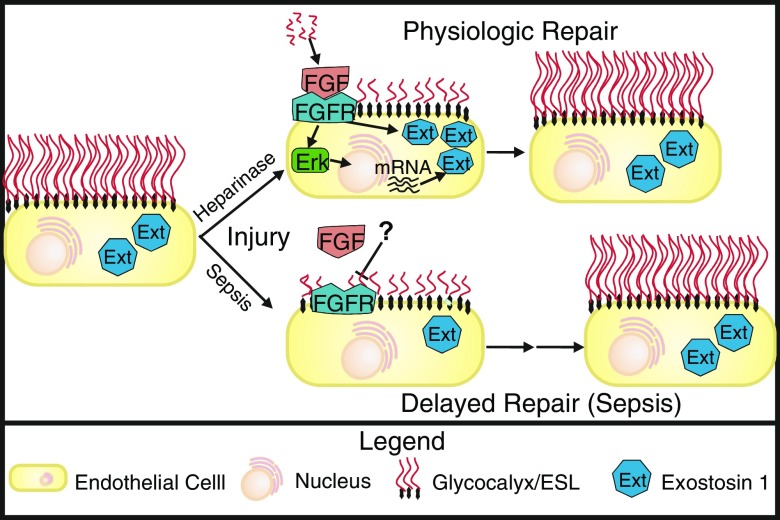
Figure 1.
Sepsis inhibits fibroblast growth factor (FGF)-mediated repair of the pulmonary endothelial glycocalyx. At baseline, pulmonary endothelial cells project a long glycocalyx/endothelial surface layer (ESL) into the vessel lumen that is maintained in part via exostosin-1 (Ext) expression (left). Injury by either infusion of heparinase or sepsis causes disruption of the pulmonary endothelial ESL and release of heparin sulfate (HS) fragments. Physiologic repair of the ESL after heparinase injury occurs rapidly because HS fragments activate FGF signaling, which leads both to activation of existing Ext as well as Erk-mediated up-regulation of additional Ext, resulting in rapid reconstitution of the ESL. In contrast, repair after sepsis-induced injury is significantly delayed because sepsis leads to inhibition of fibroblast growth factor receptor 1 (FGFR) signaling and subsequent suppression of the FGF-mediated pathway that is necessary for Ext activation and up-regulation.