Figure 1.
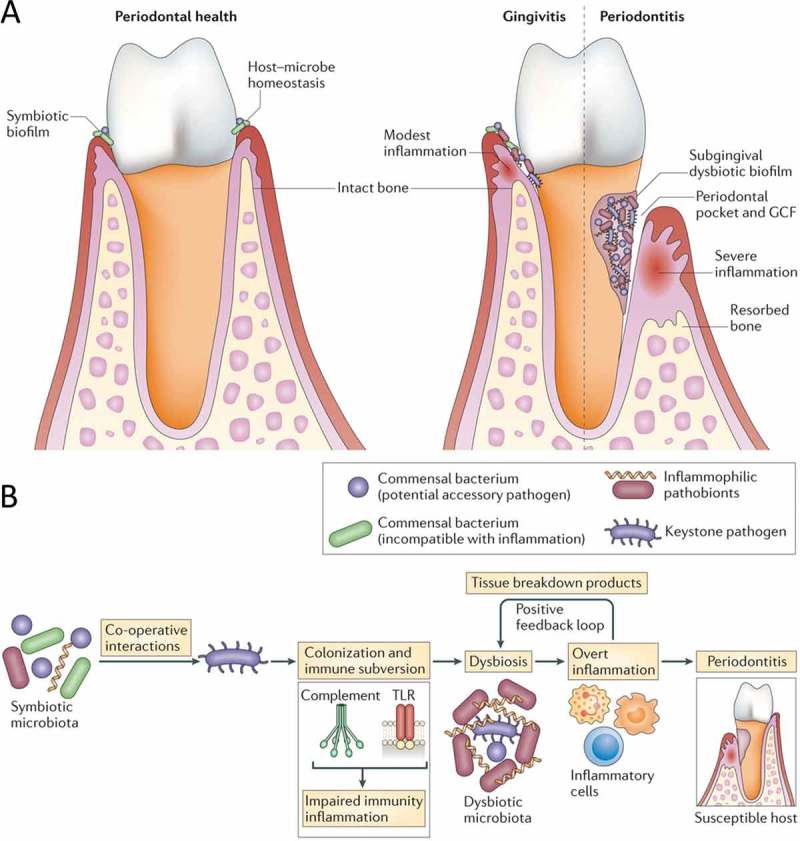
Dysbiosis and periodontal disease. (A) Progression from a state of periodontal health and host–microbe homeostasis to gingivitis (periodontal inflammation without bone loss) and to periodontitis, associated with a dysbiotic biofilm, formation of periodontal pockets, and induction inflammatory bone loss. (B) Periodontitis is induced in susceptible hosts by a polymicrobial community, wherein different members fulfill distinct roles that converge synergistically to cause destructive inflammation. Keystone pathogens, the colonization of which is facilitated by accessory pathogens, initially subvert the host response, leading to a dysbiotic community where pathobionts over-activate the inflammatory response and induce periodontal tissue degradation, including resorption of the supporting alveolar bone. Inflammation and dysbiosis positively reinforce each other because inflammatory tissue breakdown products (e.g. collagen peptides, heme-containing compounds) carried in the pockets via the gingival crevicular fluid are used as nutrients by the dysbiotic microbiota. This process generates a self-perpetuating pathogenic cycle that may underlie the chronicity of periodontitis. (From Hajishengallis [23]. Used with permission.)
