Abstract
Objective
The objective of our pilot study was to evaluate the influence of daily phlebotomy on patients’ haemoglobin levels from our general intensive care unit.
Methods
We prospectively enrolled 35 patients who did not present with acute haemorrhage or developed it during the study period. For each patient we recorded: the diagnosis, age, sex, haemoglobin, hematocrit, SOFA and APACHE II score, blood volume drawn in standardized vials, number of blood tests ordered per day, fluid balance per day, number of ICU days. The collected data were analyzed using the linear regression model, paired t-test, receiver operating characteristic curves, and descriptive analysis. Statistical analysis was performed with SPSS v.17 trial version (IBM, NY, USA).
Results
The mean volume of blood drawn per day was 18.1 (SD ± 14.4) ml and the number of blood tests was 3.8 (SD ± 1.75) per day. On univariate linear regression analysis both the blood volume drawn daily (p = 0.04) and the number of blood tests per day (p = 0.009) correlated with a drop in mean haemoglobin concentration. The difference in the mean value of haemoglobin at admission and discharge correlated with overall mortality (p = 0.03). The sensitivity of admission haemoglobin equal to 10.6 g/dL in predicting mortality was 82.4% with a specificity of 50%, (p = 0.019, AUC = 0.732).
Conclusions
We evidenced the predictive power of blood sampling and number of blood tests done on haemoglobin concentration. Besides the main objective of the study we noticed that the difference in the mean value of haemoglobin at admission and discharge correlated with overall mortality. Considering that blood sampling contributes to anemia among ICU patients, we should limit the daily tests undertaken, to the tests absolutely necessary for guiding our therapy.
Keywords: anemia, haemoglobin, hematocrit, phlebotomy
Rezumat
Obiectiv
Acest studiu pilot a avut ca obiectiv stabilirea influenţei flebotomiei iatrogene asupra valorii hemoglobinei a pacienţilor critici din secţia noastră.
Metodă
Au fost înrolaţi prospectiv un număr de 35 de pacienţi care nu s-au prezentat la internare cu hemoragie sau au prezentat un episod hemoragic în timpul internării. Pentru fiecare pacient am documentat: diagnosticul, vârsta, sexul, hemoglobina şi hematocritul la internare, volumul de sânge recoltat în fiecare zi alături de numărul de recoltări, bilanţul hidric, numărul de zile de internare, scorul SOFA şi APACHE. Datele au fost analizate folosind modelul de regresie liniară, testul t, curbe ROC precum şi analiză statistică descriptivă. Softul folosit pentru analiza statistică a fost SPSS v.17 trial version (IBM, NY, USA).
Rezultate
Volumul mediu de sânge recoltat per zi a fost de 18,1 (SD ± 14,4) ml şi numărul de recoltări per zi a fost de 3,8 (SD ± 1,75). Folosind modelul de regresie liniară, atât volumul de sânge recoltat per zi (p = 0,04) cât şi numărul de recoltări per zi (p = 0,009) s-au corelat cu o scădere a valorii medii a hemoglobinei. Diferenţa între valoarea hemoglobinei la internare şi externare s-a corelat statistic cu mortalitatea (p = 0,03). Valoarea hemoglobinei la internare asociată cu o creştere a mortalităţii a fost de 10,6 g/dl având o specificitate de 50% şi sensibilitate 82,4% (p = 0,019, AUC = 73,2%).
Concluzii
Studiul de faţă demonstrează influenţa flebotomiei iatrogene asupra valorii hemoglobinei la pacienţii critici. În afara obiectivului primar al studiului valoarea hemoglobinei la internare s-a corelat cu o creştere a mortalităţii. Având în vedere numărul de recoltări per zi la pacienţii critici precum şi asocierea anemiei cu o mortalitate crescută, este necesară restricţia acestor teste la numărul minim necesar ghidării terapiei.
Introduction
Patients admitted to intensive care units are subject to frequent blood sampling for a variety of blood tests. This blood sampling can cause a drop in haemoglobin and hematocrit levels [1].
In this pilot study we sought to investigate the influence of blood sampling on haemoglobin levels in patients cared for in our general intensive care unit.
Material and method
With the approval of the University’s Ethics Committee, between April and September 2013 we prospectively included 35 patients aged between 18 to 87 years old, admitted to the ICU of Târgu Mureş Emergency County Hospital. Patients with active bleeding at admission (hemothorax, peritoneal or retroperitoneal haematoma, hemorrhagic stroke, epidural or subdural haematoma, gastrointestinal bleeding, blood loss with renal replacement therapy) and those who developed it during their ICU stay were excluded. Patients, who received medication that might influence the haemoglobin levels (erythropoietin, iron, vitamin B12, folic acid) or were admitted in the ICU for less than 2 days or over 25 days, were also excluded from the study.
