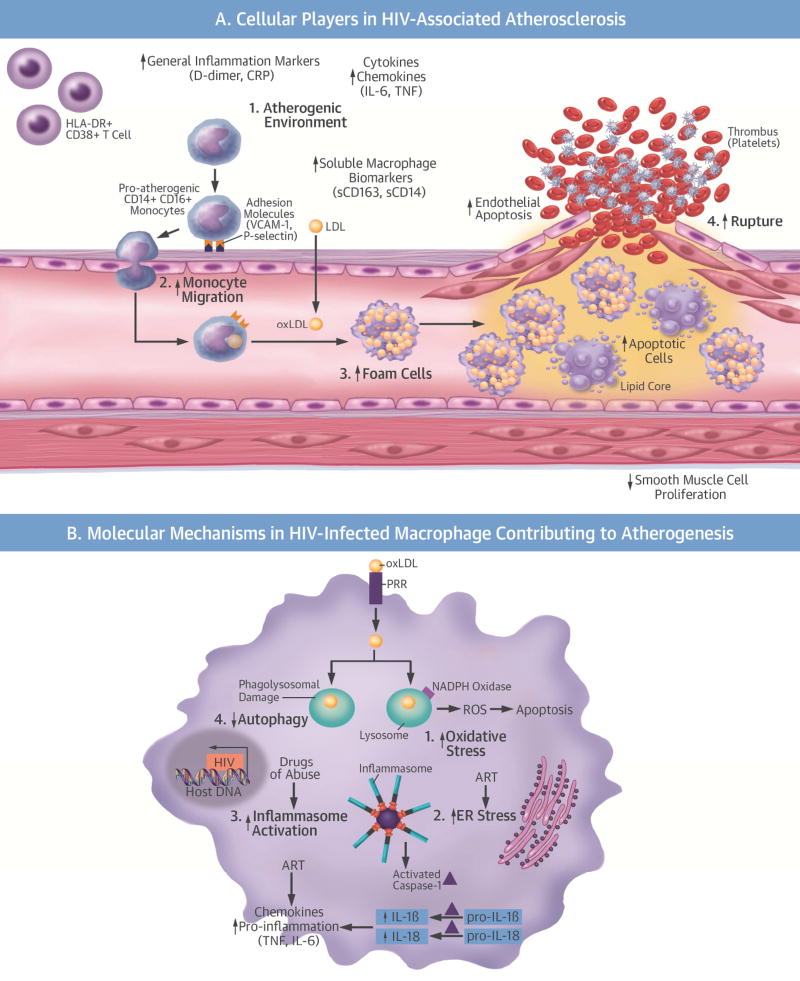
Central Illustration. Cellular and Molecular Mechanisms of HIV Atherogenesis.
(A) Cellular players in the initiation, progression, and plaque rupture of HIV-associated atherosclerosis. 1) HIV enhances the inflammatory environment, causing an increase in atherogenic monocytes, HLA-DR+CD38+ T cells, cytokines, and chemokines. 2) The increase in atherogenic monocytes and chemokines increases monocyte migration into the vasculature. 3) HIV increases foam cell formation. 4) HIV decreases smooth muscle cell proliferation and increases endothelial and foam cell apoptosis, making the plaque more vulnerable to rupture. (B) Molecular mechanisms in an HIV-infected macrophage contributing to atherogenesis: 1) increased OS; 2) increased ER stress; 3) increased inflammasome activation and cytokine production; 4) decreased autophagy. These molecular mechanisms amplify each other and are further complicated by ART and HIV risk factors and comorbidities. ART = antiretroviral therapy; CRP = C-reactive protein; ER = endoplasmic reticulum; HCV = hepatitis C virus; HIV = human immunodeficiency virus; IL = interleukin; LDL = low-density lipoprotein; NADPH = nicotinamide adenine dinucleotide phosphate; OS = oxidative stress; oxLDL= oxidized low-density lipoprotein; PRR = pathogen recognition receptor; ROS = reactive oxygen species; TNF = tumor necrosis factor; VCAM-1 = vascular cell adhesion molecule-1.