Abstract
Objective
The Eating Disorder Examination (EDE) was originally developed and validated in primarily white female samples. Since data indicate that eating pathology impacts black youth, elucidating the psychometric appropriateness of the EDE for black youth is crucial.
Method
A convenience sample was assembled from seven pediatric obesity studies. The EDE was administered to all youth. Confirmatory factor analyses (CFA) were conducted to examine the original four-factor model fit and two alternative factor structures for black and white youth. With acceptable fit, multiple-group CFAs were conducted. For measurement invariant structures, the interactive effects of race with sex, BMIz, adiposity, and age were explored (all significance levels p<.05).
Results
For both black and white youth (N=820; 41% black; 37% male; 6–18y; BMIz -3.11–3.40), the original four-factor EDE structure and alternative eight-item one-factor structure had mixed fit via CFA. However, a seven-item, three-factor structure reflecting Dietary Restraint, Shape/Weight Overvaluation, and Body Dissatisfaction had good fit and held at the level of strict invariance. Girls reported higher factor scores than boys. BMIz and adiposity were positively associated with each subscale. Age was associated with Dietary Restraint and Body Dissatisfaction. The interactional effects between sex, BMIz, and age with race were not significant; however, the interaction between adiposity and race was significant. At higher adiposity, white youth reported greater pathology than black youth.
Conclusion
An abbreviated seven-item, three-factor version of the EDE captures eating pathology equivalently across black and white youth. Full psychometric testing of the modified EDE factor structure in black youth is warranted.
Keywords: Eating Disorder Examination (EDE), factor structure, invariance, children, adolescents, black, race
The Eating Disorder Examination (EDE)1 is a semi-structured interview that is widely used for the assessment of eating pathology.2 It is generally considered a reliable and valid measure of eating attitudes and behaviors3 and has been used extensively in clinical research settings.(e.g.,4–7) Initially validated in adult patients with anorexia and bulimia nervosa,8 the EDE has subsequently been examined among adult individuals across the eating disorder spectrum, in those with overweight and obesity, and in community samples.5 The EDE has also been used in child and adolescent samples,9–11 and a child version was developed in 199612 and validated by several groups.12–15
Consistent with most psychological assessment instruments,16 the EDE has been developed and validated within primarily non-Hispanic white female populations.(e.g.,1,8,12,13) This is problematic because data demonstrate that eating and weight pathology are reported by other ethnic and racial groups, and important differences may exist in the presentation and manifestation of eating pathology.17 The presence and prevalence of eating pathology in the non-Hispanic black population is especially critical to elucidate, given that traditional risk factors for eating pathology (e.g., body dissatisfaction and internalization of the thin ideal) are significantly less pronounced for non-Hispanic black youth compared to white youth.18–20 Yet, there are no significant differences in the lifetime prevalence of anorexia nervosa in nationally representative samples of non-Hispanic black and non-Hispanic white populations.17,21 Non-Hispanic black youth and adults may even have a higher lifetime prevalence of bulimia nervosa compared to non-Hispanic white children and adults.17,21 Such findings may be due to the influence of the dominant culture’s beauty ideals and resulting acculturative stress and body dissatisfaction.22,23 Moreover, studies suggest that relative to non-Hispanic white populations, binge-eating disorder appears to be at least as prevalent in non-Hispanic black populations.17,21,24 Non-Hispanic black youth and adults have a significantly higher lifetime prevalence of sub-clinical binge eating behaviors compared to non-Hispanic white youth and adults.17,21 Indeed, data obtained from the EDE indicate that non-Hispanic black youth report equal rates of binge and loss of control eating as non-Hispanic white youth.25
Although eating pathology has been examined in racially heterogeneous samples,26 it is unknown whether the measures used to assess eating disorder pathology function similarly for non-Hispanic black and non-Hispanic whiteψ youth.27 One approach to help determine whether a measure functions similarly for both groups is by examining measurement invariance. Measurement invariance holds when there is no systematic error biased against a certain group;28 that is, if black and white youth have identical levels of eating pathology, they are equally likely to endorse related items regardless of group membership. Notably, other measures of eating pathology have been found to lack invariance for black and white adults,29 but to our knowledge there are no data on measures for pediatric samples. Given that eating disturbance typically develops adolescence, but can also manifest during middle childhood,21 elucidating the measurement invariance of the EDE across races is important in order to reliably and validly identify those with eating pathology. It is also crucial for cross-cultural research,30 as we seek to better understand disturbed eating in minority populations. Measurement invariance of the EDE in black and white youth is a necessary step to ensure that comparisons between groups are valid and interpretations meaningful.
To this end, we studied the measurement invariance of the EDE in a large sample of black and white children and adolescents. Three separate factor structures proposed in the adult and pediatric literature were examined. The first was the original EDE four-factor solution, which includes 22 items and four subscales: Restraint, Eating Concern, Weight Concern, and Shape Concern.1,12 The second was an eight-item, one-factor solution comprised primarily of weight and shape items.5,9,31 The third was a seven-item, three-factor solution comprised of Dietary Restraint, Shape/Weight Overvaluation, and Body Dissatisfaction subscales.4,32 Because the EDE was developed to assess symptomology specific to eating disorders1 that should apply similarly to both black and white youth, we hypothesized that the individual EDE factor structures would be similar for both races.
METHOD
Participants
A convenience sample was assembled from children and adolescents enrolled in seven studies on eating behaviors and obesity at the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) and the Uniformed Services University of the Health Sciences (USUHS) in the United States. Participants were 820 boys and girls from non-treatment studies (ClinicalTrials.gov ID: NCT00320177, n=77; NCT00631644, n=156; NCT00001195, n=133; and NCT00001522, n=184), excess weight gain prevention studies (NCT00263536, n=15; NCT00680979, n=101), and a treatment study for those with a body mass index (BMI, kg/m2) at or above the 95th percentile with at least one obesity-related comorbidity (e.g., diabetes; NCT00001723, n=154) enrolled from 1999 through 2015. Individuals were included if they were administered either the original EDE for adults or the child version of the EDE1,12 at a screening or baseline visit. Additionally, individuals were included if parents reported the child’s race as “black” or “white” and the child’s ethnicity as “non-Hispanic.” Children of other races, multiple races, or Hispanic ethnicity were excluded. Any participant enrolled in the studies prior to 1999, when we began administering the EDE, was excluded. For all studies other than NCT00001723, for which an obesity-related medical condition was required for inclusion, youth were excluded for major psychiatric or medical diagnoses, medications affecting weight, pregnancy, current involvement in weight loss treatment programs, or greater than 5% weight loss within 3 months of assessment. In addition, for the intervention studies, individuals currently in psychotherapy or weight loss treatment were excluded. Participants were recruited through the National Institutes of Health (NIH) clinical trials website, posters at physician offices, direct mailings to homes within a 50-mile radius of Bethesda, Maryland, and flyers within the local community. All studies were approved by the NICHD institutional review board (IRB); NCT00680979 and NCT00631644 were also approved by the USUHS IRB. Written consent and assent were provided by parents and children, respectively.
