Abstract
Purpose:
To understand soft contact lens (SCL) and gas-permeable (GP) lens wearers' behaviors and knowledge regarding exposure of lenses to water.
Methods:
The Contact Lens Risk Survey (CLRS) and health behavior questions were completed online by a convenience sample of 1056 SCL and 85 GP lens wearers aged 20 to 76 years. Participants were asked about exposing their lenses to water and their understanding of risks associated with these behaviors. Chi-square analyses examined relationships between patient behaviors and perceptions.
Results:
GP lens wearers were more likely than SCL wearers to ever rinse or store lenses in water (rinsing: 91% GP, 31% SCL, P < 0.001; storing: 33% GP, 15% SCL P < 0.001). Among SCL wearers, men were more likely to store (24% vs. 13%, P = 0.003) or rinse (41% vs. 29%, P = 0.012) their lenses in water. Showering while wearing lenses was more common in SCL wearers (86%) than GP lens wearers (67%) (P < 0.0001). Swimming while wearing lenses was reported by 62% of SCL wearers and 48% of GP lens wearers (P = 0.027). Wearers who rinsed (SCL; P < 0.0001, GP; P = 0.11) or stored lenses in water (SCL; P < 0.0001, GP P = 0.007) reported that this behavior had little or no effect on their infection risk, compared with those who did not. Both SCL (P < 0.0001) and GP lens wearers (P < 0.0001) perceived that distilled water was safer than tap water for storing or rinsing lenses.
Conclusions:
Despite previously published evidence of Acanthamoeba keratitis' association with water exposure, most SCL, and nearly all GP lens wearers, regularly expose their lenses to water, with many unaware of the risk.
Key Words: soft contact lenses, gas-permeable lenses, Acanthamoeba, keratitis, swimming, showering
There are approximately 40.9 million contact lens wearers in the United States, of whom >90% wear soft contact lenses (SCL).1 Proper lens care, such as replacing care solution daily,2 using a clean storage case,3 and avoiding overnight wear,4 is essential to minimize the risk of adverse events such as microbial keratitis (MK) and corneal inflammatory events (CIEs). One of the most visually devastating forms of MK is Acanthamoeba keratitis (AK). Nearly 85%5 of Acanthamoeba cases occur in contact lens wearers, and a primary risk factor for developing AK is exposing contact lenses to water.6
Acanthamoeba has been found in air, dust, soil, and water—including tap water.5,7 Contact lens wearers have contracted Acanthamoeba from exposure to pools,8 hot tubs,8 homemade saline,9 and from household tap water.10 Other commonly isolated pathogenic microbes associated with contact lens-related complications include strains of Pseudomonas, Serratia, Stenotrophomonas, and Achromobacter, all of which can be found in tap water or in plumbing system biofilms.11,12
Avoiding tap water exposure when wearing contact lenses is important,10 yet, many gas-permeable (GP) lens product package inserts instruct the patient to use water during the lens cleaning process and most SCL package instructions do not mention risk of exposure of lenses to water. Such water exposure potentially contaminates the lens and storage case and places the patient at risk for serious infection. A recent case report draws attention to an AK case, in which a patient complied with manufacturer GP care solution guidelines, which included a tap water-rinsing step, and an infection developed.13 Those authors emphatically called for changes in industry labeling and in practice to eliminate the use of tap water for cleaning GP lenses or any storage cases. They also sought better warnings for patients on the danger of using tap or distilled water for lens care.13
Despite warnings from the United States Food and Drug Administration (FDA)14 and the Centers for Disease Control and Prevention (CDC)15 about the risks of contact lens exposure to water, products that instruct wearers to use tap water during cleaning and rinsing remain on the market and cases of AK have not declined since the 2007 US multistate Acanthamoeba keratitis outbreak investigation.16
The purpose of this study was to evaluate the attitudes and behaviors of a contemporary cohort of contact lens wearers regarding their lenses and water exposure through an online survey of behaviors and perceptions relating to contact lens wear.
METHODS
This study is a secondary analysis of data collected from an adult population to evaluate self-reported behaviors related to contact lens wear and water exposure. The study followed the Declaration of Helsinki and received approval from The Ohio State University Institutional Review Board. To be an eligible participant, one had to be a current (wore lenses in the week preceding the survey) GP or SCL wearer aged 18 years or above. Participants were recruited by a marketing research company (Schlesinger Associates, Iselin, NJ), which fielded the survey online. Participants were members of the research firm's market research panel and wore contact lenses. Panel members were recruited in-person, through internet advertising, e-mail campaigns, or telephone calls. Panel members were located in the United States and were not geographically restricted.
