Abstract
AIM
To evaluate the therapeutic effect of fluorofenidone on disrupted blood-retinal barrier in the diabetic mice and uncover its underlying mechanism.
METHODS
db/db mice were randomly chosen for treatment with daily doses of fluorofenidone or placebo at 5-week-old, treatment continued until mice reach 24-week-old. Then, expression of transcriptiona factor insulin gene enhancer binding protein-1 (Islet-1) and vascular endothelial growth factor (VEGF) in murine retinas were evaluated. Retinal vascular permeability was assessed by examining the level of albumin in db/db murine retinas. Furthermore, the retinal vessel tight junction was estimated by checking the level of occludin in the murine retinal tissues.
RESULTS
After occurrence of diabetic retinopthy in db/db mice, expressions of transcritpional factor Islet-1 was found to be upregulated in db/db murine retinas compared with non-diabetic controls. Similar to expression pattern of Islet-1, VEGF were also demonstrated to be increased in retinas of db/db mice, which was accompanied by increased retinal vascular leakage and decreased tight junction protein level. Systemetic administration of fluorofenidone repaired broken retinal vascular tight junction by restoring occludin expression in db/db retinal tissue. Consequently, retinal vascular premeability were indicated to be reduced by examining the transudative albumin level in diabetic retinal tissues. Both Islet-1 and VEGF expression were inhibited in the retinas of db/db mice after treatment with fluorofenidone.
CONCLUSION
Fluorofenidone significantly protectes retinal tight junction and reduces retinal vascular leakage. The phenomenon can be partially attributed to reducing overexpression of Islet-1 and VEGF in diabetic retinal tissues.
Keywords: pyridone agent, diabetic retinopathy, blood-retinal barrier
Introduction
Diabetic retinopathy is one of the diseases that cause vision loss in the world. Approximately 75% of all diabetic patients show clinical signs of retinopathy within 15y after onset of diabetes[1]. Diabetic macular edema arising from vascular leakage due to inner blood-retinal barrier (iBRB) damage is the major cause of loss of vision in patients with diabetic retinopathy[2]. Several cytokines have been demonstrated to particpate in the pathogenesis of iBRB breakdown in diabetic patients. Growing evidence indicates that vascular endothelial growth factor (VEGF) is related to iBRB damage in diabetic retinopathy. It has been demonstrated VEGF levels dramaticallty upregulated in patients with diabetic macular edema and associated with vascular leakage, making it a highly important therapeutic target[3]–[5]. More recently, efforts with anti-VEGF therapy have produced promising results in patients with diabetic macular edema[6]. It has been confirmed that hypoxia inducible factor-1 (HIF-1) could regulate VEGF expression at transcriptional level. Treatment targeting HIF-1α could reduce the leakage of retinal blood vessels by inhibiting the expression of VEGF[7]. In addition to HIF-1α, a growing number of transcription factors, such as PPARg-coactivator-1a[8], have been shown to be involved in the regulation of VEGF expression. Figure out the regulation pathway of VEGF expression, and found more transcription factor which involved in regulating the expression of VEGF, would help us have better understanding the pathogenesis of diabetic retinopathy and providing better way to treat diabetic retinopathy.
Islet-1 is a LIM domain transcription factor[9]. The functions of Islet-1 involve in cell fate specification and embryonic development[10]. Recently, exogenous Islet-1 has been proven to possess ability to enhance proliferative, migratory and tube formation properties of the vascular endothelial cells, which is attributed to increased secretion of VEGF[11]. Moreover, accumulated date indicate that Islet-1 gene mutation is correlated with type 2 diabetes. It could manipulate body weight and glucose homeostasis via the activation of proglucagon gene expression. Islet-1, as a transcription factor, has a role in promoting angiogenesis and associated with diabetes. However, until now, there is no research on whether endogenous Islet-1 is involved in the occurrence of diabetic retinopathy. Therefore, the current study is to investigate whether the transcription factor Islet is related to the disruption of iBRB in diabetic mice.
