Abstract
Objective
Asian Americans consume more sodium than other racial/ethnic groups. The purpose of this analysis was to describe major sources of sodium intake to inform sodium reduction initiatives.
Methods
Cross-sectional data on adults (aged >18 years) from the National Health and Nutrition Examination Survey (NHANES) 2011-2012 with one 24-hour dietary recall were analyzed (n=5,076). Population proportions were calculated from “What We Eat in America” (WWEIA) food categories.
Results
Asian Americans had a higher sodium density vs adults of other racial/ethnic groups (means in mg/1000kcal: Asian American, 2031.1; Hispanic,1691.6; White: 1666.5; Black: 1655.5; P<.05, all). Half of sodium consumed by Asian Americans came from the top 10 food categories, in contrast to Hispanics (43.6%), Whites (39.0%), and Blacks (36.0%). Four food categories were a top source of sodium for Hispanics, Whites, Blacks, and others, but not among Asian Americans: cold cuts and cured meats; meat mixed dishes; eggs and omelets; and cheese. The top three food category sources of sodium among Asians were soups, rice, and yeast breads accounting for 28.9% of dietary sodium. Asian Americans were less likely to add salt at the table, but used salt in food preparation ‘very often’ (P for both <.01).
Conclusions
Mean sodium consumption and sources vary across racial/ethnic groups with highest consumption in Asian Americans. Given the smaller number of food categories contributing to sodium intake in Asian Americans, results imply that targeted activities on a few food items would have a large impact on reducing sodium intake in this group.
Keywords: Sodium, Race, Ethnicity, Asian Americans
Introduction
Cardiovascular disease is the leading cause of death in the United States (US)1 and hypertension is a leading risk factor. A positive and continuous relationship between sodium intake and blood pressure is well established,2 yet 89% of US adults consume more sodium than recommended by the US Department of Health and Human Services and the US Department of Agriculture’s (USDA) Dietary Guidelines for Americans.3 Existing estimates of sodium intake measured by self-report show that US adults consume an average of 3,552mg/day (SE 32.2),4 well above recommendations (1,500-2,300mg/day), and public health efforts aim to reduce sodium consumption.5-7 Salt sensitivity, defined as greater blood pressure response to sodium intake than average, is more prevalent in non-Hispanic Blacks and Asian populations;8-10 thus, an understanding of racial/ethnic variation in sources of dietary sodium and salt behaviors has important implications for public health practice.
Asians, particularly those in East and Central Asia, have the highest sodium intakes in the world.11 Mean sodium intake in East Asia, high-income Asia Pacific (mainly Japan and South Korea) and Central Asia were 4,800mg/day, 5,000mg/day and 5,510mg/day, respectively; out of all regions, East Asia experienced the largest increases from 1990 to 2010 (430mg/day). Sodium intakes in Asia may inform US recommendations, but an understanding of sodium intakes among Asian Americans who have different dietary patterns based on American influences is necessary. Despite this, few data exist on Asian American diets. A 2011-2012 analysis of National Health and Nutrition Examination Survey (NHANES) data showed non-Hispanic Asian Americans had greater sodium intake compared with non-Hispanic Blacks (3,630 vs 3,310 mg/day), and only 8% consumed the recommended amount of sodium/day (≤2,300 mg/day) compared with 13%, 16% and 12% of non-Hispanic Whites, non-Hispanic Blacks and Hispanics, respectively.12 While sodium policy in the US targets processed and packaged foods, the majority of sodium ingested in East Asian countries is added during cooking, or at the table in the form of soy sauce or other condiments.2,13
Understanding whether and how sources of sodium intake vary by race/ethnicity could inform the development of culturally appropriate, effective sodium reduction strategies. Public health strategies could refine approaches (ie, encouraging industry participation, sodium reduction targets for food manufacturers, nutrition label modifications, consumer education, and/or taxation on high-sodium foods) based on top dietary sources of sodium in target populations.14 Our study aimed to identify the top 10 food category sources of sodium and salt behaviors for Asian Americans compared with other racial/ethnic groups.
Methods
Study Design and Population
NHANES is a nationally representative, multi-stage complex survey designed to assess the health and nutritional status of the non-institutionalized, civilian US population. As detailed elsewhere,15 NHANES participants completed a household interview to collect demographic and general health information followed by a visit to a Mobile Examination Center for a physical examination, anthropometric measures, and a 24-hour dietary recall administered by a trained interviewer using the USDA-multiple pass method. Signed informed consent was obtained from all participants or their proxies.