To describe the prevalence of the hygiene and demographic factors related to contact lens wear, the Contact Lens Risk Survey (CLRS)17 was administered to the sample of contact lens wearers described above.1 The CLRS was developed for SCL wearers and was adapted to include GP lens wearers. The CLRS uses a standard methodology and validated set of questions,17,18 including questions pertaining to self-reported demographics, closed eye conditions, exposure of lenses to water, and case hygiene. Several questions were also added to assess perceptions and beliefs toward behaviors of contact lens wear and care.
Water-related behaviors surveyed included rinsing lenses with tap water, storing lenses in tap water, showering with lenses, swimming while wearing lenses, and handling of the lens case after lens application to the eye. Response options for the frequency of practicing a behavior were “always,” “fairly often,” “sometimes,” “infrequently,” and “never.” For swimming, the response options were “daily,” “weekly,” “monthly,” “<monthly,” and “never.” Options for what was done with the lens case after lenses have been placed on the eye included “rinse with solution,” “rinse with water,” “dry with tissue,” “put caps back on,” “air dry without caps,” and “other.” For several behaviors, participants' perceptions were queried as to whether a particular behavior “prevents infection,” “has little/no effect,” or “is likely to cause infection.”
Because of the inherent risk of exposing contact lenses to water, participants with a reported response of ever practicing a behavior (ie, always, fairly often, sometimes, infrequently) were grouped together during analysis and then compared with those who reported never performing that behavior. Using χ2 analysis, statistical comparisons were made regarding specific behaviors and their corresponding perceptions. The Bowker test of symmetry was used to compare perceptions related to tap and distilled water for rinsing and storing lenses. Additional corrections for multiple comparisons were not incorporated. Sample sizes for each reported behavior or perception differ because of incomplete responses.
RESULTS
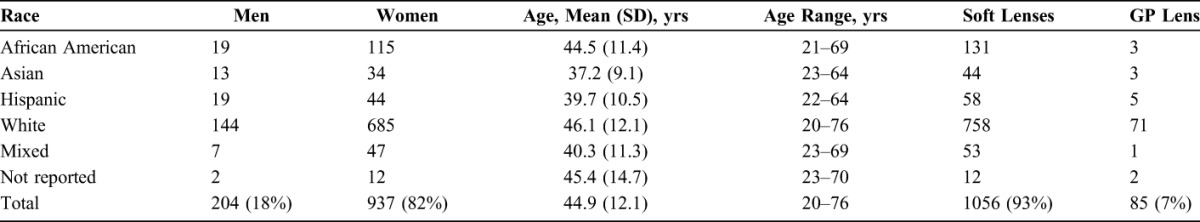
The survey was completed by 1141 adults consisting of 1056 SCL wearers and 85 GP lens wearers. The SCL wearers were younger (range: 20–76 yrs, mean 44.3 ± 11.9 yrs) than the GP lens wearers (range: 23–74 yrs, mean: 52.7 ± 12.4 yrs) (P < 0.0001). The majority of participants were women and white (Table 1).
TABLE 1.
Demographic Characteristics of CLRS Participants
Exposures to Water
Of the 85 GP lens wearers surveyed, 81 provided responses to the rinsing and storing questions. Of those 81, 91% reported that they ever rinsed their lenses with tap water, compared with 31% of the 1008 SCL wearers (P < 0.001) (Fig. 1). Of the 81 GP lens wearers, 33% reported storing lenses in tap water compared with 15% of 894 SCL wearers (P < 0.001) (Fig. 1). Of 184 male SCL wearers, 41% reported rinsing their lenses with tap water compared with 29% of 824 female SCL wearers (P = 0.012), but this difference was not found among 12 male GP lens wearers (100%) and 90% of 69 female GP lens wearers (P = 0.22). Of 163 male SCL wearers, 24% reported storing their lenses in water compared with 13% of 731 female SCL wearers (P = 0.003), but this difference was not found among 58% of 12 male and 33% of 69 female GP lens wearers (P = 0.17).
FIGURE 1.
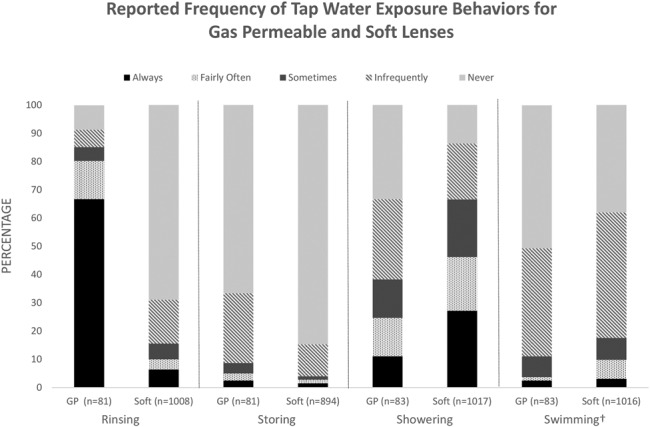
Reported frequency of soft lens and gas-permeable lens exposure to water through rinsing, storing, showering, or swimming. †Swimming frequency recorded as daily, weekly, monthly, <monthly, never. GP, gas-permeable lens; Soft, soft lens.