Procedures
Participants were seen at the NIH Hatfield Clinical Research Center. All data were collected at screening or baseline visits, before the initiation of any treatment.
Measures
Eating Disorder Examination (EDE)
The EDE version 12OD/C.21 and the child version12 are semi-structured interviews designed to assess disordered eating attitudes and behaviors, and are similar except the script for the child version was adapted to make it more accessible for a younger audience.33 The adult version was has been examined in children as young as eight years,34 and the child version in youth as young as six years.9,31 No maximum age range exists for either version, though psychometric properties of the child version have only been examined in youth up to 16 years of age.9 In the current study, 94.5% of youth 15 years and older were administered the adult version. Over 99% of youth under 12 years were administered the child version. The adult and child version have successfully been combined in previous analyses.7,35,36 There are four clinically derived subscales assessing disordered eating attitudes: Restraint (5 items), Eating Concern (5 items), Weight Concern (5 items), and Shape Concern (8 items). A global score is generated as the average of the four subscales. However, recent data suggest experimentally derived factor structures provide better fit.4,5,31,32 Additional questions assessing behavioral symptoms (i.e., binge eating and compensatory behaviors) are used clinically, but are not included in subscale or global scores.1 Internal consistency for the EDE subscales differ by sample and can range from poor to excellent; however, Shape Concern typically garners the highest consistency across subscales.3,31 Interrater reliability is generally good.3,13,37 Concurrent and discriminant validity are generally adequate,3,31,37 but vary by subscale and population of interest.3,37 In the current study, all EDEs were administered by trained clinical interviewers evidencing good interrater reliability (intraclass correlations .87 to .99, ps<.01) as previously described.35,38
Body composition
Height and fasting weight were measured in triplicate using calibrated electronic instruments. BMI was calculated as weight in kilograms divided by the square of height in meters. BMIz was calculated according to the Centers for Disease Control and Prevention 2000 growth charts.39 Body fat mass (kg) was measured by dual-energy x-ray absorptiometry (DXA) (Hologic, Bedford, MA, USA) or air displacement plethysmography (Bod Pod; Life Measurement Inc., Concord, CA, USA). As in prior studies,40 measurements of fat mass were adjusted to account for known differences in the two assessment techniques.41
Statistical Analyses
Descriptive statistics, internal consistency, and analyses of variance (ANOVA) were conducted with SPSS 22.0 (IBM Statistics, Armonk, NY). Confirmatory factor analyses (CFA) and multi-group analyses were analyzed using Mplus 7.0 (Muthen & Muthen, Los Angeles, CA). Cronbach’s alpha was used to determine estimated internal consistency and was considered satisfactory at α = 0.70 or above.42 CFAs were conducted with robust weighted least squares mean- and variance-adjusted (WLSMV) estimation, which is appropriate for ordinal data.43 Model fit for the four-factor1,12 and abbreviated one-5,9,31 and three-factor4,32 models were examined separately for each racial group prior to invariance testing.44 Model fit was assessed with the Comparative Fit Index (CFI), Tucker-Lewis Index (TLI), Root Mean Square Error of Approximation (RMSEA), and chi-square (χ2). The following values were used to indicate good model fit: CFI>.95, TLI>.95, and RMSEA≤.06.45 The chi-square statistic was also examined; however, it is highly influenced by sample size. With larger sample sizes, chi-square tends to be statistically significant, indicating poor model fit;46,47 therefore more emphasis was given to other estimates of model fit. Adequate fit of a given model in each racial group was a prerequisite for measurement invariance testing of that particular model. That is, if the CFA models conducted separately within both racial groups met acceptable fit criteria for a given factor structure, multi-group CFAs were then examined44 using a nested model approach from least to most restrictive to evaluate measurement invariance across race.
The first step (i.e., least restrictive, fully unconstrained model) in the multi-group CFA was configural invariance, where all model parameters were free to vary across groups. The second step was metric (or weak) invariance, where the factor loadings were constrained to be equal across groups. If metric invariance was met, the factor structure of the EDE would be considered the same for both black and white youth, and the association between a given EDE item and its latent factor would be the same for black and white youth. For example, if endorsing the item “Empty Stomach” was as strongly associated with scores on the Restraint scale for both black and white youth, it would be indicative of metric invariance across race for this item. The third step was scalar (or strong) invariance, where factor loadings and item intercepts were constrained across groups. Scalar invariance is necessary to compare black and white youths’ group means on the EDE. The final step was strict invariance, where factor loadings, item intercepts, and residual variances were constrained to be equal across groups. Strict invariance is often considered too stringent and often unobtainable in practice,48 but it is included for completeness.
Nested models were compared using the change in CFI values and the DIFFTEST function in Mplus, which is the chi-square difference test for WLSMV estimation. The null hypothesis for the chi-square difference test was that the models being compared were the same; therefore, when p>.05, we did not reject the null hypothesis and chose the more constrained model over the less constrained model. The criterion for change in CFI was .01 (i.e., when ΔCFI between the less constrained and more constrained models ≤.01, we would not reject the null hypothesis based on the recommendation of Cheung),49 and was more highly regarded in evaluating model fit given that the chi-square difference test is sensitive to sample size, often resulting in significant findings for larger sample sizes.49 Finally, if the invariance models held at the level of scalar invariance, BMIz, fat mass, and age were centered at their respective means, and the main and interactional effects of race with sex, BMIz, fat mass (adjusting for age, sex, and centered height in centimeters), and age were explored with ANOVAs. Relationships and differences were considered significant when p values were ≤.05.