We recorded for each patient included: the diagnosis, age, sex, haemoglobin (at admission and discharge), hematocrit (at admission and discharge), SOFA and APACHE II score, blood volume drawn in standardized vials, number of blood tests ordered per day, fluid balance per day, serum sodium and number of ICU days.
For each patient blood was drawn in standardized vials as follows: 6 ml vial for biochemistry tests, 2 ml for complete blood count, 5 ml for coagulation tests, 2 ml for acid base tests, 10 ml for blood culture tests and 5 ml for procalcitonin test. We also estimated a mean blood loss from the central vein catheterization of 5–10 ml for each sampling.
Statistical analysis
Descriptive statistics were used to characterize the patient population. The paired t test was used to evaluate the change in haemoglobin and hematocrit from admission to discharge. The independent t test was used to evaluate how the admission haemoglobin, hematocrit relates to mortality. Univariate and multivariate regression analysis was employed to determine the correlation between the mean haemoglobin concentration and the number of blood tests performed per day and the volume of blood drawn per day. Haemoglobin concentration determined at admission was also used to test the sensitivity and specificity in relation to overall mortality and reported by using receiver operating curve. We analyzed the data using the SPSS trial version 17 (IBM, NY, USA).
Results
Out of the 35 patients included in the study, 62.8% were males and 37.2% females. The average age of our population was 59 (SD ± 17.5) years with a range of 18–87 years.
Almost half of the patients (45.7%) were classified as medical and 54.2% as surgical. The mean SOFA score at admission was 8.2 (SD ± 4.6) and the mean APACHE II admission score was 18.1 (SD ± 8.4) with a mean ICU stay of 9.7 (SD ± 6.1) days, with a maximum of 25 ICU days (Table 1).
Table 1.
Summary of data
| Patients (n = 35) | Mean | Standard Deviation |
|---|---|---|
| Age | 59.4 | ± 17.5 |
| Male, % | 62.8 | |
| SOFA score | 8.2 | ± 4.6 |
| Apache II score | 18.1 | ± 8.4 |
| Haemoglobin on admission (g/dL) | 11.3 | ± 2.4 |
| Haemoglobin on discharge (g/dL) | 10.1 | ± 2.3 |
| Haemoglobin during ICU stay (g/dL) | 10.7 | ± 1.9 |
| Number of blood tests/day | 3.8 | ± 1.7 |
| Volume of blood loss/day (mL) | 18.1 | ± 14.4 |
| ICU length of stay (days) | 9.7 | ± 6.1 |
The mean value for haemoglobin at admission was 11.3 g/dL (SD ± 2.4) and the mean discharge value was 10.1 g/dL (SD ± 2.3) (Table 1).
The mean change in haemoglobin from admission to discharge was 1.18 g/dL (p = 0.007).
From all the blood tests done, 6.7% was attributed to blood cultures (mean 10.9 mL, SD ± 14), 14.8% to acid-base tests (mean 21.5 mL, SD ± 13.5), 28% to biochemistry (mean 41.7 mL, SD ± 24.7), 9.6% to complete blood count (mean 14.3 mL, SD ± 8.6), 21.7% to coagulation tests (mean 31.9 mL, SD ± 19.4), 1% to procalcitonin tests (mean 1.1 mL, SD ± 3) and 18.04% to vessel catheterization (mean 16.9 mL, SD ± 13.8) (Table 2).
Table 2.