Of 278 SCL wearers who reported ever rinsing lenses with tap water, 115 (41%) stored lenses in tap water compared with 22 (4%) of the 615 who never rinsed lenses with tap water (P < 0.0001). Of 278 SCL wearers who reported ever rinsing lenses with tap water, 141 (51%) reported rinsing their storage case with tap water as compared with 231 (37%) of 619 who did not rinse lenses with tap water (P < 0.0001). Wearers of GP lenses who reported ever rinsing lenses with tap water (n = 74) were equally likely to store lenses in tap water (32%) compared with those who never rinsed lenses with tap water (43%) (P = 0.31). Of 74 GP lens wearers, 59% who reported rinsing lenses with water also rinsed their storage case with tap water compared with 28% of the nontap water-rinsing group (P = 0.011).
Showering while wearing lenses was the most common exposure to water for SCL wearers, reported by 878 (86%), and was reported by 54 (67%) of GP lens wearers (Fig. 1). There was no difference in exposure for showering while wearing contact lenses between male SCL wearers (90% of 186) and female SCL wearers (86% of 831) (P = 0.66) or male GP lens wearers (85% of 13) and female GP lens wearers (64% of 70) (P = 0.27). Swimming while wearing contact lenses was reported in 62% of 1016 SCL wearers and 51% of 83 GP lens wearers (Fig. 1). There was no difference in reported exposure for swimming while wearing contact lenses between 66% of 186 male SCL wearers and 61% of 830 female SCL wearers (P = 0.63) or 38% of 13 GP lens-wearing males and 53% of 70 GP-wearing females (P = 0.07).
For other known CIE or MK risk factors, SCL wearers who ever rinsed lenses with tap water were more likely to wear lenses overnight (always or often; 27% of 313), compared with those who never rinsed lenses with tap water (15% of 694; P < 0.0001). Of 137 SCL wearers who ever stored lenses in tap water, 30% wore lenses overnight (always or often) compared with 16% of the 757 who never stored lenses in tap water (P < 0.0001). Wearers of SCL who rinsed lenses with tap water were also more likely to never, infrequently, or sometimes discard solution (22% of 278) compared with the nonrinsing group (9% of 622) (P < 0.0001). This was the same for SCL wearers who stored lenses in tap water (26% of 137) compared with the nonstoring group (10% of 757) (P < 0.0001).
Perception of Risk Related to Water Exposure of Lenses
Compared with GP lens wearers, SCL wearers perceived a greater risk of acquiring infection through rinsing lenses with tap or distilled water or storing lenses in tap or distilled water (all P < 0.0001) (Table 2).
TABLE 2.
Perception of Risk Related to Contact Lens Water Exposure
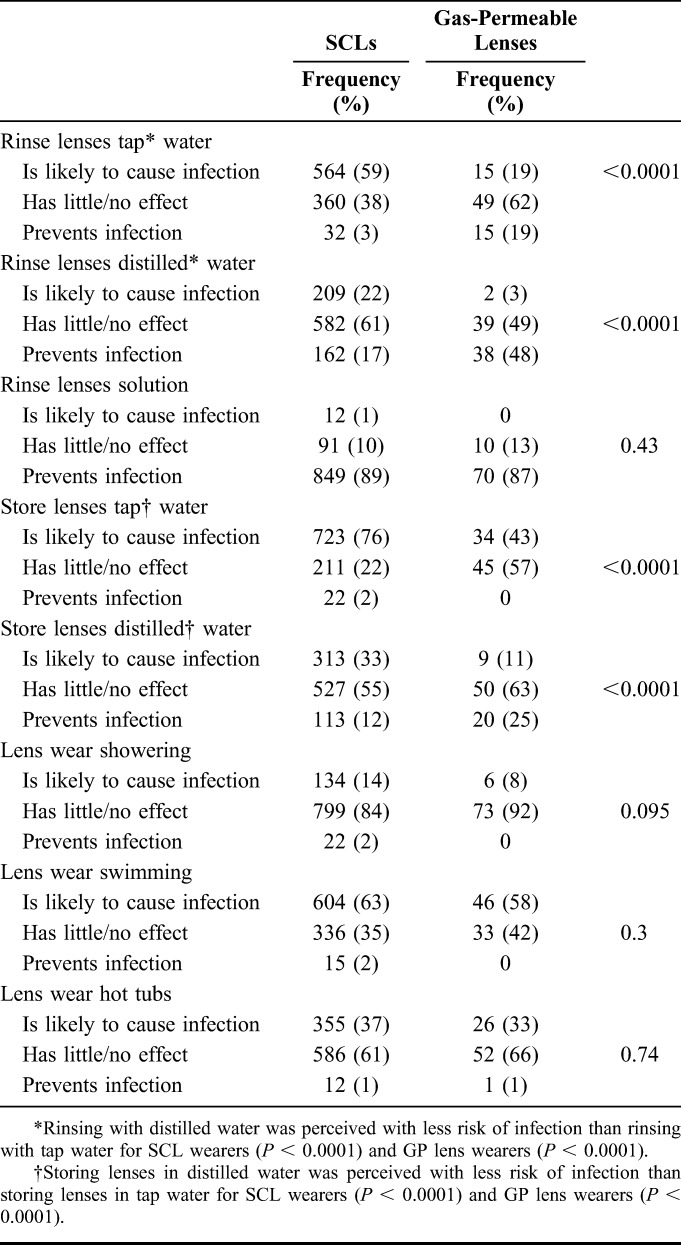
Rinsing lenses with distilled water was perceived as having less risk than rinsing lenses with tap water. This was true for all SCL wearers regardless of whether they rinsed with tap water (P < 0.0001, all) and for GP lens wearers who reported rinsing lenses with tap water (P < 0.0001) (Table 3). Storing lenses in distilled water was perceived as having less risk than storing lenses in tap water for all wearers, regardless of whether they stored lenses in tap water (P < 0.0001, all groups).