RESULTS
Eight-hundred-twenty children and adolescents (40.88% black, 37.44% male) ages 6 to 18 years were studied (Table 1). BMI z-scores ranged from −3.11 to 3.40 (45.5% obese). Black and white youth did not differ on age or sex; however, black youth had significantly higher BMIz and fat mass compared to white youth. The majority of youth were administered the adult version of the EDE (64.8%; Mage=15.08, SDage=1.49), and the remainder were assessed with the child version (Mage=11.18, SDage=2.28).
Table 1.
Participant Demographics
| Total Sample (N=820) | Black (n=335) | White (n=485) | p | |
|---|---|---|---|---|
| Girls (%) | 62.6 | 65.1 | 60.8 | .22 |
| Sex (% male) | 37.44 | 34.93 | 39.18 | .22 |
| Age (years; M ± SD) | 13.70 ± 2.60 | 13.65 ± 2.63 | 13.74 ± 2.58 | .69 |
| BMIz (M ± SD) | 1.29 ± 1.16 | 1.64 ± 1.09 | 1.05 ± 1.15 | < .001 |
| Fat Mass (kg; M ± SD) | 28.34 ± 20.53 | 34.22 ± 23.00^ | 24.48 ± 17.73^ | < .001 |
Note.
= Adjusted for height, age, and sex.
Internal Consistency
Cronbach’s alpha values for the original four EDE subscales,1,12 the EDE global score,1,12 and the abbreviated one-5,9,31 and three-factor4,32 scales were consistent across races and for the whole group (Table 2). For the original four-factor structure,1,12 internal consistency was less than satisfactory for the Restraint and Eating Concern subscales, but satisfactory for the Weight Concern subscale, Shape Concern subscale, and global score for both racial groups. The brief eight-item scale5,9,31 evidenced satisfactory internal consistency for both racial groups. Internal consistency was less than satisfactory for the seven-item three-factor structure4,32 Dietary Restraint subscale, but satisfactory for the Shape/Weight Overvaluation and Body Dissatisfaction subscales for both racial groups.
Table 2.
Internal Consistency Reliabilities (Cronbach’s Alpha) for the Full and Abbreviated EDE Scales
| EDE | Total Sample (N=820) | Blacks (n=335) | Whites (n=485) |
|---|---|---|---|
| Original Four-Factor | |||
| Restraint | .58 | .56 | .60 |
| Eating Concern | .61 | .55 | .66 |
| Weight Concern | .74 | .71 | .75 |
| Shape Concern | .86 | .85 | .87 |
| Global Score | .91 | .90 | .91 |
|
| |||
| Eight-Item, One-Factor | .88 | .87 | .90 |
|
| |||
| Seven-Item, Three-Factor | |||
| Dietary Restraint | .65 | .61 | .68 |
| Shape/Weight Overvaluation | .84 | .85 | .83 |
| Body Dissatisfaction | .86 | .83 | .88 |
Note. EDE = Eating Disorder Examination
Invariance Analyses
The measurement models by race are presented in Table 3. The fit of the original four-factor structure1,12 was good for white youth, but mixed for black youth as the RMSEA was out of the acceptable range. The abbreviated one-factor structure,5,9,31 with an a priori residual covariance between two items - importance of weight and importance of shape,31 was good for black youth, but mixed for white youth as the RMSEA was out of the acceptable range. Given these results, multi-group CFAs were not examined for the original factor structure1,12 or for the abbreviated one-factor structure.5,9,31
Table 3.
Fit Indices by Race for the Full and Abbreviated EDE Scales
| Goodness-of-fit statistics | ||||||
|---|---|---|---|---|---|---|
|
|
||||||
| Model | χ2 | df | p | CFI | TLI | RMSEA |
| Original Four-Factor | ||||||
| Black | 485.00 | 202 | < .001 | .957 | .950 | .065 |
| White | 530.92 | 202 | < .001 | .976 | .973 | .058 |
|
| ||||||
| Eight-Item, One-Factor | ||||||
| Black | 82.98 | 19 | < .001 | .995 | .993 | .053 |
| White | 36.66 | 19 | .009 | .993 | .989 | .083 |
|
| ||||||
| Seven-Item, Three-Factor | ||||||
| Black | 12.69 | 11 | .31 | .999 | .999 | .021 |
| White | 27.59 | 11 | .004 | .997 | .994 | .056 |
Note. EDE = Eating Disorder Examination; CFI = comparative fit index; TLI = Tucker-Lewis index; RMSEA = root-mean-square error of approximation
The measurement model for the abbreviated three-factor, seven-item structure4,32 was acceptable for both groups, and all items loaded well on their respective factors; therefore, multi-group testing was conducted. All fit indices are presented in Table 4. The configural invariance model fit was good across groups, although, as anticipated given the large sample size, the chi-square was significant. The metric invariance model constrained factor loadings and, based on the change in CFI, the more constrained metric invariance model was chosen as optimal given the ΔCFI was less than .01. The scalar invariance model was assessed next and evidenced good model fit. The ΔCFI from the metric invariance model to the scalar invariance model was acceptable. However, as expected given the sample size, the chi-square difference test was significant. Strict invariance was assessed as the final step, and the model evidenced good fit. The ΔCFI from the scalar invariance model to the strict invariance model was acceptable. However, the chi-square difference test remained significant. The strict invariance model for the three-factor, seven-item structure4,32 was, therefore, considered the final, most acceptable level of model fit.
Table 4.
Summary of Measurement Invariance of the Abbreviated Three-Factor EDE Scale Across Race
| Invariance Model: Constraints | χ2 (df) | DIFFTESTχ2 (df) | CFI | ΔCFI | TLI | RMSEA [90% CI] |
|---|---|---|---|---|---|---|
| Configural: None | 75.66 (41)*** | .996 | .995 | .045 [.029, .061] | ||
| Metric: Factor loadings | 90.02 (45)*** | 12.87 (4)* | .994 | .002 | .995 | .049 [.034, .064] |
| Scalar: Factor loadings, item intercepts | 117.96 (58)*** | 38.57 (13)*** | .992 | .002 | .994 | .050 [.037, 063] |
| Strict: Factor loadings, item intercepts, residual variances | 136.15 (65)*** | 19.85 (7)** | .991 | .001 | .994 | .052 [.039, .064] |
Note. EDE = Eating Disorder Examination; DIFFTEST = chi-square for difference testing with robust weighted least squares mean- and variance-adjusted estimation; CFI = comparative fit index; TLI = Tucker-Lewis index; RMSEA = root-mean-square error of approximation; CI = confidence interval
p < .05,
p < .01,
p < .001
Relationships with Demographic Characteristics
Most omnibus ANOVAs were significant with main effects of sex, BMIz, fat mass, or age (Table 5). Girls reported significantly higher Dietary Restraint (M=1.21, SD=1.41), Shape/Weight Overvaluation (M=1.98, SD=1.71), and Body Dissatisfaction (M=1.94, SD=1.74) than boys (M=0.69, SD=1.16; M=1.44, SD=1.53; M=0.95, SD=1.40, respectively; ps<.001). Higher BMIz and fat mass were associated with greater Dietary Restraint, Shape/Weight Overvaluation, and Body Dissatisfaction scores (ps<.001). Age was positively associated with Dietary Restraint, Shape/Weight Overvaluation, and Body Dissatisfaction (ps<.01).
