Abstract
In this case report, we demonstrate that the use of a winged expandable cage was able to obtain good clinical and radiological results in a case of cervical tuberculosis with severe kyphosis. However, case series will be necessary to affirm its validity as a stand-alone device for similar cases with high risk of instability.
Keywords: Cervical tuberculosis, winged expandable cage, spondylodiscitis
Introduction
The use of winged expandable titanium cages (WETC) following single or multiple cervical corpectomy for the treatment of different diseases has been proposed as an alternative to other cervical reconstructive techniques as autologous bone graft (ABG), non-expandable titanium cages (NETC) and expandable titanium cages (ETC). We recently reported (1) good results in a series of patients treated for cervical spondylosis using WETC after single or multiple corpectomy. Herein we report a case of cervical tuberculosis with severe kyphosis treated with this device. Cervical alignment was restored, the patient fully recovered in 2 weeks and post-operative radiological imaging showed good results in terms of stability.
Case presentation
We describe the case of a 44-year-old Nigerian ambassador who used travel to foreign countries for work duties reporting a recent journey in Africa. He presented to our emergency department since affected by severe cervical pain from about 2 weeks. Full blood tests were normal, white cell blood counts, C-reactive protein (CRP), erythrocyte sedimentation rate (ESR) and serum alkaline phosphatase were within the ranges. He did not report history of smoke, alcohol or drug and no previous infection or operation. Neurological examination was unremarkable. Cervical radiograph showed C4 and C5 vertebral height loss associated to severe cervical kyphosis (Figure 1). Spondylodiscitis was suspected and cervical MRI demonstrated inflammatory tissue at C4-C5 with vertebral body erosion and pre-vertebral abscess (Figure 2). Work-up for tuberculosis was negative and thoracic radiograph was normal. Nevertheless, due to the clinical indolent course of infection and destructive behavior, tubercular spondylodiscitis was suspected and the standard four-drug therapy was started [isoniazid (5 mg/kg), rifampicin (10 mg/kg) ethambutol (15 mg/kg) and pyrazinamide (25 mg/kg)] with the plan to operate the patient after a partial or total resolution of the infection. In the following days, the patient complained uncontrollable pain so we proceeded to a pre-vertebral abscess evacuation followed by C4-C5 corpectomy with insertion of a WETC. Standard left-side anterior cervical approach was executed. Before the insertion of the WETC abundant wash-out, curettage of the inflammatory tissue and careful preparation of the adjacent endplates were executed. Histological examination and microbiological investigation including bacterial, fungal, and mycobacterial stains and culture were taken. In post-operative period, the patient wore Philadelphia collar and post-operative imaging showed good results in terms of kyphosis reduction (Figure 3). Tissue examination revealed granuloma formation and polymerase chain reaction (PCR) for Mycobacterium Tuberculosis in tissues was positive. Intravenous antibiotics were continued and the patient fully recovered in about 2 weeks. Cervical radiographs at 2, 4, 8 and 12 weeks from the operation showed the stability of the device, maintenance of cervical alignment and no subsidence. Cervical MRI executed at 2 months demonstrated resolution of the inflammatory process (Figure 4).
Figure 1.

Cervical radiograph demonstrated C4-C5 vertebral bodies collapse.
Figure 2.
Cervical MRI showed the presence of prevertebral abscess and C4-C5 spondylodiscitis.
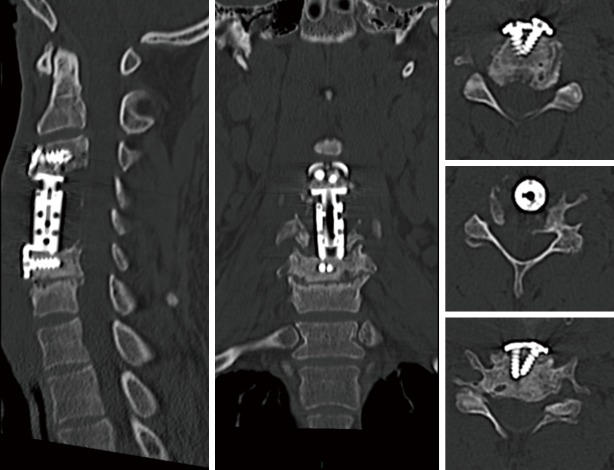
Figure 3.
Postoperative cervical CT showed a good realignment of cervical spine and the correct position of the WETC and screws. WETC, winged expandable titanium cage.
Figure 4.