It has been shown that pirfenidone, as a pyridone agent, could ameliorate fibrosis in different tissues[12]–[13]. Oral administration of pirfenidone was approved to be safe for suppression of fibrosis in clinical trials. Fluorofenidone (AKF-PD) is an improved analog of pirfenidone. The difference in structures between fluorofenidone and pirfenidone is that the hydro- at the metaposition of the benzene ring in pirfenidone is replaced by fluoro- in fluorofenidone. Alteraton of this chemical structure could result in promotion of absorption and transmission ability and increasing physiological activity. Since now, it has been demonstrated that fluorofenidone could attenuate diabetic nephropathy and kidney fibrosis in different anmial models[14]–[15]. It is widely believed that diabetic retinopathy and nephropathy are two major microvascular complications of diabetes mellitus, which lead to blindness and end-stage renal disease. Diabetic retinopathy always find to be accompanied by diabetic nephropathy in clinic. It has also been cofirmed that diabetic nephropathy was related to the severity of diabetic macular edema[16]. These findings drive us to imagine whether fluorofenidone has a therapeutic effect on diabetic retinopathy.
In order to find the answers to these questions. db/db mice were used to figure out changes of Islet-1 gene expression in murine retinal tissues during the process of diabetic retinopathy, and to find correlation between Islet-1 and diabetic retinopathy. The second purpose of our study was to evaluate the therapeutic effects of fluorofenidone on the disrupted blood-retinal barrier and to explore its underlying mechanism in diabetic mice.
MATERIALS AND METHODS
Animals
C57BL/KsJ db/db male and age-matched db/m mice were obtained from Silaike (Shanghai, China), which were bred and maintained in a pathogen-free environment with a 12-hour light/dark cycle. The experimental animals were composed of following groups: normal control group (db/m mice, n=16), negative control group (1% CMC-Na was used to treat db/db mice, n=16) and treatment group (db/db mice treated by oral gavage at dose of 500 mg/(kg·d) of fluorofenidone, n=16). Treatment started at the age of 5wk with an end point at 24-week old. Body weight of mice was measured.
Analysis of Blood Glucose and Serum Lipids
Following a 12-hour overnight fast, blood from the tail vein was collected. Blood glucose meter was used to measure blood glucose levels in mice (LifeScan, Milpitas, CA, USA). Meanwhile, automatic analyzer model 7170 (Hitachi Co., Ltd., Japan) was adopted to exmine serum levels of triglyceride and cholesterol.
Determination of Disruption of Blood-retinal Barrier
In order to analyze the extent of damage of the blood-retinal barrier in db/db mice, the level of albumin leaking from retinal vessels was evaluated. Once deeply anesthetized, the chest of the mice was opened followed by insertin of a catheter into the left ventricle with a small incision on the right atrium. Phosphate buffer saline was infused. Consequently, mice were sacrificed and retina was isolated, extravascular level of albumin in murine retina was assessed by using the Western blot technique.
Western Blot
Total protein of murine retinas were collected and resolved on sodium dodecyl sulfate (SDS)-polyacrylamide gel, then it was transferred onto a nitrocellulose membrane and incubated with anti-Islet-1 (Abcam, UK), anti-VEGF (Abcam, UK), anti-Albumin(Abcam, UK), anti-occludin (Abcam, UK) and anti-β-actin antibodies (Sigma, USA). Membranes were incubated with peroxidase-conjugated secondary antibodies and developed using the ECL system.
Statistical Analysis
All the data were expressed as mean±SEM and processed by SPSS20.0 statistical package. One-way analysis of variance followed by the LSD test were utilized to assess significant differences. P<0.05 would be considered to be statistically significant.