Table 5.
Main and Interaction Effects of Race and Demographic Characteristics for Subscales of the Abbreviated Three-Factor EDE Scale
| Variables | Dietary Restraint | Shape/Weight Overvaluation | Body Dissatisfaction | |||
|---|---|---|---|---|---|---|
|
| ||||||
| B | SE B | B | SE B | B | SE B | |
| Race | 0.00 | 0.12 | 0.20 | 0.15 | 0.06 | 0.15 |
| Sex | −0.55*** | 0.12 | −0.42** | 0.15 | −0.97*** | 0.15 |
| Race × Sex | 0.09 | 0.20 | −0.30 | 0.25 | −0.05 | 0.24 |
| F (df) | 9.70 (3, 818)*** | 7.52 (3, 808)*** | 23.62 (3, 814) *** | |||
|
| ||||||
| Race | −0.20* | 0.09 | −0.19 | 0.12 | −0.34** | 0.11 |
| BMIz | 0.48*** | 0.05 | 0.53*** | 0.06 | 0.84*** | 0.06 |
| Race × BMIz | −0.07 | 0.08 | 0.00 | 0.10 | −0.14 | 0.09 |
| F (df) | 47.06 (3, 816)*** | 39.69 (3, 806)*** | 101.41 (3, 812)*** | |||
|
| ||||||
| Race | −0.16 | 0.11 | −0.10 | 0.13 | −0.29* | 0.12 |
| Fat Mass | 0.03*** | 0.00 | 0.04*** | 0.01 | 0.03*** | 0.00 |
| Height | 0.00 | 0.00 | 0.00 | 0.01 | 0.00 | 0.01 |
| Sex | −0.42*** | 0.11 | −0.35** | 0.13 | −0.84*** | 0.12 |
| Race × Fat Mass | −0.01* | 0.01 | −0.01* | 0.01 | −0.03*** | 0.01 |
| F (df) | 19.44 (5, 635)*** | 20.10 (5, 628)*** | 58.27 (5, 633)*** | |||
|
| ||||||
| Race | 0.06 | 0.10 | 0.12 | 0.12 | 0.10 | 0.12 |
| Age | 0.11*** | 0.02 | 0.09 | 0.03** | 0.13*** | 0.03 |
| Race × Age | −0.06 | 0.04 | −0.03 | 0.05 | −0.04 | 0.05 |
| F (df) | 8.17 (3, 816)*** | 4.10 (3, 806)** | 8.51 (3, 812)*** | |||
Note. EDE = Eating Disorder Examination; Dummy coding was entered as follows: Race - White = 0, Black = 1, Sex - Girls = 0, Boys = 1; BMIz, fat mass, age, and height were centered at their respective means.
p < .05;
p < .01;
p < .001.
The interactional effects of race were not significant for age, sex, or BMIz. However, there were significant interactions of race by fat mass for each of the EDE subscales. At lower fat mass, scores were similar for white and black youth; but at higher fat mass, subscale scores were significantly higher for white youth compared to black youth (Figure 1).
Figure 1. Race by Fat Mass Interactions for the (A) Dietary Restraint, (B) Shape/Weight Overvaluation, and (C) Body Dissatisfaction Subscales of the Three-Factor Structure.
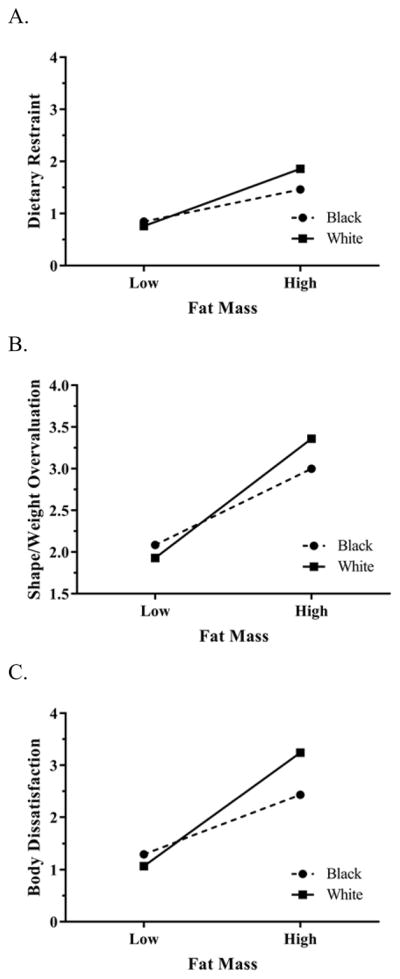
A. There were significant race by fat mass interactions (adjusting for age, sex, and height) for the Dietary Restraint factor of the seven-item, three-factor structure. At lower fat mass, scores were similar for whites and blacks; but at higher fat mass, scores were significantly higher for white youth compared to black youth (p < .05).
B. There were significant race by fat mass interactions (adjusting for age, sex, and height) for the Shape/Weight Overvaluation factor of the seven-item, three-factor structure. At lower fat mass, scores were similar for whites and blacks; but at higher fat mass, scores were significantly higher for white youth compared to black youth (p < .05).
C. There were significant race by fat mass interactions (adjusting for age, sex, and height) for the Body Dissatisfaction factor of the seven-item, three-factor structure. At lower fat mass, scores were similar for whites and blacks; but at higher fat mass, scores were significantly higher for white youth compared to black youth (p < .001).
