 37.6.[8] A 2006 study on headache in United States EDs also noted that the majority of patients with migraine were females.[9] In Australia 71% of all patients presenting to the EDs with migraine were female, with a median age of 37 years.[10]
Arrival characteristics to the Emergency Department, such as time of arrival, mode of arrival, and triage category, may be useful prognostic factors for outcomes such as probability of admission, length of stay, or mortality.[11] There are few publications regarding ED arrival characteristics of migraine patients.
Treatment options and inconsistencies
The National Health and Medical Research Council’s (NHMRC) Emergency Care Acute Pain Management Manual provides an evidence based management approach for health care professionals to treat a number of conditions, including migraine. Their recommendations include aspirin, metoclopramide, chlorpromazine, prochlorperazine, and sumatriptan, which all have a strong evidence base.[12] Antiemetics including metoclopramide, chlorpromazine and prochlorperazine are effective for reducing both pain and nausea in migraine. Opioid use is discouraged.
Medications used to treat migraine in the ED are quite varied. In a survey of emergency physicians in Ontario, Canada, 15% of respondents said that their department had a migraine protocol and of these protocols, 16% included antiemetics, 11% NSAIDS, 9% ergotamines, 2% opiates and less than 1% included triptans.[13] An ED in Houston in the United States used an anti-emetic most commonly[14] while in Trieste in Italy, 90% of patients received an NSAID.[15] Opioids are also commonly used in the United States for migraine treatment, particularly meperidine.[16] An Australian audit found that paracetamol and codeine were overused in the treatment of migraine.[10]
Simple analgesics
Paracetamol has been shown to be superior to placebo.[17] NSAIDs are the mainstay for outpatient treatment and are useful for mild migraine, but must be used with caution in patients with a high risk of bleeding or kidney disease.[16,18]
Opiods
Opioids should be avoided in migraine treatment. They are associated with increases in headache frequency, increased headache-related disability, increased health-care resource utilization, and increased comorbidities including cardiovascular and psychiatric disorders including dependence. In one study 16.6% of current opioid users for migraine met the criteria for dependence.[19] Despite this, opioids are frequently used to treat migraine in North America. Their efficacy is no better than NSAID use, while having more side effects and a higher migraine recurrence rate.[20] Opioid use should only be considered as a last resort when other options are contraindicated or have failed.
Antiemetic dopamine antagonists
Antiemetics are an appropriate and effective first line treatment of migraine in an emergency department. Chlorpromazine,[21] droperidol,[22] prochlorperazine,[23] and metoclopramide[24] have shown anti-migraine efficacy and are relatively inexpensive. Prochlorperazine intravenously is just as or more effective than intravenous metoclopramide.[25]
Ergot derivatives
Ergotamine and dihydroergotamine are effective agents for migraine but have been superseded by triptans which have a more favorable side effect profile.[26] Ergotamine has a poor oral bioavailability, making an oral triptan more effective.[27]
Triptans
Triptans are an effective treatment for migraine.[28] Prescribing sumatriptan has shown improvement in overall heath functioning scores, fewer health care visits, and decreased absenteeism.[29] Triptans are particularly useful in cases with severe pain resistant to simple analgesia. The route of administration of triptans affects its efficacy. For example sumatriptan given subcutaneously has the fastest onset and highest efficacy as compared with when given orally, intranasal, or rectally.[17] However, this method of administration of sumatriptan also has the highest rate adverse effects.[17] Adverse effects include dizziness, fatigue, nausea, paraesthesia, and chest tightness.[30] Triptans have different levels of efficacy. At two hours eletriptan is the most effective triptan, followed by rizatriptan, zolmitriptan, and sumatriptan.[31]
METHODS
The study aimed to characterize the patients that present to a large metropolitan emergency department with migraine, and to identify the medications used in treating this condition.
Population
All patients presenting with migraine in the presentation to the ED or with migraine in the end diagnosis between March 2005 and December 2014 were included in this study.
Methodology
This study is a retrospective database interrogation of clinical records, used to collect quantitative data on patient demographics and medication prescriptions in the ED.
Demographics
Electronic data was extracted from Emergency Department Information System (EDIS), and the medical record. Each ED presentation is registered with EDIS, which records patient information such as demographic information, length of stay, mode of arrival, presenting complaint, discharge diagnosis, and discharge destination.
