Fig. 2.
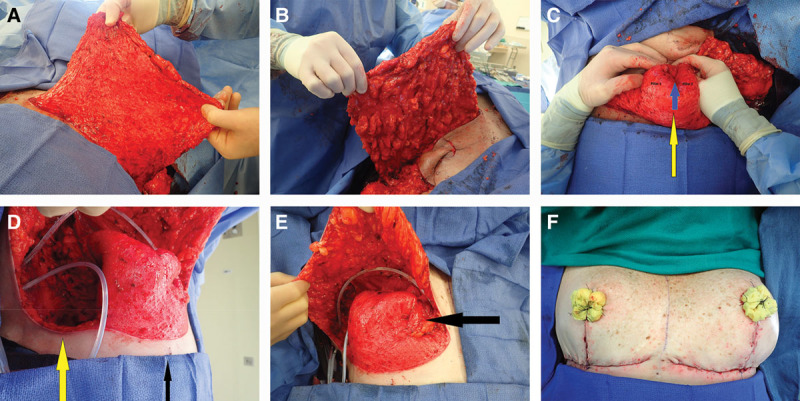
A, B The deepithelialized inferior mastectomy flap that forms the bulk of the reconstructed breast mound is shown. To maximize the amount of volume available for reconstructing a breast mound centered on the meridian, we find it useful to divide the dermis in the inframammary fold laterally, leaving two-thirds connected medially, allowing for medial tissue transfer (demonstrated in a subsequent panel). C, Demonstrates how we reconstruct the breast mound. The inferior dermal flap is folded in half along a transverse axis creating a double thickness flap. This folded flap is then folded again on itself along the vertical meridian (yellow arrow) creating 2 pillars. At this point, we use a 2-0 absorbable suture to stabilize the reconstructed breast mound by suturing the 2 pillars to each other at the base near the inframammary fold (IMF). We continue the interrupted suturing superiorly to the apex of the reconstructed mound (blue arrow demonstrates apical suture). We also suture this reconstructed mound to the pectoralis major muscle. We typically choose a point 6 to 7 cm above the IMF as the most superior point on the pectoralis, where we suture the mound in place. This will position the bulk of the tissue near the IMF, where we want it, to maximize lower pole fullness and nipple projection. D, Demonstrates the division of the inferior mastectomy flap in the lateral one-third at the IMF (yellow arrow). We then transfer this tissue at the lateral IMF as far medially as possible—up, over, and partially behind the reconstructed breast mound—and suture it to a parasternal location, which provides additional projection, height, and medial fullness. E, This transposition results in transfer of tissue from the most lateral point on the IMF to the most medial point in the newly reconstructed breast mound (black arrow at parasternal location was previously located at the far lateral IMF). F, The Wise flaps are closed over the breast mound with additional projection provided by the tissue between the vertical limbs, which is finally followed by NAC grafting. Note the asymmetry between the breasts that often results after a cancer resection (right) and prophylactic mastectomy (left).