Follow-Up Analyses by Non-Intervention and Intervention Groups
The data for black and white youth were combined, and post-hoc CFAs were conducted for each of the factor structures in both non-intervention (n=551) and intervention (n=271) groups. Findings were similar to those for black and white youth the four-factor1,12 and one-factor5,9,31 model evidenced mixed fit, while the three-factor model4,32 evidenced good fit for both non-intervention and intervention groups. Specifically, the four-factor model1,12 had mixed fit for the non-intervention group (χ2 (202)=895.07, p<.001; CFI=.94; TLI=.93; RMSEA=.08) as the RMSEA was out of acceptable range, and did not converge for the intervention group. The one-factor eight-item model5,9,31 had mixed fit for both groups with the RMSEA out of acceptable range (non-intervention: (χ2 (19)=67.39, p<.001; CFI=.99; TLI=.99; RMSEA=.07; intervention: (χ2 (19)=45.77, p<.001; CFI=.99; TLI=.98; RMSEA=.07). The three-factor seven-item model4,32 evidenced good fit for both groups (non-intervention: (χ2 (11)=25.99, p<.01; CFI=.99; TLI=.99; RMSEA=.05; intervention: (χ2 (11)=10.06, p>.05; CFI=1.00; TLI=1.00; RMSEA<.001).
Follow-Up Analyses by EDE Adult and Child Versions
Using the combined data from black and white youth, post-hoc CFAs were conducted for each of the factor structures for the adult (n=531) and child (n=289) versions. The four-factor model1,12 had mixed fit for the adult version as the RMSEA was out of acceptable range (χ2 (202)=662.50, p<.001; CFI=.96; TLI=.96; RMSEA=.07); however, the child version evidenced good fit (χ2 (202)=358.60, p<.001; CFI=.98; TLI=.97; RMSEA=.05). The one-factor eight-item model5,9,31 had mixed fit for the adult version with the RMSEA out of acceptable range (χ2 (19)=77.25, p<.001; CFI=.99; TLI=.99; RMSEA=.08); however, the child version evidenced good fit: (χ2 (19)=31.21, p<.05; CFI=1.00; TLI=1.00; RMSEA=.05). The three-factor seven-item model4,32 evidenced good fit for both versions (adult: (χ2 (11)=21.97, p<.05; CFI=1.00; TLI=1.00; RMSEA=.04; child: (χ2 (11)=19.84, p<.05; CFI=1.00; TLI=.99; RMSEA=.05).
DISCUSSION
This study examined whether the EDE was structurally equivalent across black and white youth. Three factor structures evident in the current literature were examined: the original twenty-two item four-factor structure consisting of Restraint, Eating Concern, Weight Concern, and Shape Concern subscales,1,12 a brief eight-item one-factor structure consisting of primarily weight and shape items,5,9,31 and a seven-item three-factor structure consisting of Dietary Restraint, Shape/Weight Overvaluation, and Body Dissatisfaction subscales.4,32 Of the three factor structures examined, only the seven-item three-factor structure4,32 evidenced good fit for both races and had evidence for strict invariance signifying measurement equivalence for both black and white youth. In other words, the abbreviated three-factor model4,32 measured the construct of eating pathology similarly regardless of race and despite differences (and similarities) in eating pathology prevalence.
The abbreviated three-factor model4,32 maps on to components of the original structure.1,12 The Dietary Restraint subscale of the three-factor model4,32 contains three items from the original structure’s1,12 Restraint subscale: restraint over eating, food avoidance, and dietary rules.4 The Shape/Weight Overvaluation subscale includes the two importance items4 from the original factor structure’s1,12 Shape Concern and Weight Concern subscales. Similarly, the Body Dissatisfaction subscale includes the two dissatisfaction items4 from the original factor structure’s1,12 Shape Concern and Weight Concern subscales. Only items in the Eating Concern subscale of the original four-factor structure (e.g., eating in secret, fear of losing control over eating)1,12 are not included in the abbreviated model.
Identification that a seven-item, three-factor structure4,32 EDE functions similarly across black and white youth is important. First, there are discrepant levels of certain risk factors for eating pathology (e.g., body dissatisfaction, thin-ideal internalization) across races, and this factor structure assesses eating pathology equivalently for both black and white youth.18–20 Using an assessment that effectively captures eating pathology will elucidate the manifestation of eating problems in black youth. Moreover, it will ultimately help to inform intervention approaches. Indeed, accurately elucidating the behaviors and attitudes that reflect eating pathology in this group is crucial to effectively targeting and treating eating disturbance. Second, the measurement invariance allows for group means to be appropriately compared between black and white youth. This will allow for a more meaningful understanding and comparison of disordered eating attitudes and behaviors in youth from different racial backgrounds.
The lack of fit for the original four-factor EDE model is informative, but expected, given that the original four domains of the EDE (i.e., Restraint, Eating Concern, Shape Concern, and Weight Concern) were clinically derived.1,12 With one exception,10 empirically derived factor analyses from a variety of sample populations have not been able to replicate the clinically derived four-factor structure.4–6,9 Our findings and the lack of support for the four-factor model3 in adult and child populations from various racial and ethnic backgrounds caution use of the original four-factor structure1,12 for comparison of means across black and white youth with sub-diagnostic eating pathology. It is possible that these structures may be assessing different constructs for black and white youth, though replication and expansion to eating disorder populations is warranted. Nevertheless, despite the EDE’s original testing in individuals with anorexia nervosa and bulimia nervosa,8 over the last ten years research making use of EDE in samples of individuals with obesity has increased considerably. This is perhaps due the rise in obesity over the past several decades,50,51 and the associations between bulimia nervosa and binge-eating disorder with obesity.52,53 Given this, it is important to understand how the utility of this widely-used interview fares with those at the higher end of the weight spectrum.
In addition to the seven-item, three-factor4,32 structure’s measurement invariance across race, the pattern of internal consistency reliabilities for the three subscales was similar for both black and white youth. The reliability for Shape/Weight Overvaluation and Body Dissatisfaction were high, but not for Dietary Restraint. This discrepancy may reflect a broader conceptual problem of dietary restraint within the EDE that 1) includes both cognitive and behavioral restraint and 2) may not distinguish between healthy, flexible levels of restraint and more rigid restraint indicative of eating pathology.50 Even in the original four-factor structure,1,12 the Restraint subscale was less effective at distinguishing between women with bulimia and restricting controls and between women with binge-eating disorder and overweight controls than it was for distinguishing between women with anorexia and bulimia nervosa and normal weight controls.3 In addition, in samples of youth enriched for overweight, the Restraint subscale of the original four-factor structure did not distinguish between youth with and without disordered eating.7 Participants in the current study were enriched for overweight, but not for full-syndrome eating disorders across the weight spectrum. Thus, it is possible that dietary restraint in this population is more variable than what would be expected in clinical populations. However, it also possible that the measurement of restraint may need further adjustment to adequately distinguish amongst groups with varying levels of restraint.