Results
Clinical Characteristics of the Mice After Fluorofenidone Treatment
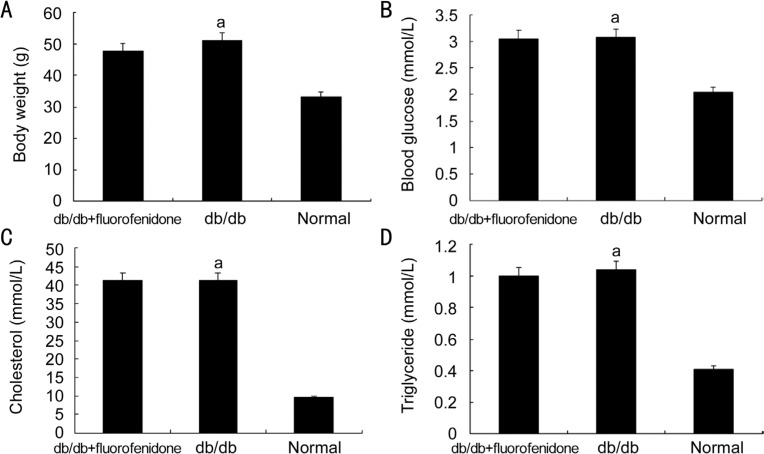
Serum lipid together with blood glucose and body weight were monitored in db/db mice before and after fluorofenidone treatment. Body weights (db/db vs db/m: 50.97±2.95 vs 33.02±0.44 g, P<0.05) and blood glucose concentrations of db/db mice (db/db vs db/m: 41.11±3.61 vs 9.51±0.72 mmol/L, P<0.05) were dramatically increased compared with db/m mice. Similarly, we also found serum concentrations of cholesterol (db/db vs littermates: 3.08±0.62 vs 2.04±0.21 mmol/L, P<0.05) and triglycerides (db/db vs littermates: 1.04±0.15 vs 0.41±0.05 mmol/L, P<0.05) were upregulated in db/db mice when compared with db/m mice. Conversely, the difference between fluorofenidone-treated db/db and placebo-treated db/db mice was insignificant. Treatment with fluorofenidone did not affect serum levels of triglycerides (fluorofenidone vs db/db: 1.00±0.11 vs 1.04±0.15 mmol/L, P>0.05), cholesterol (fluorofenidone vs db/db: 43.06±0.13 vs 3.08±0.62 mmol/L, P>0.05), glucose (fluorofenidone vs db/db: 41.17±2.78 vs 41.11±3.61 mmol/L, P>0.05) compared with placebo-treated mice. Fluorofenidone did not change body weight of the mice (fluorofenidone vs db/db: 47.75±4.83 vs 50.97±2.95 g, P>0.05) (Figure 1). In summary, with progression of diabetes, db/db mice manifested as increased body weight and elevated level of blood glucose and serum lipid.
Figure 1. Body weight and serum concentration of glaucose or lipid in db/db mice after fluorofenidone treatment.
A: Body weight of db/db mice and normal control mice were measured; B: Blood glucose of mice were examined; C, D: Serum concentrations of cholesterol and triglyceride were evaluated. The difference between placebo-treated db/db mice and normal control mice (nondiabetic mice) was statistically significant (aP<0.05).
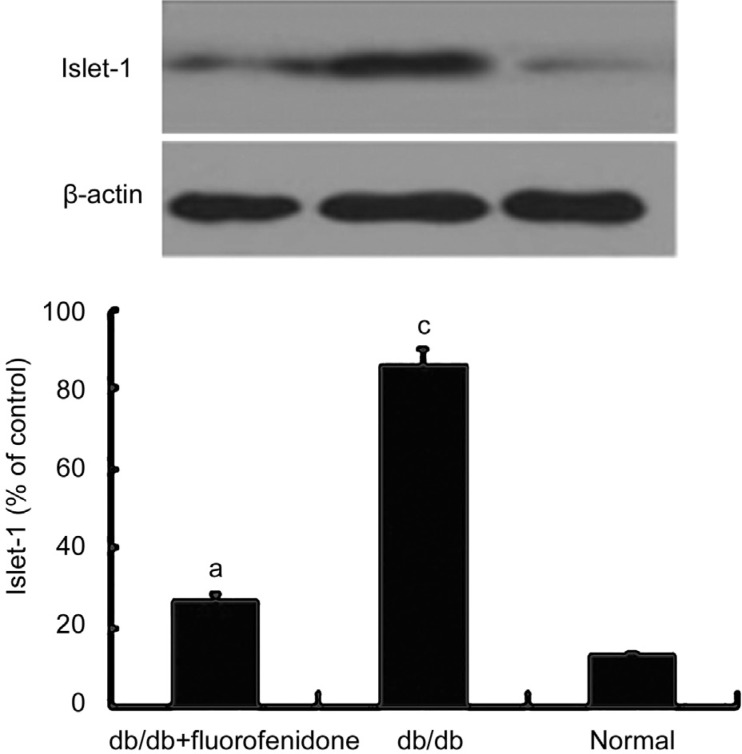
Downregulation of Retinal Islet-1 Expression in the Retinas of db/db Mice by Fluorofenidone
To figure out the relationship between Islet-1 and diabetic retinopathy, Islet-1 level in the retinas of db/db mice was evaluated at age 24wk, Diabetic retinopathy has been occurring in the retinal tissues at this time. We found that expression of Islet-1 in db/db murine retina was significantly increased compared with normal control (P<0.05, Figure 2). This indicates that the occurrence of diabetic retinopathy can induce the expression of Islet-1, we infer that there is a positive correlation between the expression of Islet-1 and diabetic retinopathy and Islet-1 may play a potential role in this process. We also found, compared with placebo-treated db/db mice, systematic administration of fluorofenidone suppressed the expresssion of Islet-1 in the db/db retinas (P<0.05) and almost completely reversed this pathological upregulation which was induced by diabetes to normal level (Figure 2).