A migraine patient group was defined using two inclusion criteria: a) All patients who had the ED Departure Diagnosis ICD Code Primary of G43.9 – migraine. b) All patients who had “migraine” in their presenting complaint. These patients were then reviewed to exclude entries where migraine was a secondary complaint.
Figure 1 shows the final number of patients in the migraine group.
Figure 1.
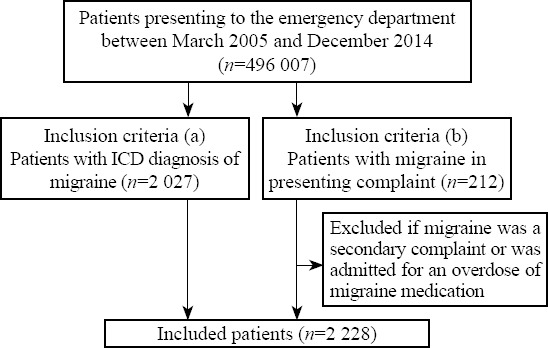
Included patients in migraine group.
Characteristics of the migraine patients were compared to those of the total ED population. These characteristics included sex, age, arrival time and date, mode of arrival, triage category, and length of stay.
Medication prescriptions
Migraine patients who arrived between June 4th 2014 and 31 December 2014 had their electronic medical chart retrieved. Medications and fluids given to these patients were collated. A total of 105 patient records were searched of which 98 patient medication charts were retrieved and used in the study. Electronic medication charts could not be retrieved for seven patients. Medication prescriptions were collated.
Analysis
Basic descriptive statistics are provided for all variable collected. Differences between the migraine population and the total ED population were tested using chi-square and analysis of variance tests. Significance was met at the P=0.05 level. Medication administration was presented in tabular format with both stat (immediate administration) and as required medications presented. Rates were presented per 1 000 presentations.
RESULTS
Patient demographics
There were a total of 496 007 presentations to the Emergency Department from March 2005 to December 2014. Descriptive statistics of those presentations is given in Table 1.
Table 1.
Demographic details, migraine population vs. total population, n (%)
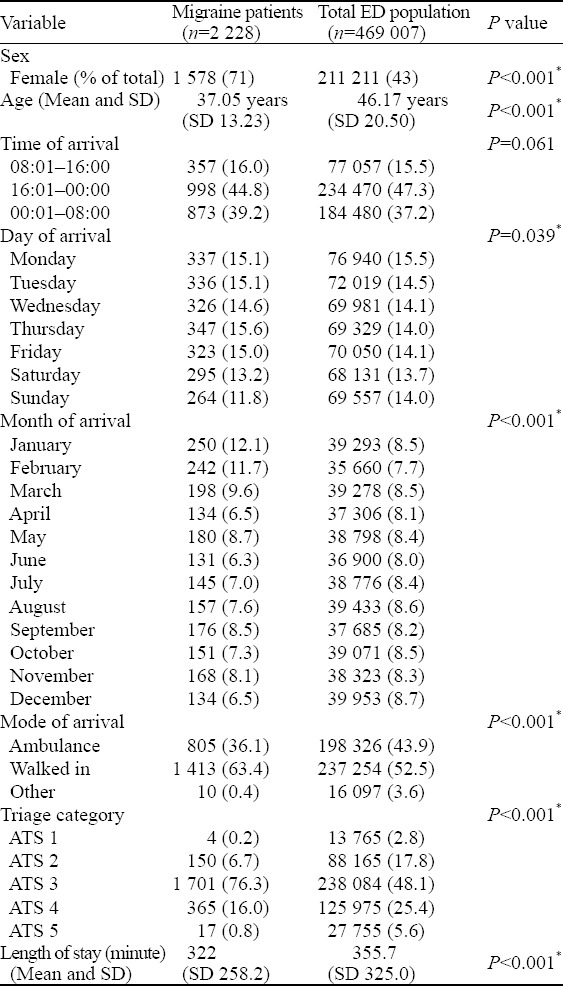
The mean age of patients presenting with migraine was 37.05 years (SD 13.23 years), which was significantly different to the total population (P<0.001) whose mean age was 46.17 (SD 20.50).
Migraine patients were more likely to arrive between day hours of 8 am and 4 pm than the evening hours of 4 pm to midnight, or midnight to 8 am [χ2 (2) =310.94, P<0.001]. Attendance was different depending on the day, with patients attending the ED less on the weekend and most on Thursday [χ2 (6) =15.90, P=0.014].