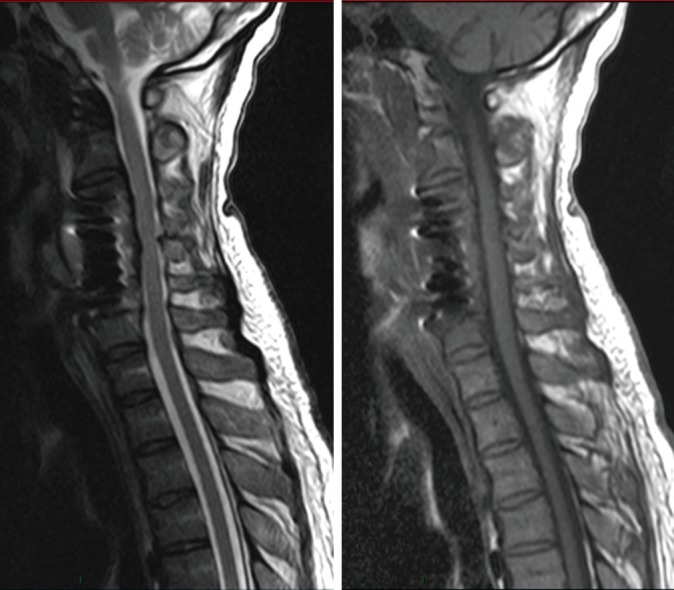
Follow-up cervical MRI demonstrated the resolution of the inflammatory process and no instability of the construct.
Discussion
Cervical spondylodiscitis is a quite rare finding respect the more common location of spinal abscesses in the lumbar and thoracic regions (2). The incidence of spinal tuberculosis is increasing in developed nations and surgical treatment is indicated for cases of instability, deformity, neurological deficit or in cases of resistance to the medical treatment in order to evacuate the abscess and consent the antibiotics to access within the capsule (3).
Over the years, many reconstructive techniques have been proposed after single or multiple cervical corpectomy as treatment for different diseases. The use of an ABG such as iliac or fibular is considered the gold standard, but linked by some authors to donor site morbidity, pseudoarthrosis and graft dislodgement. For the treatment of cervical spondylosis its use has been reported to be successful despite the presence of infection (4).
After single or multiple corpectomy a NETC was proposed to give more stiffness to the construct but its insertion can be demanding and some authors reported high rate of subsidence due to its scraping on the adjacent endplates.
In the application of metal implants in the presence of infection no implant complications have been reported by some authors (5). On the contrary other authors recommended long-term oral antibiotic regimes, eventual removal of these implants and microbiological resampling (6).
Mondorf et al. (7) reported the safe use of polyether ketone (PEEK) cage fusion in 5 patients affected by cervical spondylodiscitis.
The use of ETC has overcome the challenge presented by the insertion of NETC with the possibility to obtain a gradual correction of the cervical lordosis in site after its easy insertion.
Case series reporting its use for different diseases demonstrated good clinical and radiological results (8,9).
Nevertheless, in the use of ABG, NETC and ETC a high rate of subsidence has been reported (10,11) regardless to the disease, perhaps their use without a posterior fixation has been discouraged when multi-level decompression is executed. Sasso et al. (12) reported a 6% failure rate following two-level decompression and fusion using autologous iliac autograft and anterior plating and a 71% failure rate after three-level decompression.
In using WETC, we recently reported (1) good clinical and neurological results in a series of patients treated for cervical spondylosis.
Another issue is if an anterior approach alone is sufficient for cases of cervical spondylodiscitis. Heyde et al. (13) reported a series of 20 patients surgically treated for spondylodiscitis using a combined anterior-posterior fixation in 13 cases while an anterior approach alone was used only in 7 cases.
On the other hand, Shousha et al. (14) recently evaluated the behavior of cervical spondylodiscitis over a period of two decades in a single institution reporting that anterior surgery alone became more applicable.
Herein we report a case of cervical tuberculosis treated with a WETC in which the correction of a severe kyphosis was obtained and follow-up radiographs demonstrated no subsidence and the stability of the construct. We consider the use of WETC easier in its insertion respect a NETC and more practical respect an ETC since constituted by a single device, the fixation wings work as the anterior plating.
Shousha et al. (15) reported that ventral plating after corpectomy for spondylodiscitis should be avoided in order to avoid space available for the abscess formation. Nevertheless, it has been reported that the use of an ETC is considered safe in association to an anterior plating since a major stiffness of up to 254% was demonstrated (16). The use of a WETC can obviate this issue since no space is present between the cage and fixation wings and this may reduce the incidence of abscess formation.
After its insertion, we suggest an adequate preparation of the adjacent endplates in order to increase the adjacency between the bone and WETC and obtain distribution of the forces after its distraction.
Finally, this case report demonstrates that the use of a WETC after double corpectomy for severe kyphosis due to cervical tuberculosis is able to obtain good results in terms of clinical and radiological outcome.
Nevertheless, case series will be necessary to affirm the validity of this device as stand-alone, in particular for cases of cervical tuberculosis with severe kyphosis in which the risk of instability is high.
Conclusions
In using a WETC after single or multiple corpectomy, we recently reported a series of patients treated for cervical spondylosis.