Figure 2. Effect of fluorofenidone on Islet-1 expression in murine retinas.
The level of trascriptional factor Islet-1 in the retinas of mice was assessed by Western blot. Islet-1 expression in the db/db murine retinas were dramatically increased compared with normal control mice. Systematic adminstration of fluorofenidone almost completely attenuated upregulation of Islet-1 expression in the retinas of db/db mice. The difference between placebo-treated db/db mice and db/db mice treated with fluorofenidone was statistically significant (aP<0.05). The difference between placebo-treated db/db mice and normal control mice was statistically significant (cP<0.05).
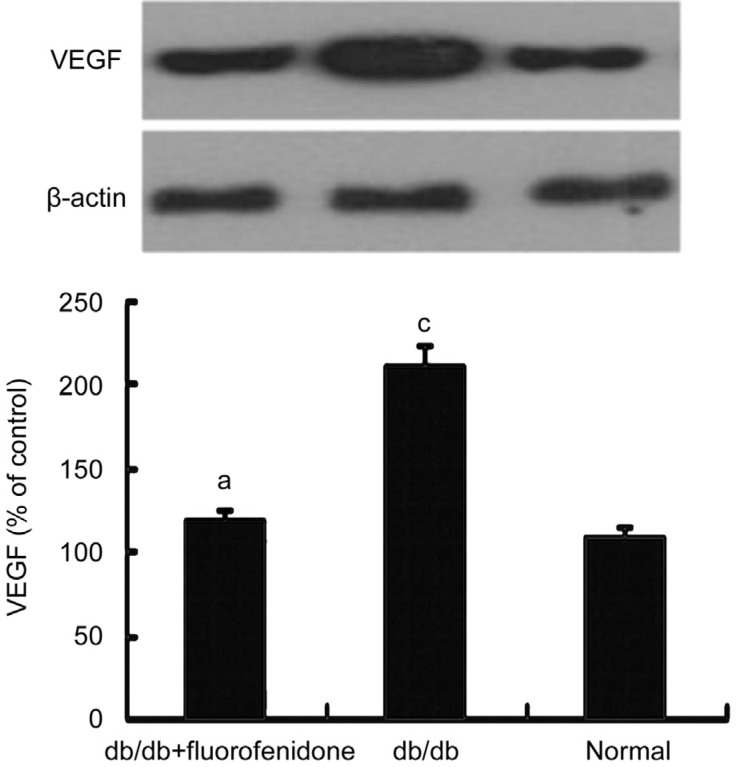
Effect of Fluorofenidone on Vascular Endothelial Growth Factor Expression in the Retinas of db/db Mice
Overexpression of VEGF has been demontrated in diabetic retinopathy, which result in disruption of blood-retinal barrier and vascular leakage. Be consistent with it, we detected an increased level of VEGF in db/db retinas with high glucose compared with normal control mice (P<0.05, Figure 3). Then, effects of fluorofenidone on retinal VEGF expression in db/db mice was evaluated. Compared with placebo-treated db/db mice, VEGF expression was dramatically decreased in the retinas of db/db mice which was systematically adniminstrated with fluorofenidone (P<0.05, Figure 3). It has been proven that Islet-1 could promote the angiogenesis by increasing the expression of VEGF. This indicates that Islet directly or indirectly participate in the regulation of VEGF expression. We obseved inbibition of the expression of Islet-1 in retinal tissues by fluorofenidone, which may consequently downregulate expression of VEGF on transcriptional level in the retina of diabetic mice.