Patients with migraines were more likely to arrive in January or February than any other month of the year and this was significantly different to the rest of the population’s presentation patterns (P<0.001). Between 2005 and 2014, migraine presentations made up between 0.34%–0.61% of total ED presentations, which has been increasing in more recent years (Figure 2).
Figure 2.
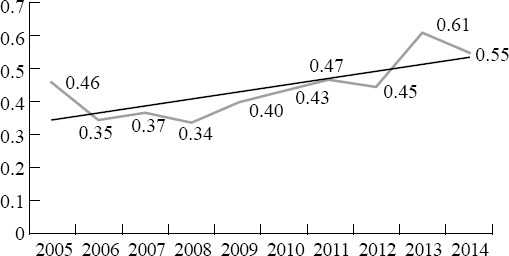
Percentage of the total ED presentations presenting with migraine over time.
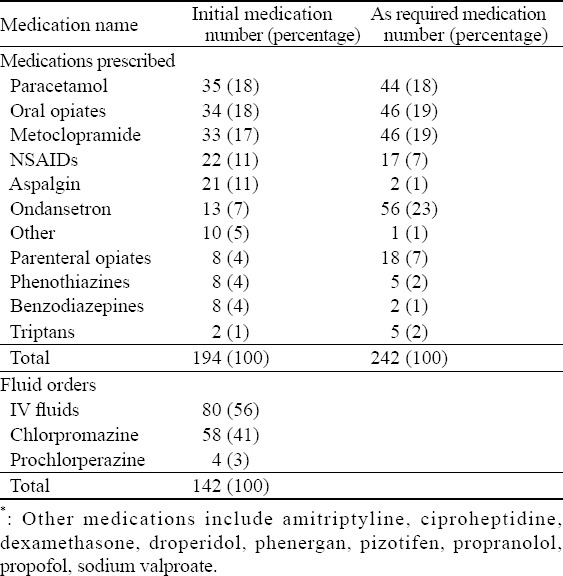
Medication prescriptions
Ninety-eight patient medication charts showed a total of 194 initial medication prescriptions, 242 as required medication prescriptions, and 142 fluid order prescriptions (Table 2).
Table 2.
Medications prescribed to the 98 patients in the migraine treatment cohort, n (%)
DISCUSSION
Demographics
The patient demographics in this study is similar to other studies of migraine patients, with females of reproductive age more commonly affected by the condition.[6] Interestingly, the migraine patient demographics of sex and age of this study are similar to those of a previous Australian study conducted by Kelly et al.[10]
The difference in prevalence between the sexes is likely to be multifactorial, but there is considerable evidence for sex hormone fluctuation as an important role.[32] The migraine population in the ED differs from the general ED population, which see more males and is older than the migraine population.
Triage
Migraine patients were mainly triaged into category three (76.6%). Interestingly, age of patients did not affect triage category but gender did, with females being triaged into more urgent categories. Data comparing the symptom severity between men and women show that women experience aura more commonly and have a greater impairment than males.[33] It is possible that women experience migraine symptoms more severely and are thus triaged more urgently.
Triggers affecting arrival time and increased arrivals
Arrival time results in this study may be related to migraine triggers. It was found that patients were least likely to present on Sunday, with a peak in presentations on Thursday. Similarly, Hoffman et al[34] found a peak of migraine events mid-week, with the least number of events being on Sunday. Stress is the most commonly reported trigger factor for migraine.[35] It is possible that work-related stress on business days is a trigger for migraine attacks, while Sunday, traditionally a work-free day, has a lower incidence of migraine attacks.
More migraine patients arrived in January and February. This contrasts to the general ED population which has a consistent frequency of presentation across all months. Heat and dehydration is a trigger for migraine in some patients.[3] This is unlikely related to increased presentations in January and February, as December, another extremely hot month for this study centre area, has one of the lowest percentage of arrivals. The lower number of presentations in December could be in relation to the commencement of the holiday season. The increased presentations in January and February could be related to stress, with many people starting work or study at the beginning of the year.
The proportion of migraine patients arriving to the ED has steadily increased (Figure 2). Reasons for this are unclear.