Blood drawn per test
| Test | % | Mean | Standard Deviation |
|---|---|---|---|
| Complete Blood Count (mL) | 9.6 | 14.3 | ± 8.6 |
| Acid-base (mL) | 14.8 | 21.5 | ± 13.5 |
| Coagulation tests (mL) | 21.7 | 31.9 | ± 19.4 |
| Biochemistry (mL) | 28.0 | 41.7 | ± 24.7 |
| Blood cultures (mL) | 6.7 | 10.9 | ± 14.0 |
| Procalcitonin test (mL) | 1 | 1.1 | ± 3.0 |
| Central venous catheterization (mL) | 18 | 16.9 | ± 13.8 |
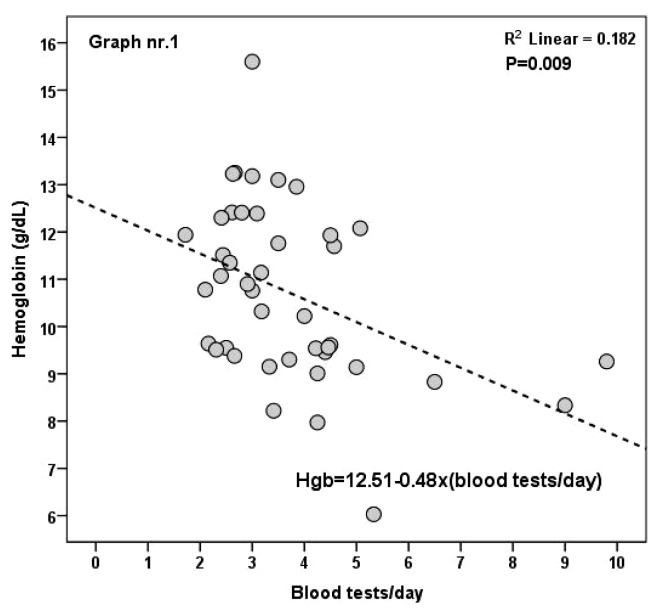
The mean volume of blood drawn per day was 18.1 (SD ± 14.4) ml and the mean number of blood tests were 3.8 (SD ± 1.75) per day (Table 1). On univariate linear regression analysis both the blood volume drawn per day (r = 0.12, p = 0.04) and number of blood tests per day (r = 0.182, p = 0.009) were correlated with a drop in mean haemoglobin concentration (Figure 1). For each ml of blood drawn the mean haemoglobin concentration dropped by 0.12 g/dL (extrapolated from the reference equation from the linear regression analysis Hb = 12.51–0.48 × number of blood tests per day).
Fig. 1.
Correlation between the number of blood tests per day and haemoglobin concentration
The difference in the mean value of haemoglobin at admission and discharge was correlated with overall mortality (p = 0.03). The mean difference in haemoglobin concentration (at admission and discharge) in survivors was 0.35 g/dL compared to a mean difference in non-survivors of 2.04 g/dL.
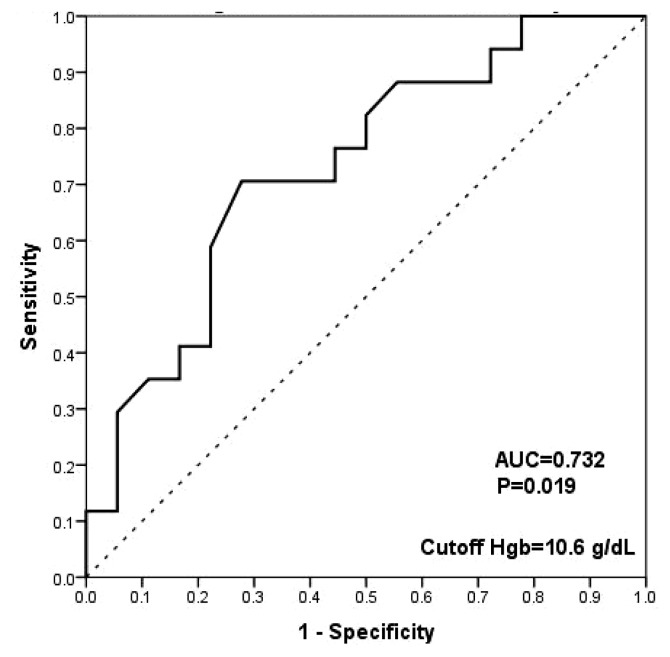
The mean value of haemoglobin at admission was also correlated with overall mortality (p = 0.019). The sensitivity of admission haemoglobin level equal to 10.6 g/dL (value determined using the Youden Index) in predicting mortality was 82.4% with a specificity of 50%, AUC = 0.732 (area under the curve) (Figure 2).
Fig. 2.
ROC: Haemoglobin at admission and mortality. ROC – Receiver operating characteristic, AUC – area under curve
Discussion
Anemia and blood transfusions in the ICU are associated with organ dysfunction, increased mortality, and a longer ICU length of stay. The SOAP study reported, in 1136 patients, a positive correlation between organ dysfunction and the number of blood draws (r = 0.34; p < 0.001) and the total volume drawn (r = 0.28; p < 0.001), about 41 ml/day/patient and approximately 280 ml per week from ventilated patients [2].
Considering that frequent blood sampling enhances the impact of anemia on the critically ill patient in ICU, our results showed similar and were in agreement with those results and also with a multicenter study that emphasize the effect of anemia on ICU mortality [3].
Compared to a retrospective study conducted at Toronto General Hospital’s medical wards which included 404 patients, our mean blood volume drawn was larger, for routine labs (18.1 mL vs 10 mL) [1]. This difference could be explained by a more frequent phlebotomy for routine labs in critically ill patients.