TABLE 3.
Perception of Risk Related to Contact Lens Water Exposure by Actual Reported Water Exposure
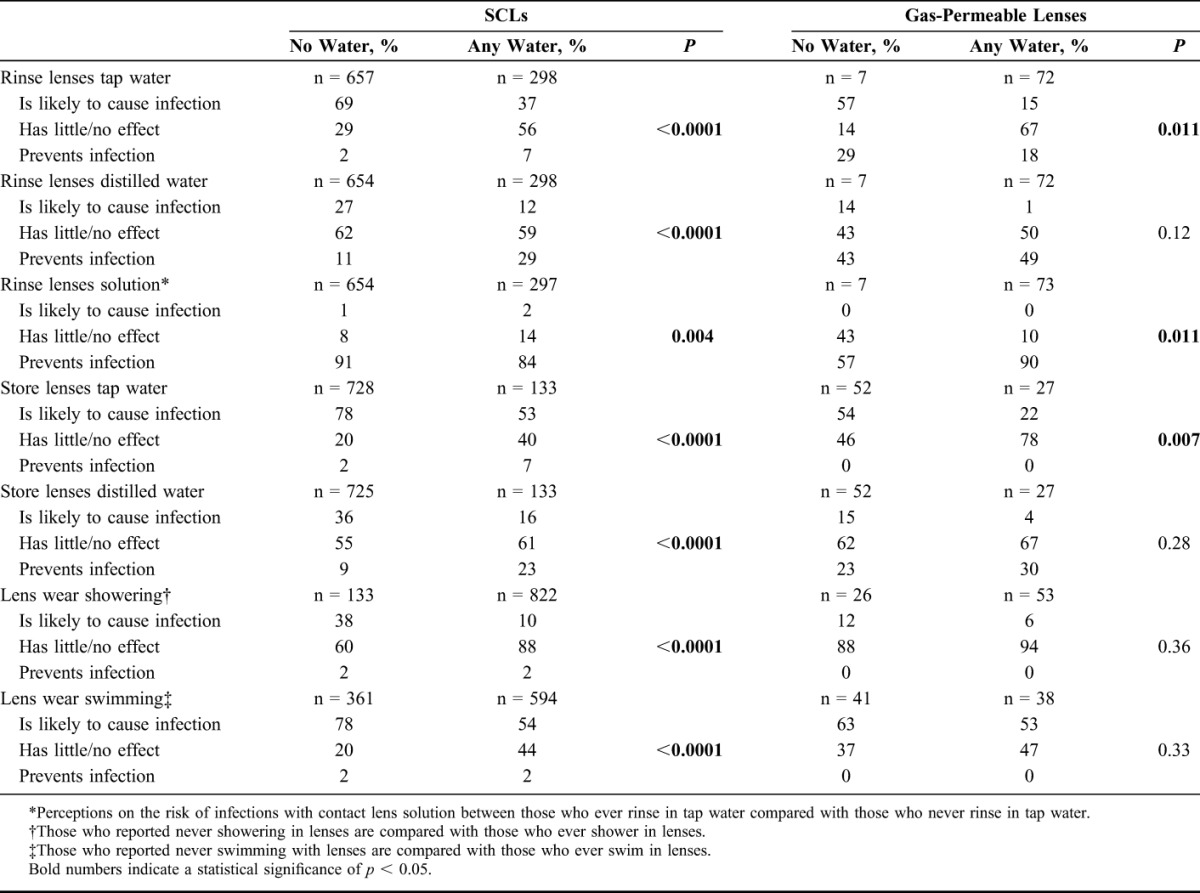
Among SCL wearers, those who reported lens exposure to water (rinsing, storing, showering, or swimming) perceived a lower risk of infection for each water-related behavior compared with those who never engaged in that particular behavior (all P < 0.0001) (Table 3). For GP lens wearers, participants who ever rinsed lenses with tap water (P = 0.011) or stored lenses in tap water (P = 0.007) perceived a lower risk of infection with those behaviors than those who did not have those behaviors.