Medications
There are no placebo-controlled studies demonstrating the effectiveness of narcotic agents in migraine.[36] This study indicates that narcotic agents are being prescribed frequently for migraine patients (Table 2). This is also prevalent in the United States, where opioids are the most commonly prescribed medication for treating migraine in EDs.[20] Criticisms for opioid use in migraine patients include low efficacy, increased recurrence, and high rates of adverse effects.[16] Opioids are commonly given for other acute pain conditions as they are generally safe and well-tolerated. However, migraine is better treated with alternative medication.
Similar to other studies, we found that triptan usage was minimal (Table 2). Despite triptans being recommended in the guidelines, it is used much less frequently than chlorpromazine or prochlorperazine. This could be because of the increased cost of the medication, potential cardiovascular risks involved with triptans, or unfamiliarity with the medication.[13]
While triptan use at this ED was minimal, phenothiazines and metoclopramide were commonly used. Our study found that metoclopramide, prochlorperazine, and chlorpromazine were also often prescribed for migraine, in line with the evidence and suggestions provided by the NHMRC.[36] These agents should be continued to be encouraged for the treatment of migraine in the ED.
Impact and costs
Despite the relatively small proportion of ED presentations with migraine, there is a significant cost involved with migraine patients attending the ED. Over one third (36%) of patients arrived by ambulance and the average length of stay was 322 minutes.
Initial opiate use for migraine is associated with a longer length of stay as compared with non-opiate first line agents.[37] Our study found that opioid prescriptions for migraine in the ED was common (Table 2). Decreasing length of stay is associated with reduced ED crowding which has substantial cost savings.[38] Thus the reduction of opioid prescriptions for migraine in the ED and provision of adequate treatment may lead to patients receiving quicker and better relief of symptoms, reduced length of stay, and economic benefits for the healthcare system.
Limitations
This study found a low proportion of migraine patients arriving to the ED as compared with other studies. We undertook a conservative approach and used a strict inclusion criteria to identify migraine. It is possible that migraine patients were diagnosed with “benign headache” or “non-specific headache” which would not have been included. Furthermore, there could have been patients with a non-migraine headache who were mistakenly diagnosed with migraine. A detailed chart review utilising the international classification of headache disorder definitions may have increased the sensitivity and specificity of our study, however this was not possible due to time and resource constraints.
The medication prescription analysis of this study was restricted to 98 patients admitted after mid 2014 for whom scanned electronic medication records were available. Despite these smaller numbers, the continued use of opioids for migraine in this hospital is evident.
CONCLUSION
There are numerous medications available to treat migraine in the ED. Opioid prescription for migraine remains high despite guidelines recommending otherwise. Metoclopramide and phenothiazines are also commonly prescribed, which is in line with current recommendations. Triptans were very rarely prescribed.
Opioid medication prescriptions for migraine needs to be reduced in favour of recommended medications such as metoclopramide, chlorpromazine, prochlorperazine, and sumatriptan. The introduction of evidence based protocols for the treatment of migraine in the emergency department may help reduce the use of narcotics and ultimately provide patients better symptom relief as well as provide economic benefits to the healthcare system.
Footnotes
Funding: None.
Ethical approval: Not needed.
Conflicts of interest: There is no conflict of interest related to this study.
Contributors: RE and ES conceived the study, wrote the protocol and collected the data. JH provided topic specific expertise. RE, ES and JH analysed the data. JH wrote the manuscript with significant input from RE and ES. All authors had final say over the manuscript.