Figure 3. Effect of fluorofenidone on VEGF expression in murine retinas.
VEGF expression was statistically upregulated in retinas of db/db mice, which was suppressed by fluorofenidone treatment. The difference between placebo-treated db/db mice and db/db mice treated with fluorofenidone was statistically significant (aP<0.05). The difference between placebo-treated db/db mice and normal control mice was statistically significant (cP<0.05).
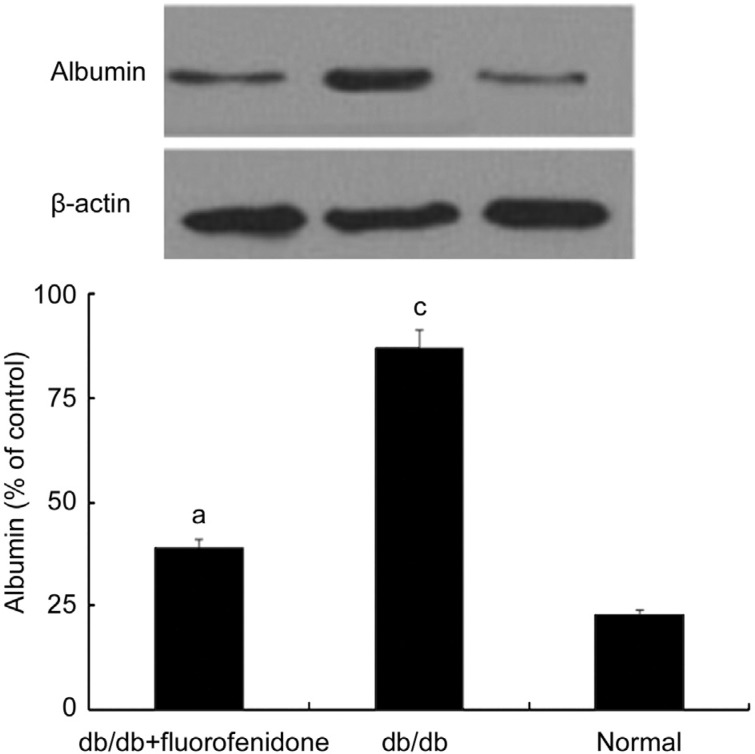
Effect of Fluorofenidone on Blood-retina Barrier in db/db Mice
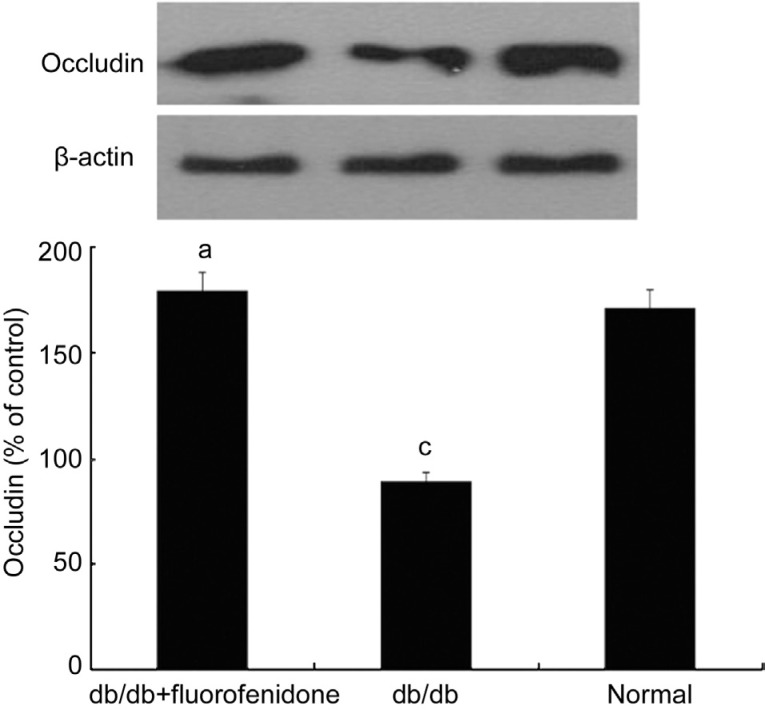
In order to examine the therapeutic efficacy of fluorofenidone on the blood-retinal barrier, we detected the level of albumin in murine retinal tissues. As shown in Figure 4, the level of albumin was significantly increased in the retinas of db/db mice compared with that of normal control (P<0.05). Systematical administration of fluorofenidone significantly decreased extravascular leakage of albumin in db/db mice (Figure 4, P<0.05). To figure out whether this phenomenon was related to alteration of the tight junction protein expression, we assessed the level of occludin in the retina of db/db mice. It demonstrated that the expression of occludin downregulated in db/db mice compared with non-diabetic littermates (Figure 5, P<0.05). Fluorofenidone treatment almost completely restored retinal occludin expression in db/db mice (Figure 5, P<0.05).
