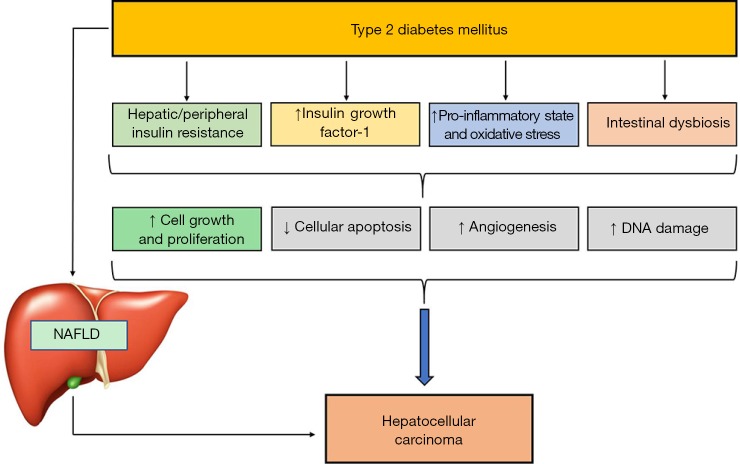
Figure 1.
Putative biological mechanisms linking type 2 diabetes mellitus and nonalcoholic fatty liver disease (NAFLD) to the development and progression of hepatocellular carcinoma. The biological mechanisms underlying the association between type 2 diabetes, NAFLD and hepatocellular carcinoma are complex and not entirely understood. Both type 2 diabetes and NAFLD are strongly associated with abdominal obesity, hepatic/peripheral insulin resistance, low-grade chronic inflammation and increased oxidative stress that may contribute to the development and progression of hepatocellular carcinoma, promoting increased cellular growth and proliferation, inhibition of cellular apoptosis, increased angiogenesis and DNA damage. Insulin resistance and coexistent chronic hyperinsulinemia lead to increased production of insulin-like growth factor 1 (IGF-1), which further promotes hepatic cellular growth/proliferation and inhibits cellular apoptosis within the liver. In addition, chronic hyperinsulinemia also activates insulin receptor substrate-1 (IRS-1), which plays a key role in the regulation of multiple cytokine pathways potentially implicated in the pathophysiology of hepatocellular carcinoma. Evidence also suggests that insulin resistance alters gut microbiota (dysbiosis) and increases circulating levels of free fatty acids, which promote hepatic steatosis (NAFLD); both of these pathologic conditions play a part in the development and progression of hepatocellular carcinoma. In particular, clear evidence indicates that NAFLD, especially in its necro-inflammatory form, exacerbates hepatic/peripheral insulin resistance and causes the intrahepatic release of multiple hepatokines and mediators that increase the risk of hepatic carcinogenesis.