The three-factor structure4,32 performed well overall in both racial groups and functioned in a manner consistent with extant research on eating pathology and sex, BMIz, fat mass, and age.51 Accordingly, girls reported higher scores than boys on Dietary Restraint, Shape/Weight Overvaluation, and Body Dissatisfaction. BMIz, fat mass, and age were positively associated with each factor. In line with trends in the United States,52,53 black youth were heavier than white youth. Consistent with research demonstrating that black individuals tend to have lower body dissatisfaction than white individuals,18–20 Body Dissatisfaction was significantly associated with race in the BMIz and fat mass models. Nevertheless, the significant interactions between fat mass and race for each subscale provide preliminary evidence for similar levels of pathology at lower fat mass and more discrepant levels of pathology at higher fat mass. Specifically, though both groups reported greater eating pathology when they had higher versus lower fat mass, white youth with higher fat mass reported significantly greater eating pathology than black youth with higher fat mass. This is consistent with research showing cultural differences in internalization of the thin ideal, with the drive for thinness being less culturally salient for black girls.54,55 It is also consistent with research indicating greater body acceptance for black individuals compared to white individuals.18–20 However, it is important to note that the interactions were statistically significant but may not be clinically meaningful as the magnitudes of the differences between races were small, particularly for Dietary Restraint and Shape/Weight Overvaluation.
Strengths of the current study include a large sample size with similar percentages of black and white participants assessed by interviewers with rigorous training in conducting the EDE.35,38 In addition, anthropometric measurements such as height, weight, and fat mass were objectively measured, and participants from across the weight and age spectrum were included. The latter improves generalizability of findings to black and white children and adolescents. However, findings are limited by the convenience samples, which by original study designs, were enriched for participants with overweight, but not for those meeting diagnostic criteria for eating disorders. Thus, we cannot extend our findings to patients with anorexia nervosa or bulimia nervosa. Though some of our sample endorsed binge eating, very few met criteria for binge-eating disorder. Therefore, it would be presumptive to extend the findings to those with binge-eating disorder. It is also possible that the slightly different inclusion/exclusion criteria from the original studies, such as treatment-seeking vs. non-treatment-seeking, could impact results. Though we found that intervention status did not moderate results, the studies may have criteria that limit generalizability. For instance, results may vary in other geographic areas, particularly outside of the United States. In addition, measurement invariance is only one step in the psychometric assessment of a measure. The current study does not provide evidence of the predictive validity of the modified structure in youth. In addition, one could argue the use of the adult and child versions of the EDE might be a limitation versus a strength of the current study. Finally, although widely used in psychological research, the racial groups “black” and “white” are simplifications of quite heterogeneous racial populations.59 Nevertheless, the current study provides preliminary evidence of the measurement invariance of the EDE in commonly classified racial groups.
Future research should seek to replicate the current findings in samples of youth with full-syndrome eating disorders and a range of pathologies. Furthermore, prospective data are needed to determine the predictive validity of a three-factor, seven-item EDE4,32 in black and white youth to determine its utility in the identification of eating pathology and response to treatment in comparison to other published factor structures. The current findings provide evidence of the three-factor structure’s stability in both the adult and child versions of the EDE, which likely serve as proxies for the factor structure’s stability across ages. Nevertheless, age and sex could also be examined separately for measurement invariance of the abbreviated three-factor structure.4,32 Finally, corroboration of the EDE’s invariance in youth from different racial and ethnic groups (e.g., Asian, Hispanic) is required. Evidence of the three-factor4,32 structure’s psychometric and predictive properties across racial and ethnic groups will be important not only in the context of conducting research that measures eating pathology across groups effectively, but also in understanding how the EDE can best be used in clinical settings with increasingly diverse populations.
Acknowledgments
Research Support: NIH Intramural Research Program Grant 1ZIAHD000641 (J. Yanovski) from NICHD with supplemental funding from the NIH Bench to Bedside Program and the Office of Behavioral and Social Sciences Research; NIDDK 1R01DK080906 (to MTK), USUHS grant R072IC (to MTK).
Footnotes
“Non-Hispanic black” and “non-Hispanic white” will be abbreviated to “black” and “white” throughout the remainder of the manuscript for brevity.
Disclaimers: None of the authors has a conflict of interest. J. Yanovski is a commissioned officer in the U.S. Public Health Service (PHS). The opinions and assertions expressed herein are those of the authors and are not to be construed as reflecting the views of the PHS, HHS, USUHS or the U.S. Department of Defense.