A study which included 17 676 patients with acute myocardial infarction from 57 US hospitals reported a mean daily blood drawn per day of 21.1 mL, just above our 18.1 mL per day. In the same study the mean blood volumes drawn per diagnostic test were: for ABG (arterial blood gas) analysis their mean blood volume drawn was 18.3 mL compared to our value of 21.5 mL; for serum biochemistry it was 69.9 mL opposed to our value of 41.6 mL and this difference is best explained by supplementary diagnostic tests required for acute myocardial infarction. For the coagulation and haematology tests their reported mean values for blood drawn were 26.6 mL and 47.4 mL opposed to our values of 31.8 mL and 14.2 mL. In their study the daily blood loss for diagnostic tests was independently associated with a higher risk of hospital acquired anemia and they concluded that blood drawn per test using paediatric vials could limit sampling blood loss [4].
In a study on blood loss from phlebotomy, in 70 renal patients, Pabla et al. reported a mean blood loss per week of 55.7 mL, mean admission haemoglobin of 9.84 g/dL and a mean discharge haemoglobin of 9.51 g/dL. Their reported mean difference in haemoglobin at admission and discharge was lower, 0.33 g/dL than our finding of 1.2 g/dL, because of lower rates of iatrogenic phlebotomy and a lower blood volume drawn per test (local protocol driven) [5].
A study carried in a medical hospital with 113 beds, recorded the entire blood collected from all the patients within a 1 week period. They found that the amount of blood recorded proved to be a mean of 45 times the required volume of specimen (range, 2 to 102 times), and underlined the consecutive risk of anemia and infections, and supplementary costs [6].
Multiple pathogenic mechanisms contribute to the development of anaemia in critically ill patients: reduced red blood cell life span, decreased production of erythropoietin and marrow response, decrease in plasma iron concentrations and efforts must be made for blood conservation [7]. Whether blood sampling was the only responsible factor for the differences in haemoglobin values in our pilot study, it is not clear, but it was certainly a contribution to anemia enhancement.
Conclusion
The results of this pilot study emphasize the predictive power of blood sampling and number of blood tests done, on haemoglobin concentration. Besides the main objective of the study we noticed that the difference in the mean value of haemoglobin at admission and discharge correlated with overall mortality, in studied patients. Considering that blood sampling contributes to anemia among ICU patients, we should limit the daily unnecessary tests undertaken.
Footnotes
Conflict of interest
Nothing to declare
References
- 1.Thavendiranathan P, Bagai A, Ebidia A, Detsky AS, Choudhry NK. Do blood tests cause anemia in hospitalized patients? The effect of diagnostic phlebotomy on hemoglobin and hematocrit levels. J Gen Intern Med. 2005;20:520–524. doi: 10.1111/j.1525-1497.2005.0094.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Vincent JL, Baron JF, Reinhart K, Gattinoni L, Thijs L, Webb A, et al. Anemia and blood transfusion in critically ill patients. JAMA. 2002;288:1499–1507. doi: 10.1001/jama.288.12.1499. [DOI] [PubMed] [Google Scholar]
- 3.Corwin HL, Gettinger A, Pearl RG, Fink MP, Levy MM, Abraham E, et al. The CRIT Study: Anemia and blood transfusion in the critically ill – current clinical practice in the United States. Crit Care Med. 2004;32:39–52. doi: 10.1097/01.CCM.0000104112.34142.79. [DOI] [PubMed] [Google Scholar]
- 4.Salisbury AC, Reid KJ, Alexander KP, Masoudi FA, Lai SM, Chan PS, et al. Diagnostic blood loss from phlebotomy and hospital-acquired anemia during acute myocardial infarction. Arch Intern Med. 2011;171:1646–1653. doi: 10.1001/archinternmed.2011.361. [DOI] [PubMed] [Google Scholar]
- 5.Pabla L, Watkins E, Doughty HA. A study of blood loss from phlebotomy in renal medical inpatients. Transfus Med. 2009;19:309–314. doi: 10.1111/j.1365-3148.2009.00960.x. [DOI] [PubMed] [Google Scholar]
- 6.Dale JC, Pruett SK. Phlebotomy – a minimalist approach. Mayo Clin Proc. 1993;68:249–255. doi: 10.1016/s0025-6196(12)60044-5. [DOI] [PubMed] [Google Scholar]
- 7.Page C, Retter A, Wyncoll D. Blood conservation devices in critical care: a narrative review. Ann Intensive Care. 2013;3:14. doi: 10.1186/2110-5820-3-14. [DOI] [PMC free article] [PubMed] [Google Scholar]