Risk perception for rinsing lenses with tap water and storing lenses in tap water was compared by sex. For SCL wearers who ever rinsed lenses with tap water, men (11%) were more likely to perceive that this behavior prevents infection than did women who rinse lenses with tap water (6%) (P < 0.0001). Men who stored lenses in tap water were less likely than women to perceive that this behavior causes infection when they were SCL wearers (males 45%; females 57%) (P < 0.0001) or GP lens wearers (males 14%; females 25%) (P = 0.01).
DISCUSSION
This study showed a high level of lens exposure to water among contact lens wearers. It also found a significant number of contact lens wearers with incorrect perceptions about the risk of infection associated with these exposures. SCL wearers were more likely to expose their lenses to water indirectly by swimming and showering, whereas GP lens wearers were more likely to directly expose lenses to tap water through rinsing or storing of lenses. The latter is not surprising as GP lens wearers historically have received different lens care instructions than SCL wearers.
Most contact lens (CL) wearers reported showering while wearing lenses, and, among those who did, most perceived this practice as having little risk of developing an eye infection. In a separate study population that completed the CLRS, 75% of SCL wearers aged 12 to 33 reported showering with lenses more often than “some of the time,” and this behavior peaked at college age.17 Although exposure to water through showering is a plausible risk for infection, the increased risk for developing a contact lens-related adverse event due to showering while wearing lenses has not been established. Joslin et al19 postulated that because Acanthamoeba has been isolated from air, these microbes may aerosolize during showering, which openly exposes the contact lens and ocular surface. In the univariate analyses of 2 recent studies, showering was identified as a risk factor for CIEs20 and MK.21
Swimming with contact lenses was reported by most of the SCL wearers and many GP lens wearers, although with lower frequency (times per month) than showering with contact lenses. The participants who swam while wearing lenses did not perceive this to be a risky behavior. It has been shown that swimming with lenses can increase the bacterial bioburden on lenses22 and can expose the ocular surface to Acanthamoeba. Swimming has been identified as a likely factor for AK in GP lens wearers,23 orthokeratology wearers,24 frequent replacement SCL wearers,23 and daily disposable lens wearers.25 Avoiding contact lens wear while swimming is the safest practice; however, if one chooses to swim while wearing reusable contact lenses, a pair of tight-fitting goggles should be worn, thorough disinfection should occur in the evening,22 and patients should be educated to be alert for signs and symptoms of infection after swimming.
More troubling than swimming or showering while wearing contact lenses is direct contact of tap water to the lens surface by rinsing or storing. It is not surprising that GP lens wearers report rinsing their lenses with tap water, as most GP care systems include a step in which tap water is recommended for removing the lens cleaner.13 Not one SCL care system recommends rinsing SCLs with tap water; however, 10% of respondents reported always or fairly often rinsing their SCL with water. Although rinsing with tap water is included in GP lens care guidelines, there are several orthokeratology case reports, including some with children, in which tap water was used for rinsing or storing lenses and an AK event ultimately developed.26,27 Although lenses were exposed to water in these case reports, the role of overnight wear in orthokeratology cannot be readily dismissed.28 Although not statistically significant, a recent CDC case–control study of AK in GP lens wearers reported slightly increased risk of development of AK associated with rinsing GPs with water.29 Currently, there is no consensus among practitioners on the risk or benefit of the tap water rinse for GPs.30
Although no GP or SCL care system or contact lens care guidelines recommend storing lenses in water, we speculate that the rinsing step recommended for some GP solutions could confuse patients into thinking water is safe for storage. In this study, GP lens care brands were not recorded. Acanthamoeba is capable of adhering to hydrogels, GP lenses, polymethyl methacrylate (PMMA), and silicone hydrogels.31 Trophozoite adherence can occur in as little as 10 seconds, and the raw number of adhered microbes increases over time.32 Acanthamoeba trophozoites and cysts can adhere to all surfaces, although the cysts bind to a lesser extent than the trophozoites.33 Acanthamoeba adherence rates also differ among lens materials.31 If a water supply is contaminated with Acanthamoeba and the water is subsequently used for lens storage, then these microbes certainly are capable of adhering to a lens and case surface.