REFERENCES
- 1.Lipton R, Stewart W, Diamond S, Diamond M. Prevalence and burden of migraine in the United States:Data From the American Migraine Study II. Headache. 2001;41(7):646–57. doi: 10.1046/j.1526-4610.2001.041007646.x. [DOI] [PubMed] [Google Scholar]
- 2.Smetana GW. The diagnostic value of historical features in primary headache syndromes:A comprehensive review. Arch Intern Med. 2000;160(18):2729–37. doi: 10.1001/archinte.160.18.2729. [DOI] [PubMed] [Google Scholar]
- 3.Wöber C, Wöber-Bingöl Ç. Triggers of migraine and tension-type headache. Handb Clin Neurol. 2010;97(C):161–72. doi: 10.1016/S0072-9752(10)97012-7. [DOI] [PubMed] [Google Scholar]
- 4.Stewart WF, Lipton RB, Simon D. Work-related disability:Results from the American Migraine Study. Cephalalgia. 1996;16(4):231–8. doi: 10.1046/j.1468-2982.1996.1604231.x. [DOI] [PubMed] [Google Scholar]
- 5.Year Book Australia 2012. Statistics ABo. Canberra, Australia 2012: [Google Scholar]
- 6.Lipton R, Bigal M, Diamond M, Freitag F. Migraine prevalence, disease burden, and the need for preventive therapy. Neurology. 2007;68(5):343–9. doi: 10.1212/01.wnl.0000252808.97649.21. [DOI] [PubMed] [Google Scholar]
- 7.Insinga RP, Ng-Mak DS, Hanson ME. Costs associated with outpatient, emergency room and inpatient care for migraine in the USA. Cephalalgia. 2011;31(15):1570–5. doi: 10.1177/0333102411425960. [DOI] [PubMed] [Google Scholar]
- 8.Valade D, Lucas C, Calvel L, Plaisance P, Derouet N, Meric G, et al. Migraine diagnosis and management in general emergency departments in France. Cephalalgia. 2011;31(4):471–80. doi: 10.1177/0333102410378178. [DOI] [PubMed] [Google Scholar]
- 9.Goldstein JN, Camargo CA, Pelletier AJ, Edlow JA. Headache in United States emergency departments:Demographics, work-up and frequency of pathological diagnoses. Cephalalgia. 2006;26(6):684–90. doi: 10.1111/j.1468-2982.2006.01093.x. [DOI] [PubMed] [Google Scholar]
- 10.Kelly A-M, Knott J, Bennetts S. Treatment of migraine in Australian emergency departments. Emerg Med Australas. 2009;21(4):333–4. doi: 10.1111/j.1742-6723.2009.01206.x. [DOI] [PubMed] [Google Scholar]
- 11.Cameron A, Rodgers K, Ireland A, Jamdar R, McKay GA. A simple tool to predict admission at the time of triage. Emerg Med J. 2015;32(3):174–9. doi: 10.1136/emermed-2013-203200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Studies NIoC. Emergency Care Acute Pain Management Manual. 2011 [Google Scholar]
- 13.Nijjar SS, Pink L, Gordon AS. Examination of migraine management in emergency departments. Pain Res Manag. 2011;16(3):183–6. doi: 10.1155/2011/182867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Morgenstern LB, Huber JC, Luna-Gonzales H, Saldin KR, Grotta JC, Shaw SG, et al. Headache in the Emergency Department. Headache. 2001;41(6):537–41. doi: 10.1046/j.1526-4610.2001.041006537.x. [DOI] [PubMed] [Google Scholar]
- 15.Relja G, Granato A, Capozzoli F, Maggiore C, Catalan M, Pizzolato G, et al. Nontraumatic headache in the Emergency Department:a survey in the province of Trieste. J Headache Pain. 2005;6(4):298–300. doi: 10.1007/s10194-005-0213-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Friedman BW, Grosberg BM. Diagnosis and management of the primary headache disorders in the emergency department setting. Emerg Med Clin North Am. 2009;27(1):71–87, viii. doi: 10.1016/j.emc.2008.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Derry S, Moore RA. Paracetamol (acetaminophen) with or without an antiemetic for acute migraine headaches in adults. Cochrane Database of Systematic Reviews [Internet] 2013. Available from: http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD008040.pub3/abstract . [DOI] [PMC free article] [PubMed]
- 18.Kirthi V, Derry S, Moore RA. Aspirin with or without an antiemetic for acute migraine headaches in adults. Cochrane Database Syst Rev. 2013;(4) doi: 10.1002/14651858.CD008041.pub3. CD008041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Buse DC, Pearlman SH, Reed ML, Serrano D, Ng-Mak DS, Lipton RB. Opioid use and dependence among persons with migraine:results of the AMPP study. Headache. 2012;52(1):18–36. doi: 10.1111/j.1526-4610.2011.02050.x. [DOI] [PubMed] [Google Scholar]