Figure 4. Albumin expression in murine retinas.
Albumin content was higher in the retinas of db/db mice when compared with non-diabetic littermates. Systematical administration of fluorofenidone significantly decreased extravascular leakage of albumin in db/db mice. The difference between placebo-treated db/db mice and db/db mice treated with fluorofenidone was statistically significant (aP<0.05). The difference between placebo-treated db/db mice and normal control mice was statistically significant (cP<0.05).
Figure 5. Occludin expression in murine retinas.
Retinal occludin level significantly decreased in db/db mice compared with that in non-diabetic littermates. Fluorofenidone treatment almost completely restored retinal occludin expression. The difference between placebo-treated db/db mice and db/db mice treated with fluorofenidone was statistically significant (aP<0.05). The difference between placebo-treated db/db mice and normal control mice was statistically significant (cP<0.05).
DISCUSSION
Significant upregulation of Islet-1 expression were found in the retinas of db/db mice. Islet-1 transcriptional activity play important roles in tissue specification and correlate with the activity of the insulin and glucagon genes[17]–[20]. It has been shown that Islet-1 could promote postnatal angiogenesis and vasculogenesis, which is attributed to increased secretion of VEGF[11]. In current study, along with elevated expression of Islet-1, the level of VEGF also increased significantly in db/db mice. Previous reports have demonstrated that VEGF could improve vascular permeability in diabetic patients and correlated with the diabetic macular edema[21]. In this study, expression of Islet-1 was significantly increased in parallel with elevated VEGF levels, vascular leakage and tight junction damage in the retinas of db/db mice. These findings suggest that Islet-1 may participate in diabetes-induced VEGF expression and iBRB breakdown.
Our findings showed that fluorofenidone significantly reversed retinal vascular leakage. To further unveil whether fluorofenidone has direct effects on the blood retinal barrier, we evlauated the effect of fluorofenidone on retinal tight junction. Our findings indicated that fluorofenidone attenuated the downregulation of tight junction protein-occludin in the retinas of db/db mice. Several studies have demonstrated that VEGF-mediated disruption of endothelial transmembrane tight-junction proteins is contributed to the breakdown of iBRB in diabetic retinopathy[22]. In accord with previous study, downregulation of tight junction protein is associated with decrease of VEGF levels in the retinal tissues after administration of fluorofenidone. We show here that protein expression of Islet-1 were suppressed by treatment with fluorofenidone. Downregulation expression of Islet-1 could concomitant attenuation of VEGF levels in retinals of db/db mice. These findings indicate an important role of Islet-1 in retinal vascular leakage through regulation of VEGF expression. Moreover, some other unknown factors implicated in iBRB breakdown may also be regulated by Islet-1. Inhibition of Islet-1 by systematically administration of fluorofenidone may suppress retinal vascular leakage through decreasing Islet-1 regulated other downstream genes besides VEGF. Further study is necessary to elucidated it.
In summary, our study suggested that Islet-1 expression is upregulated in association with VEGF expression in the retinas of db/db mice, which is attibuted to retinal vascular leakage and tight junction diruption. Fluorofenidone could reverse retinal tight junction and reduce retinal vascular leakage in db/db mice. The therapeutic efficacy of fluorofenidone on blood-retinal barrier is at least in part mediated by the inhibition of VEGF expression via attenuation of Islet-1 levels in diabetic retinal tissues.