Exposure to any source of water while wearing contact lenses may increase the risk of an infectious10 or inflammatory event.18,20 Although treated recreational water (eg, pools) and most tap water are disinfected to prevent gastrointestinal illnesses, they are not sterile and contain bacteria,12 protozoans,7 and even fungi.34 Many of the organisms responsible for MK (eg, Acanthamoeba, Pseudomonas) grow in plumbing biofilms. These organisms can adhere to contact lenses and lens storage cases if the cases come into contact with contaminated tap water and are not properly cleaned and disinfected. The level of water contamination depends on the water source (untreated sources likely being more contaminated than treated sources), region,6 season,23 or after a rainfall. Water sources may vary in microbial load depending on the regulations specifying allowable disinfectants in water supplies.35
One method for decreasing the number of microbes in a supply of water is distillation. Distillation entails boiling the water, thereby killing microbes, including Acanthamoeba cysts.36 The resulting steam is then condensed, helping also to remove particulates. Both SCL and GP lens wearers collectively perceived that the use of distilled water for rinsing contact lenses or storing lenses is safer than using tap water. This perception can be misleading as there are other ways besides water for microbes to be introduced into the process; for example finger surfaces are contaminated with bacteria with or without hand washing,37 and eyelids and conjunctiva have a baseline bioburden,38 microbes of which can easily be transferred to a lens,39 or a storage case.40 If distilled water is used to rinse a lens, the only “disinfective” property of the water would be physical removal of microbes not tightly adhered to the lens surface. If distilled water is used for storage, then no disinfection of the lens or storage case occurs.
Regardless of reporting lens rinsing with tap water or not, over 40% of the SCL and GP lens wearers reported that they typically rinse their storage case with tap water. The contact lens storage case has been identified as a common fomite for developing MK.3,4 Exposing the storage case to tap water is a clear risk factor for developing AK,41 likely because water organisms that cause MK can adhere and grow in these cases. Seal et al asked participants who wear SCL daily to refrain from swimming with lenses, avoid using tap water for rinsing the lenses or storage cases, and to air dry their storage cases daily for a 1-month period. Although there was no mention of whether participants showered with lenses on or not, Acanthamoeba was not isolated from any storage case.41 Recently, Tilia et al found that rinsing storage cases with water also increased the likelihood of contamination with Gram-negative bacteria,42 specifically with Stenotrophomonas maltophilia, Delftia acidovorans, Achromobacter spp., Serratia marcescens, and Pseudomonas spp. These bacteria have been isolated from the lenses, storage cases, and ocular surfaces of patients with mild to severe corneal conditions.18,43 In addition, Wu et al40 found that allowing the storage case to air dry is associated with lower contamination rates than nonair dried cases. This suggests that eliminating storage case or lens tap water exposure can significantly reduce the likelihood of contaminating a contact lens with microbes.
In this study, among SCL wearers, men were more likely than women to report contact lens exposure to water through rinsing or storage and also perceived these behaviors with less risk. In a survey by Morgan et al44, women had better compliance with contact lens behaviors compared with men. In our study, it is difficult to draw definitive conclusions regarding differences between sexes as this sample was heavily weighted toward women.
This study may be limited by a sample that might not be representative of all CL wearers. As a convenience sample, it was mostly women, with no participants aged below 20 years, and included only a small sample of GP lens wearers. Future studies should also consider focus groups to further develop the most appropriate question/response options to understand patients' perceptions of risk.
In summary, water exposures among CL wearers are common. Rinsing lenses with tap water is particularly prevalent with GP lens wearers, possibly because of current care system guidelines. Contact lens users should never rinse soft lenses with tap water or store any type of lens in tap or distilled water, but many wearers reported practicing these behaviors. Practitioners need to better educate their patients to avoid exposing their lenses or storage case to any source of water. Likewise, manufacturers should continue to innovate lens care products that thoroughly disinfect and clean lenses while avoiding a tap water-rinsing step.
Footnotes
Supported in part by a grant from the Contact Lens Institute (CLI) to the Centers for Disease Control and Prevention. The CLRS was developed from research funding through an unrestricted grant from Alcon Laboratories Inc.
The authors have no conflicts of interest to disclose.
The findings and conclusions in this report are those of the authors and do not necessarily represent those of the Centers for Disease Control and Prevention or US Department of Health and Human Resources.