Herein we report a case of cervical tuberculosis with severe kyphosis treated with this device after double cervical corpectomy. The patient fully recovered in post-operative period, kyphosis was corrected and no subsidence was present at radiological follow-up. This case report demonstrates that good clinical and radiological results can be obtained using this device, nevertheless case series will be necessary to affirm its validity as stand-alone in particular for cases of cervical tuberculosis with severe kyphosis in which the risk of instability is high.
Acknowledgements
None.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
Footnotes
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- 1.Tarantino R, Nigro L, Donnarumma P, et al. Cervical reconstruction techniques. After adequate selection of the patient report of a series of 34 patients treated with winged expandable cages. Neurosurg Rev 2017;40:281-6. 10.1007/s10143-016-0770-3 [DOI] [PubMed] [Google Scholar]
- 2.Muzii VF, Mariottini A, Zalaffi A, et al. Cervical spine epidural abscess: experience with microsurgical treatment in eight cases. J Neurosurg Spine 2006;5:392-7. 10.3171/spi.2006.5.5.392 [DOI] [PubMed] [Google Scholar]
- 3.Tarantino R, Donnarumma P, Fazzolari B, et al. Pott's disease: medical and surgical treatment. Clin Ter 2013;164:97-100. [DOI] [PubMed] [Google Scholar]
- 4.Stone JL, Cybulski GR, Rodriguez J, et al. Anterior cervical debridement and strut grafting for osteomyelitis of the cervical spine. J Neurosurg 1989;70:879-83. 10.3171/jns.1989.70.6.0879 [DOI] [PubMed] [Google Scholar]
- 5.Suess O, Weise L, Brock M, et al. Debridement and spinal instrumentation as a single-stage procedure in bacterial spondylitis/spondylodiscitis. Zentralbl Neurochir 2007;68:123-32. 10.1055/s-2007-984461 [DOI] [PubMed] [Google Scholar]
- 6.Shad A, Shariff S, Fairbank J, et al. Internal fixation for osteomyelitis of cervical spine: the issue of persistence of culture positive infection around the implants. Acta Neurochir (Wien) 2003;145:957-60. 10.1007/s00701-003-0129-8 [DOI] [PubMed] [Google Scholar]
- 7.Mondorf Y, Gaab MR, Oertel JM. PEEK cage cervical ventral fusion in spondylodiscitis. Acta Neurochir 2009;151:1537-41. 10.1007/s00701-009-0486-z [DOI] [PubMed] [Google Scholar]
- 8.Auguste KI, Chin C, Acosta FL, et al. Expandable cylindrical cages in the cervical spine: a review of 22 cases. J Neurosurg Spine 2006;4:285-91. 10.3171/spi.2006.4.4.285 [DOI] [PubMed] [Google Scholar]
- 9.Zaïri F, Aboukais R, Thines L, et al. Relevance of expandable titanium cage for the treatment of cervical spondylotic myelopathy. Eur Spine J 2012;21:1545-50. 10.1007/s00586-012-2380-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chen Y, Chen D, Guo Y, et al. Subsidence of titanium mesh cage: a study based on 300 cases. J Spinal Disord Tech 2008;21:489-92. 10.1097/BSD.0b013e318158de22 [DOI] [PubMed] [Google Scholar]
- 11.Kanayama M, Hashimoto T, Shigenobu K, et al. Pitfalls of anterior cervical fusion using titanium mesh and local autograft. J Spinal Disord Tech 2003;16:513-8. 10.1097/00024720-200312000-00005 [DOI] [PubMed] [Google Scholar]
- 12.Sasso RC, Ruggiero RA, Jr, Reilly TM, et al. Early reconstruction failures after multilevel cervical corpectomy. Spine (Phila Pa 1976) 2003;28:140-2. 10.1097/00007632-200301150-00009 [DOI] [PubMed] [Google Scholar]
- 13.Heyde CE, Bohem H, El Saghir H, et al. Surgical treatment of spondylodiscitis in the cervical spine: a minimum 2-year follow-up. Eur Spine J 2006;15:1380-7. 10.1007/s00586-006-0191-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shousha M, Heyde C, Boehm H. Cervical spondylodiscitis: change in clinical picture and operative management during the last two decades. A series of 50 patients and review of literature. Eur Spine J 2015;24:571-6. 10.1007/s00586-014-3672-5 [DOI] [PubMed] [Google Scholar]
- 15.Shousha M, Boehm H. Surgical treatment of cervical spondylodiscitis: a review of 30 consecutive patients. Spine (Phila Pa 1976) 2012;37:E30-6. 10.1097/BRS.0b013e31821bfdb2 [DOI] [PubMed] [Google Scholar]
- 16.Kandziora F, Pfugmacher R, Schaefer J, et al. Biomechanical comparison of expandable cages for vertebral body replacement in the cervical spine. J Neurosurg 2003;99:91-7. [DOI] [PubMed] [Google Scholar]