Acknowledgments
We thank Dr. Li-Jian Tao and Dr. Xuan Xiong for providing db/db mice with fluorofenidone treatment.
Foundations: Supported by National Natural Science Foundation of China (No.81000388); Health and Family Planning Commission of Hunan Province (No.132015-016); Natural Science Foundation of Hunan Province (No.12JJ3120).
Conflicts of Interest: Xiong SQ, None; Jiang HB, None; Xu HZ, None; Xia XB, None.
REFERENCES
- 1.Klein R, Klein BE, Moss SE. Epidemiology of proliferative diabetic retinopathy. Diabetes Care. 1992;15(6):1875–1189. doi: 10.2337/diacare.15.12.1875. [DOI] [PubMed] [Google Scholar]
- 2.Lian JX, Gangwani RA, McGhee SM, Chan CK, Lam CL, Primary Health Care Group. Wong DS. Systematic screening for diabetic retinopathy (DR) in Hong Kong: prevalence of DR and visual impairment among diabetic population. Br J Ophthalmol. 2016;100(2):151–155. doi: 10.1136/bjophthalmol-2015-307382. [DOI] [PubMed] [Google Scholar]
- 3.Thomas AA, Feng B, Chakrabarti S. ANRIL: a regulator of VEGF in diabetic retinopathy. Invest Ophthalmol Vis Sci. 2017;58(1):470–480. doi: 10.1167/iovs.16-20569. [DOI] [PubMed] [Google Scholar]
- 4.Funatsu H, Yamashita H, Noma H, Mimura T, Yamashita T, Hori S. Increased levels of vascular endothelial growth factor and interleukin-6 in the aqueous humor of diabetics with macular edema. Am J Ophthalmol. 2002;133(1):70–77. doi: 10.1016/s0002-9394(01)01269-7. [DOI] [PubMed] [Google Scholar]
- 5.Xia XB, Xiong SQ, Song WT, Luo J, Wang YK, Zhou RR. Inhibition of retinal neovascularization by siRNA targeting VEGF (165) Mol Vis. 2008;14:1965–1973. [PMC free article] [PubMed] [Google Scholar]
- 6.Ho AC, Scott IU, Kim SJ, Brown GC, Brown MM, Ip MS, Recchia FM. Anti-vascular endothelial growth factor pharmacotherapy for diabetic macular edema: a report by the American Academy of Ophthalmology. Ophthalmology. 2012;119(10):2179–2188. doi: 10.1016/j.ophtha.2012.07.058. [DOI] [PubMed] [Google Scholar]
- 7.Xia XB, Xiong SQ, Xu HZ, Jiang J, Li Y. Suppression of retinal neovascularization by shRNA targeting HIF-1alpha. Curr Eye Res. 2008;33(10):892–902. doi: 10.1080/02713680802416670. [DOI] [PubMed] [Google Scholar]
- 8.Saint-Geniez M, Jiang A, Abend S, Liu L, Sweigard H, Connor KM, Arany Z. PGC-1α regulates normal and pathological angiogenesis in the retina. Am J Pathol. 2013;182(1):255–265. doi: 10.1016/j.ajpath.2012.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hunter CS, Rhodes SJ. LIM-homeodomain genes in mammalian development and human disease. Mol Biol Rep. 2005;32(2):67–77. doi: 10.1007/s11033-004-7657-z. [DOI] [PubMed] [Google Scholar]
- 10.Wilfinger A, Arkhipova V, Meyer D. Cell type and tissue specific function of islet genes in zebrafish pancreas development. Dev Biol. 2013;378(1):25–37. doi: 10.1016/j.ydbio.2013.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Xiong SQ, Jiang HB, Li YX, Li HB, Xu HZ, Wu ZK, Zheng W, Xia XB. Role of endogenous insulin gene enhancer protein ISL-1 in angiogenesis. Mol Vis. 2016;22:1375–1386. [PMC free article] [PubMed] [Google Scholar]
- 12.Di Sario A, Bendia E, Macarri G, Candelaresi C, Taffetani S, Marzioni M, Omenetti A, De Minicis S, Trozzi L, Benedetti A. The anti-fibrotic effect of pirfenidone in rat liver fibrosis is mediated by downregulation of procollagen alpha1(1), TIMP-1 and MMP-2. Dig Liver Dis. 2004;36(11):744–751. doi: 10.1016/j.dld.2004.05.012. [DOI] [PubMed] [Google Scholar]