REFERENCES
- 1.Cope JR, Collier SA, Rao MM, et al. Contact lens wearer demographics and risk behaviors for contact lens-related eye Infections–United States, 2014. MMWR Morb Mortal Wkly Rep. 2015;64:865–870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Levy B, Heiler D, Norton S. Report on testing from an investigation of fusarium keratitis in contact lens wearers. Eye Contact Lens. 2006;32:256–261. [DOI] [PubMed] [Google Scholar]
- 3.Larkin DF, Kilvington S, Easty DL. Contamination of contact lens storage cases by Acanthamoeba and bacteria. Br J Ophthalmol. 1990;74:133–135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Stapleton F, Keay L, Edwards K, et al. The incidence of contact lens-related microbial keratitis in Australia. Ophthalmology. 2008;115:1655–1662. [DOI] [PubMed] [Google Scholar]
- 5.Dart JK, Saw VP, Kilvington S. Acanthamoeba keratitis: diagnosis and treatment update 2009. Am J Ophthalmol. 2009;148:487–499.e2. [DOI] [PubMed] [Google Scholar]
- 6.Radford CF, Minassian DC, Dart JK. Acanthamoeba keratitis in England and Wales: incidence, outcome, and risk factors. Br J Ophthalmol. 2002;86:536–542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Stockman LJ, Wright CJ, Visvesvara GS, et al. Prevalence of Acanthamoeba spp. and other free-living amoebae in household water, Ohio, USA–1990–1992. Parasitol Res. 2011;108:621–627. [DOI] [PubMed] [Google Scholar]
- 8.Sengor T, Kurna SA, Altun A, et al. Contact lens-related acanthamoeba keratitis and accompanying dacryoadenitis. Eye Contact Lens. 2015;41:204–209. [DOI] [PubMed] [Google Scholar]
- 9.Stehr-Green JK, Bailey TM, Brandt FH, et al. Acanthamoeba keratitis in soft contact lens wearers. A case-control study. JAMA. 1987;258:57–60. [PubMed] [Google Scholar]
- 10.Kilvington S, Gray T, Dart J, et al. Acanthamoeba keratitis: the role of domestic tap water contamination in the United Kingdom. Invest Ophthalmol Vis Sci. 2004;45:165–169. [DOI] [PubMed] [Google Scholar]
- 11.Wang JL, Chen ML, Lin YE, et al. Association between contaminated faucets and colonization or infection by nonfermenting gram-negative bacteria in intensive care units in Taiwan. J Clin Microbiol. 2009;47:3226–3230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Minogue E, Tuite NL, Smith CJ, et al. A rapid culture independent methodology to quantitatively detect and identify common human bacterial pathogens associated with contaminated high purity water. BMC Biotechnol. 2015;15:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Legarreta JE, Nau AC, Dhaliwal DK. Acanthamoeba keratitis associated with tap water use during contact lens cleaning: manufacturer guidelines need to change. Eye Contact Lens. 2013;39:158–161. [DOI] [PubMed] [Google Scholar]
- 14.US FDA. Contact lens risks. Available at: http://www.fda.gov/forconsumers/consumerupdates/ucm048893.htm. Accessed October 12, 2016.
- 15.Centers for Disease Control and Prevention. Water & contact lenses. Available at: http://www.cdc.gov/contactlenses/water-and-contact-lenses.html. Accessed October 12, 2016.
- 16.Yoder JS, Verani J, Heidman N, et al. Acanthamoeba keratitis: the persistence of cases following a multistate outbreak. Ophthalmic Epidemiol. 2012;19:221–225. [DOI] [PubMed] [Google Scholar]
- 17.Wagner H, Richdale K, Mitchell GL, et al. Age, behavior, environment, and health factors in the soft contact lens risk survey. Optom Vis Sci. 2014;91:252–261. [DOI] [PubMed] [Google Scholar]
- 18.Richdale K, Lam DY, Wagner H, et al. Case-control pilot study of soft contact lens wearers with corneal infiltrative events and healthy controls. Invest Ophthalmol Vis Sci. 2016;57:47–55. [DOI] [PubMed] [Google Scholar]
- 19.Joslin CE, Tu EY, Shoff ME, et al. The association of contact lens solution use and Acanthamoeba keratitis. Am J Ophthalmol. 2007;144:169–180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sorbara L, Zimmerman AB, Mitchell GL, et al. Multicenter testing of a risk assessment survey for soft contact lens wearers with adverse events: a contact lens assessment in youth study. Eye Contact Lens. In press. [DOI] [PubMed]
- 21.Lim CH, Carnt NA, Farook M, et al. Risk factors for contact lens-related microbial keratitis in Singapore. Eye. 2016;30:447–455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Choo J, Vuu K, Bergenske P, et al. Bacterial populations on silicone hydrogel and hydrogel contact lenses after swimming in a chlorinated pool. Optom Vis Sci. 2005;82:134–137. [DOI] [PubMed] [Google Scholar]