References
- 1.Fairburn CG, Cooper Z. The Eating Disorder Examination. In: Fairburn CG, Wilson GT, editors. Binge eating: Nature, assessment, and treatment. 12. New York, NY: Guilford Press; 1993. pp. 317–360. [Google Scholar]
- 2.Guest T. Using the Eating Disorder Examination in the assessment of bulimia and anorexia: Issues of reliability and validity. Soc Work Health Care. 2000;31(4):71–83. doi: 10.1300/J010v31n04_05. [DOI] [PubMed] [Google Scholar]
- 3.Berg KC, Peterson CB, Frazier P, Crow SJ. Psychometric evaluation of the eating disorder examination and eating disorder examination-questionnaire: A systematic review of the literature. Int J Eat Disord. 2012;45(3):428–438. doi: 10.1002/eat.20931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Grilo CM, Crosby RD, Peterson CB, et al. Factor Structure of the Eating Disorder Examination Interview in Patients With Binge-eating Disorder. Obesity. 2010;18(5):977–981. doi: 10.1038/oby.2009.321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Byrne SM, Allen KL, Lampard AM, Dove ER, Fursland A. The factor structure of the eating disorder examination in clinical and community samples. Int J Eat Disord. 2010;43(3):260–265. doi: 10.1002/eat.20681. [DOI] [PubMed] [Google Scholar]
- 6.Mannucci E, Ricca V, Di Bernardo M, Moretti S, Cabras PL, Rotella CM. Psychometric properties of EDE 12.0D in obese adult patients without binge eating disorder. Eat Weight Disord. 1997;2(3):144–149. doi: 10.1007/BF03339965. [DOI] [PubMed] [Google Scholar]
- 7.Tanofsky-Kraff M, Goossens L, Eddy KT, et al. A multisite investigation of binge eating behaviors in children and adolescents. J Consult Clin Psychol. 2007;75(6):901–913. doi: 10.1037/0022-006X.75.6.901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cooper Z, Cooper PJ, Fairburn CG. The validity of the eating disorder examination and its subscales. Br J Psychiatry. 1989;154(6):807–812. doi: 10.1192/bjp.154.6.807. [DOI] [PubMed] [Google Scholar]
- 9.Wade TD, Byrne S, Bryant-Waugh R. The eating disorder examination: Norms and construct validity with young and middle adolescent girls. Int J Eat Disord. 2008;41(6):551–558. doi: 10.1002/eat.20526. [DOI] [PubMed] [Google Scholar]
- 10.O’Brien A, Watson HJ, Hoiles KJ, et al. Eating disorder examination: Factor structure and norms in a clinical female pediatric eating disorder sample. Int J Eat Disord. 2015;49(1):107–110. doi: 10.1002/eat.22478. [DOI] [PubMed] [Google Scholar]
- 11.Couturier J, Lock J, Forsberg S, Vanderheyden D, Yen HL. The addition of a parent and clinician component to the eating disorder examination for children and adolescents. Int J Eat Disord. 2007;40(5):472–475. doi: 10.1002/eat.20379. [DOI] [PubMed] [Google Scholar]
- 12.Bryant-Waugh R, Cooper PJ, Taylor CL, Lask BD. The use of the eating disorder examination with children: A pilot study. Int J Eat Disord. 1996;19(4):391–397. doi: 10.1002/(SICI)1098-108X(199605)19:4<391::AID-EAT6>3.0.CO;2-G. [DOI] [PubMed] [Google Scholar]
- 13.Watkins B, Frampton I, Lask B, Bryant-Waugh R. Reliability and validity of the child version of the eating disorder examination: A preliminary investigation. Int J Eat Disord. 2005;38(2):183–187. doi: 10.1002/eat.20165. [DOI] [PubMed] [Google Scholar]
- 14.Hilbert A, Buerger A, Hartmann AS, Spenner K, Czaja J, Warschburger P. Psychometric evaluation of the eating disorder examination adapted for children. Eur Eat Disord Rev. 2013;21(4):330–339. doi: 10.1002/erv.2221. [DOI] [PubMed] [Google Scholar]
- 15.Frampton I, Wisting L, Overas M, Midtsund M, Lask B. Reliability and validity of the Norwegian translation of the Child Eating Disorder Examination (ChEDE) Scand J Psychol. 2011;52(2):196–199. doi: 10.1111/j.1467-9450.2010.00833.x. [DOI] [PubMed] [Google Scholar]
- 16.Dana RH, Aponte JF, Wohl J. Psychological assessment in the diagnosis and treatment of ethnic group members. Needham Heights, MA: Allyn & Bacon; 2000. [Google Scholar]
- 17.Marques L, Alegria M, Becker AE, et al. Comparative prevalence, correlates of impairment, and service utilization for eating disorders across US ethnic groups: Implications for reducing ethnic disparities in health care access for eating disorders. Int J Eat Disord. 2011;44(5):412–420. doi: 10.1002/eat.20787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Roberts A, Cash TF, Feingold A, Johnson BT. Are black-white differences in females’ body dissatisfaction decreasing? A meta-analytic review. J Consult Clin Psychol. 2006;74(6):1121–1131. doi: 10.1037/0022-006X.74.6.1121. [DOI] [PubMed] [Google Scholar]
- 19.Franko DL, Striegel-Moore RH. The role of body dissatisfaction as a risk factor for depression in adolescent girls: are the differences Black and White? J Psychosom Res. 2002;53(5):975–983. doi: 10.1016/s0022-3999(02)00490-7. [DOI] [PubMed] [Google Scholar]
- 20.Ruiz SY, Pepper A, Wilfley D. Obesity and body image among ethnically diverse children and adolescents. In: Thompson JK, editor. Handbook of eating disorders and obesity. Hoboken, New Jersey: John Wiley & Sons, Inc; 2004. pp. 656–678. [Google Scholar]
- 21.Swanson SA, Crow SJ, Le Grange D, Swendsen J, Merikangas KR. Prevalence and correlates of eating disorders in adolescents. Results from the national comorbidity survey replication adolescent supplement. Arch Gen Psychiatry. 2011;68(7):714–723. doi: 10.1001/archgenpsychiatry.2011.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Taylor JY, Caldwell CH, Baser RE, Faison N, Jackson JS. Prevalence of eating disorders among Blacks in the National Survey of American Life. Int J Eat Disord. 2007;40(Suppl):S10–14. doi: 10.1002/eat.20451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Perez M, Voelz ZR, Pettit JW, Joiner TE., Jr The role of acculturative stress and body dissatisfaction in predicting bulimic symptomatology across ethnic groups. Int J Eat Disord. 2002;31(4):442–454. doi: 10.1002/eat.10006. [DOI] [PubMed] [Google Scholar]
- 24.Striegel-Moore RH, Wilfley DE, Pike KM, Dohm FA, Fairburn CG. Recurrent binge eating in black American women. Arch Fam Med. 2000;9(1):83–87. doi: 10.1001/archfami.9.1.83. [DOI] [PubMed] [Google Scholar]
- 25.Cassidy OL, Matheson B, Osborn R, et al. Loss of control eating in African-American and Caucasian youth. Eat Behav. 2012;13(2):174–178. doi: 10.1016/j.eatbeh.2012.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.George JBE, Franko DL. Cultural Issues in Eating Pathology and Body Image Among Children and Adolescents. J Pediatr Psychol. 2010;35(3):231–242. doi: 10.1093/jpepsy/jsp064. [DOI] [PubMed] [Google Scholar]