- 13.Behr J, Bendstrup E, Crestani B, Günther A, Olschewski H, Skold CM, Wells A, Wuyts W, Koschel D, Kreuter M, Wallaert B, Lin CY, Beck J, Albera C. Safety and tolerability of acetylcysteine and pirfenidone combination therapy in idiopathic pulmonary fibrosis: a randomised, double-blind, placebo-controlled, phase 2 trial. Lancet Respir Med. 2016;4(6):445–453. doi: 10.1016/S2213-2600(16)30044-3. [DOI] [PubMed] [Google Scholar]
- 14.Li BX, Tang YT, Wang W, Xie YY, Wang NS, Yuan QJ, Zhang FF, Peng ZZ, Hu GY, Tao LJ. Fluorofenidone attenuates renal interstitial fibrosis in the rat model of obstructive nephropathy. Mol Cell Biochem. 2011;354(1-2):263–273. doi: 10.1007/s11010-011-0826-1. [DOI] [PubMed] [Google Scholar]
- 15.Qin J, Xie YY, Huang L, Yuan QJ, Mei WJ, Yuan XN, Hu GY, Cheng GJ, Tao LJ, Peng ZZ. Fluorofenidone inhibits nicotinamide adeninedinucleotide phosphate oxidase via PI3K/Akt pathway in the pathogenesis of renal interstitial fibrosis. Nephrology (Carlton) 2013;18(10):690–699. doi: 10.1111/nep.12128. [DOI] [PubMed] [Google Scholar]
- 16.Romero-Aroca P, Mendez-Marin I, Baget-Bernaldiz M, Fernéndez-Ballart J, Santos-Blanco E. Review of the relationship between renal and retinal microangiopathy in diabetes mellitus patients. Curr Diabetes Rev. 2010;6(2):88–101. doi: 10.2174/157339910790909387. [DOI] [PubMed] [Google Scholar]
- 17.Cai CL, Liang X, Shi Y, Chu PH, Pfaff SL, Chen J, Evans S. Isl1 identifies a cardiac progenitor population that proliferates prior to differentiation and contributes a majority of cells to the heart. Dev Cell. 2003;5(6):877–889. doi: 10.1016/s1534-5807(03)00363-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kim KT, Kim N, Kim HK, Lee H, Gruner HN, Gergics P, Park C, Mastick GS, Park HC, Song MR. ISL1-based LIM complexes control Slit2 transcription in developing cranial motor neurons. Sci Rep. 2016;7(6):36491. doi: 10.1038/srep36491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Du A, Hunter CS, Murray J, Noble D, Cai CL, Evans SM, Stein R, May CL. Islet-1 is required for the maturation, proliferation, and survival of the endocrine pancreas. Diabetes. 2009;58(9):2059–2069. doi: 10.2337/db08-0987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Peng SY, Wang WP, Meng J, Li T, Zhang H, Li YM, Chen P, Ma KT, Zhou CY. ISL1 physically interacts with BETA2 to promote insulin gene transcriptional synergy in non-beta cells. Biochim Biophys Acta. 2005;1731(3):154–159. doi: 10.1016/j.bbaexp.2005.08.013. [DOI] [PubMed] [Google Scholar]
- 21.Funatsu H, Yamashita H, Sakata K, Noma H, Mimura T, Suzuki M, Eguchi S, Hori S. Vitreous levels of vascular endothelial growth factor and intercellular adhesion molecule 1 are related to diabetic macular edema. Ophthalmology. 2005;112(5):806–816. doi: 10.1016/j.ophtha.2004.11.045. [DOI] [PubMed] [Google Scholar]
- 22.Harhaj NS, Felinski EA, Wolpert EB, Sundstrom JM, Gardner TW, Antonetti DA. VEGF activation of protein kinase C stimulates occludin phosphorylation and contributes to endothelial permeability. Invest Ophthalmol Vis Sci. 2006;47(11):5106–5115. doi: 10.1167/iovs.06-0322. [DOI] [PubMed] [Google Scholar]