- 20.Friedman BW, Serrano D, Reed M, Diamond M, Lipton RB. Use of the emergency department for severe headache. A population-based study. Headache. 2009;49(1):21–30. doi: 10.1111/j.1526-4610.2008.01282.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bigal ME, Bordini CA, Speciali JG. Intravenous chlorpromazine in the Emergency Department treatment of migraines:a randomized controlled trial. J Emerg Med. 2002;23(2):141–8. doi: 10.1016/s0736-4679(02)00502-4. [DOI] [PubMed] [Google Scholar]
- 22.Silberstein SD, Young WB, Mendizabal JE, Rothrock JF, Alam AS. Acute migraine treatment with droperidol:A randomized, double-blind, placebo-controlled trial. Neurology. 2003;60(2):315–21. doi: 10.1212/01.wnl.0000042477.63516.b2. [DOI] [PubMed] [Google Scholar]
- 23.Jones J, Sklar D, Dougherty J, White W. Randomized double-blind trial of intravenous prochlorperazine for the treatment of acute headache. JAMA. 1989;261(8):1174–6. [PubMed] [Google Scholar]
- 24.Colman I, Brown MD, Innes GD, Grafstein E, Roberts TE, Rowe BH. Parenteral Metoclopramide for acute migraine:Meta-Analysis of randomisedcontrolled trials. BMJ. 2004;329(7479):1369–72. doi: 10.1136/bmj.38281.595718.7C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Friedman BW, Esses D, Solorzano C, Dua N, Greenwald P, Radulescu R, et al. A randomized controlled trial of prochlorperazine versus metoclopramide for treatment of acute migraine. Ann Emerg Med. 2008;52(4):399–406. doi: 10.1016/j.annemergmed.2007.09.027. [DOI] [PubMed] [Google Scholar]
- 26.Goadsby P, Olesen J. Diagnosis and management of migraine. BMJ. 1996;312:1283–7. doi: 10.1136/bmj.312.7041.1279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tfelt-Hansen P. History of headache research in Denmark. Cephalalgia. 2001;21(7):748–52. doi: 10.1177/033310240102100702. [DOI] [PubMed] [Google Scholar]
- 28.Ferrari MD, Goadsby PJ, Roon KI, Lipton RB. Triptans (serotonin, 5-HT1B/1D agonists) in migraine:detailed results and methods of a meta-analysis of 53 trials. Cephalalgia. 2002;22(8):633–58. doi: 10.1046/j.1468-2982.2002.00404.x. [DOI] [PubMed] [Google Scholar]
- 29.Lofland JH, Johnson NE, Nash DB, Lofland JH, Batenhorst AS. Changes in resource use and outcomes for patients with migraine treated with sumatriptan:A managed care perspective. Arch Intern Med. 1999;159(8):857–63. doi: 10.1001/archinte.159.8.857. [DOI] [PubMed] [Google Scholar]
- 30.Johnston MM, Rapoport AM. Triptans for the management of migraine. Drugs. 2010;70(12):1505–18. doi: 10.2165/11537990-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 31.Thorlund K, Mills EJ, Wu P, Ramos E, Chatterjee A, Druyts E, et al. Comparative efficacy of triptans for the abortive treatment of migraine:a multiple treatment comparison meta-analysis. Cephalalgia. 2014;34(4):258–67. doi: 10.1177/0333102413508661. [DOI] [PubMed] [Google Scholar]
- 32.Chai NC, Peterlin BL, Calhoun AH. Migraine and estrogen. Curr Opin Neurol. 2014;27(3):315–24. doi: 10.1097/WCO.0000000000000091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Buse DC, Loder EW, Gorman JA, Stewart WF, Reed ML, Fanning KM, et al. Sex differences in the prevalence, symptoms, and associated features of migraine, probable migraine and other severe headache:results of the American Migraine Prevalence and Prevention (AMPP) Study. Headache. 2013;53(8):1278–99. doi: 10.1111/head.12150. [DOI] [PubMed] [Google Scholar]
- 34.Hoffmann J, Schirra T, Lo H, Neeb L, Reuter U, Martus P. The influence of weather on migraine –are migraine attacks predictable? Ann Clin Transl Neurol. 2015;2(1):22–8. doi: 10.1002/acn3.139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kelman L. The triggers or precipitants of the acute migraine attack. Cephalalgia. 2007;27(5):394–402. doi: 10.1111/j.1468-2982.2007.01303.x. [DOI] [PubMed] [Google Scholar]
- 36.Holdgate A, Kelly A. Emergency Care Evidence in Practice Series:Management of Acute Migraine. 2006 [Google Scholar]
- 37.McCarthy LH, Cowan RP. Comparison of parenteral treatments of acute primary headache in a large academic emergency department cohort. Cephalalgia. 2015;35(9):807–15. doi: 10.1177/0333102414557703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Foley M, Kifaieh N, Mallon WK. Financial impact of emergency department crowding. West J Emerg Med. 2011;12(2):192–7. [PMC free article] [PubMed] [Google Scholar]