- 27.Cassidy O, Sbrocco T, Tanofsky-Kraff M. Utilizing non-traditional research designs to explore culture-specific risk factors for eating disorders in African American adolescents. Adv Eat Disord. 2015;3(1):91–102. doi: 10.1080/21662630.2014.948470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kline RB. Principles and practice of structural equation modeling. 4. Guilford publications; 2015. [Google Scholar]
- 29.Kelly NR, Mitchell KS, Gow RW, et al. An evaluation of the reliability and construct validity of eating disorder measures in white and black women. Psychol Assess. 2012;24(3):608–617. doi: 10.1037/a0026457. [DOI] [PubMed] [Google Scholar]
- 30.Milfont TL, Fischer R. Testing measurement invariance across groups: Applications in cross-cultural research. International Journal of psychological research. 2015;3(1):111–130. [Google Scholar]
- 31.Jongenelis MI, Byrne SM, Pettigrew S, Allen KL, Watt F. A psychometric examination of a modified eight-item version of the Children’s Eating Disorder Examination. Psychol Assess. 2014;26(1):267–276. doi: 10.1037/a0034803. [DOI] [PubMed] [Google Scholar]
- 32.Grilo CM, Reas DL, Hopwood CJ, Crosby RD. Factor structure and construct validity of the Eating Disorder Examination-Questionnaire in college students: further support for a modified brief version. Int J Eat Disord. 2015;48(3):284–289. doi: 10.1002/eat.22358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Tanofsky-Kraff M, Shomaker LB, Olsen C, et al. A prospective study of pediatric loss of control eating and psychological outcomes. J Abnorm Psychol. 2011;120(1):108–118. doi: 10.1037/a0021406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Berg KC, Swanson SA, Stiles-Shields EC, Eddy KT, Peterson CB, Grange DL. Response patterns on interview and questionnaire versions of the Eating Disorder Examination and their impact on latent structure analyses. Compr Psychiatry. 2013;54(5):506–516. doi: 10.1016/j.comppsych.2012.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Glasofer DR, Tanofsky-Kraff M, Eddy KT, et al. Binge eating in overweight treatment-seeking adolescents. J Pediatr Psychol. 2007;32(1):95–105. doi: 10.1093/jpepsy/jsl012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Shomaker LB, Tanofsky-Kraff M, Elliott C, et al. Salience of loss of control for pediatric binge episodes: does size really matter? Int J Eat Disord. 2010;43(8):707–716. doi: 10.1002/eat.20767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Allison DB, Baskin ML, editors. Handbook of assessment methods for eating behaviors and weight-related problems: Measures, theory, and research. 2. Los Angeles: Sage Publications, Inc; 2009. [Google Scholar]
- 38.Tanofsky-Kraff M, Yanovski SZ, Wilfley DE, Marmarosh C, Morgan CM, Yanovski JA. Eating-Disordered Behaviors, Body Fat, and Psychopathology in Overweight and Normal-Weight Children. J Consult Clin Psychol. 2004;72(1):53–61. doi: 10.1037/0022-006X.72.1.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kuczmarski RJ, Ogden CL, Guo SS, et al. 2000 CDC Growth Charts for the United States: methods and development. Vital Health Stat. 2002;11(246):1–190. [PubMed] [Google Scholar]
- 40.Shomaker LB, Tanofsky-Kraff M, Young-Hyman D, et al. Psychological symptoms and insulin sensitivity in adolescents. Pediatr Diabetes. 2010;11(6):417–423. doi: 10.1111/j.1399-5448.2009.00606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Robotham DR, Schoeller DA, Mercado AB, et al. Estimates of body fat in children by Hologic QDR-2000 and QDR-4500A dual-energy X-ray absorptiometers compared with deuterium dilution. J Pediatr Gastroenterol Nutr. 2006;42(3):331–335. doi: 10.1097/01.mpg.0000189373.31697.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bland JM, Altman DG. Statistics notes: Cronbach’s alpha. BMJ. 1997;314:572. doi: 10.1136/bmj.314.7080.572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Brown TA. Confirmatory Factor Analysis for Applied Research. Vol. 2. New York, NY: The Guilford Press; 2015. [Google Scholar]
- 44.Meade AW, Johnson EC, Braddy PW. Power and sensitivity of alternative fit indices in tests of measurement invariance. J Appl Psychol. 2008;93(3):568–592. doi: 10.1037/0021-9010.93.3.568. [DOI] [PubMed] [Google Scholar]
- 45.Hu Lt, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct Equ Modeling. 1999;6(1):1–55. [Google Scholar]
- 46.Bentler PM, Bonnet DG. Significance tests and goodness of fit in the analysis of covariance structures. Psychol Bull. 1980;88:588–606. [Google Scholar]
- 47.Jöreskog KG, Sörbom D. LISREL 8: Structural equation modeling with the SIMPLIS command language. Chicago, IL: Scientific Software International; 1993. [Google Scholar]
- 48.Millsap RE, Meredith W. Factorial Invariance: Historical Perspectives and New Problems. In: Cudeck R, MacCallum RC, editors. Factor analysis at 100: Historical developments and future directions. Mahwah, NJ: Lawrence Erlbaum Associates; 2007. pp. 131–152. [Google Scholar]
- 49.Cheung GW, Rensvold RB. Evaluating Goodness-of-Fit Indexes for Testing Measurement Invariance. Struct Equ Modeling. 2002;9(2):233–255. [Google Scholar]
- 50.Haynos AF, Field AE, Wilfley DE, Tanofsky-Kraff M. A novel classification paradigm for understanding the positive and negative outcomes associated with dieting. Int J Eat Disord. 2015;48(4):362–366. doi: 10.1002/eat.22355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Thompson JK. Handbook of eating disorders and obesity. Hoboken, N.J: John Wiley & Sons; 2004. [Google Scholar]
- 52.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA. 2014;311(8):806–814. doi: 10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Ogden CL, Carroll MD, Lawman HG, et al. Trends in obesity prevalence among children and adolescents in the United States, 1988–1994 through 2013–2014. JAMA. 2016;315(21):2292–2299. doi: 10.1001/jama.2016.6361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Cassidy O, Sbrocco T, Vannucci A, et al. Adapting interpersonal psychotherapy for the prevention of excessive weight gain in rural African American girls. J Pediatr Psychol. 2013;38(9):965–977. doi: 10.1093/jpepsy/jst029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Cassidy O, Eichen DM, Burke NL, et al. Adapting interpersonal psychotherapy for the prevention of excessive weight gain: Considerations for urban African American girls. 2016 doi: 10.1093/jpepsy/jst029. Manuscript submitted for publication. [DOI] [PMC free article] [PubMed] [Google Scholar]