- 23.Radford CF, Lehmann OJ, Dart JK. Acanthamoeba keratitis: multicentre survey in England 1992-6. National Acanthamoeba Keratitis Study Group. Br J Ophthalmol. 1998;82:1387–1392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Arance-Gil A, Gutierrez-Ortega AR, Villa-Collar C, et al. Corneal cross-linking for Acanthamoeba keratitis in an orthokeratology patient after swimming in contaminated water. Cont Lens Anterior Eye. 2014;37:224–227. [DOI] [PubMed] [Google Scholar]
- 25.Kaji Y, Hu B, Kawana K, et al. Swimming with soft contact lenses: danger of acanthamoeba keratitis. Lancet Infect Dis. 2005;5:392. [DOI] [PubMed] [Google Scholar]
- 26.Robertson DM, McCulley JP, Cavanagh HD. Severe acanthamoeba keratitis after overnight orthokeratology. Eye Contact Lens. 2007;33:121–123. [DOI] [PubMed] [Google Scholar]
- 27.Watt K, Swarbrick HA. Microbial keratitis in overnight orthokeratology: review of the first 50 cases. Eye Contact Lens. 2005;31:201–208. [DOI] [PubMed] [Google Scholar]
- 28.Bullimore MA, Sinnott LT, Jones-Jordan LA. The risk of microbial keratitis with overnight corneal reshaping lenses. Optom Vis Sci. 2013;90:937–944. [DOI] [PubMed] [Google Scholar]
- 29.Cope JR, Collier SA, Schein OD, et al. Acanthamoeba keratitis among rigid gas permeable contact lens wearers in the United States, 2005 through 2011. Ophthalmology. 2016;123:1435–1441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hampton D, Tarver ME, Jacobs DS, et al. Special Commentary: Food and Drug Administration, American Academy of Ophthalmology, American Academy of Optometry, American Optometric Association and the Contact Lens Association of Ophthalmologists Cosponsored Workshop: Revamping Microbiological Test Methods for Contact Lenses, Products, and Accessories to Protect Health and Ensure Safety. Eye Contact Lens. 2015;41:329–333. [DOI] [PubMed] [Google Scholar]
- 31.Omana-Molina MA, Gonzalez-Robles A, Salazar-Villatoro L, et al. Silicone hydrogel contact lenses surface promote Acanthamoeba castellanii trophozoites adherence: qualitative and quantitative analysis. Eye Contact Lens. 2014;40:132–139. [DOI] [PubMed] [Google Scholar]
- 32.Kelly LD, Long D, Mitra D. Quantitative comparison of Acanthamoeba castellanii adherence to rigid versus soft contact lenses. CLAO J. 1995;21:111–113. [PubMed] [Google Scholar]
- 33.Kilvington S, Larkin DF. Acanthamoeba adherence to contact lenses and removal by cleaning agents. Eye. 1990;4:589–593. [DOI] [PubMed] [Google Scholar]
- 34.Kinsey GC, Paterson RR, Kelley J. Methods for the determination of filamentous fungi in treated and untreated waters. J Appl Microbiol. 1998;85(suppl 1):214S–24S. [DOI] [PubMed] [Google Scholar]
- 35.Joslin CE, Tu EY, McMahon TT, et al. Epidemiological characteristics of a Chicago-area Acanthamoeba keratitis outbreak. Am J Ophthalmol. 2006;142:212–217. [DOI] [PubMed] [Google Scholar]
- 36.Kilvington S. Moist-heat disinfection of Acanthamoeba cysts. Rev Infect Dis. 1991;13(suppl 5):S418. [DOI] [PubMed] [Google Scholar]
- 37.Ly VT, Simmons PA, Edrington TB, et al. Efficacy of hand washing procedures on bacterial contamination of hydrogel contact lenses. Optom Vis Sci. 1997;74:288–292. [DOI] [PubMed] [Google Scholar]
- 38.Dave SB, Toma HS, Kim SJ. Changes in ocular flora in eyes exposed to ophthalmic antibiotics. Ophthalmology. 2013;120:937–941. [DOI] [PubMed] [Google Scholar]
- 39.Mowrey-McKee MF, Sampson HJ, Proskin HM. Microbial contamination of hydrophilic contact lenses. Part II: quantitation of microbes after patient handling and after aseptic removal from the eye. CLAO J. 1992;18:240–244. [PubMed] [Google Scholar]
- 40.Wu YT, Willcox MD, Stapleton F. The effect of contact lens hygiene behavior on lens case contamination. Optom Vis Sci. 2015;92:167–174. [DOI] [PubMed] [Google Scholar]
- 41.Seal DV, Kirkness CM, Bennett HG, et al. Acanthamoeba keratitis in Scotland: risk factors for contact lens wearers. Cont Lens Anterior Eye. 1999;22:58–68. [DOI] [PubMed] [Google Scholar]
- 42.Tilia D, Lazon de la Jara P, Zhu H, et al. The effect of compliance on contact lens case contamination. Optom Vis Sci. 2014;91:262–271. [DOI] [PubMed] [Google Scholar]
- 43.Wiley L, Bridge DR, Wiley LA, et al. Bacterial biofilm diversity in contact lens-related disease: emerging role of Achromobacter, Stenotrophomonas, and Delftia. Invest Ophthalmol Vis Sci. 2012;53:3896–3905. [DOI] [PubMed] [Google Scholar]
- 44.Morgan PB, Efron N, Toshida H, et al. An international analysis of contact lens compliance. Cont Lens Anterior Eye. 2011;34:223–228. [DOI] [PubMed] [Google Scholar]