The USDA Food and Nutrient Database for Dietary Studies (FNDDS) 2011-2012 was used to code dietary intakes and calculate nutrient intakes. Each food in the 24-hour dietary recall is assigned to one of more than 7,000 food codes. Nutrient values for FNDDS are from the USDA National Nutrient Database for Standard Reference.16 FNDDS food categories were linked to one What We Eat in America (WWEIA) category to analyze sodium intake in the previous 24 hours from food and beverages. The WWEIA classification scheme includes approximately 150 food categories and does not disaggregate into ingredients (ie, pizza vs cheese, tomatoes, etc.).17 Sodium estimates did not include adjustments for discretionary salt use, as salt added at the table or during cooking, in the average American diet is estimated to make up 6% and 5% of sodium intake, respectively.16,17
The 2011-2012 NHANES had a sample size of 9,756 and was the first wave to include an oversample of non-Hispanic Asian Americans.15 Participants were excluded if they were aged <18 years (n=3,892) or were missing the first dietary recall (n=788). The final analytic sample included 5,076 individuals.
Measures
Means and standard errors for sodium (mg), energy (kcal) and sodium density (mg/1,000kcal), a measure that accounts for differences in calories consumed, were calculated by race/ethnicity and food source.
To determine the top 10 dietary sources of sodium, population proportions (%) were calculated for each food category by summing the amount of sodium consumed within each category for all persons within each racial/ethnic group and dividing that by the sum of all sodium consumed for all foods for all persons within each racial/ethnic group multiplied by 100.18 Salt behaviors were determined by two questions that asked respondents to rate how often they add ordinary salt to their food at the table and how often they add ordinary salt/seasoned salt while cooking/preparing food.
Demographic variables included sex, age, race/ethnicity, education, poverty/income, and nativity. Race/ethnicity was divided into five categories: Hispanic, non-Hispanic White, non-Hispanic Black, non-Hispanic Asian and other (including mixed race) (hereafter referred to as Hispanic, White, Black, Asian American and other). Education was restricted to adults aged >25 years.
Statistical Analyses
Food categories were ranked based on population proportion and the top 10 are reported. Mean differences comparing Asian Americans to other race/ethnicities were calculated using t-tests. Tests were considered statistically significant if P<.05. Correction for multiple comparisons was not included given the small number of planned comparisons.19 Calculations were estimated using SAS-callable SUDAAN v.11.0.0 (RTI International, Research Triangle Park, NC) to adjust for the complex survey design. Sample weights accounted for the probability of selection, non-response, and day of the week of dietary recall.
Results
Demographic Characteristics
The analytic sample was 14.5% Hispanic (95%CI: 9.8, 20.9), 66.0% White (95%CI: 57.2, 73.9), 11.8% Black (95%CI: 7.5, 18.0), 5.1% Asian (95%CI: 3.7, 7.2), and 2.6% other (95%CI: 1.7, 3.8). Over half had more than a high school education; 29.9% had some college (95%CI: 26.8, 33.3) and 32.9% had a college degree or more (95%CI: 26.9, 39.5). The majority of the sample (82.9%) was US-born (95%CI: 78.3, 86.6) (Table 1).
Table 1. Demographic characteristics, NHANES 2011-12, n=5,076.
| Weighted na | n | % | 95% CI | ||
| Total | 233,250,000 | ||||
| Sex | |||||
| Male | 114,610,000 | 2,535 | 49.1 | (47.2, 51.1) | |
| Female | 118,640,000 | 2,541 | 50.9 | (48.9, 52.8) | |
| Age group | |||||
| 18-24 years | 32,784,000 | 757 | 14.1 | (9.7, 19.9) | |
| 25-44 years | 76,917,000 | 1,625 | 33.0 | (29.1, 37.1) | |
| 45-64 years | 84,170,000 | 1,662 | 36.1 | (33.1, 39.2) | |
| ≥65 years | 39,371,000 | 1,032 | 16.9 | (14.7, 19.3) | |
| Race/ethnicity | |||||
| Hispanic | 33,772,000 | 1,008 | 14.5 | (9.8, 20.9) | |
| Non-Hispanic White | 154,020,000 | 1,905 | 66.0 | (57.2, 73.9) | |
| Non-Hispanic Black | 27,442,000 | 1,366 | 11.8 | (7.5, 18.0) | |
| Non-Hispanic Asian | 11,999,000 | 639 | 5.1 | (3.7, 7.2) | |
| Other | 6,010,000 | 158 | 2.6 | (1.7, 3.8) | |
| Educationb | |||||
| <High school | 34,172,000 | 1,044 | 17.1 | (13.7, 21.1) | |
| High school | 40,354,000 | 904 | 20.1 | (16.9, 23.8) | |
| Some college | 60,019,000 | 1,210 | 29.9 | (26.8, 33.3) | |
| ≥College graduate | 65,857,000 | 1,158 | 32.9 | (26.9, 39.5) | |
| Household income (% federal poverty level) | |||||
| <200% FPL | 87,871,000 | 2,440 | 40.1 | (33.7, 46.7) | |
| 200%-399% FPL | 57,393,000 | 1,092 | 26.2 | (22.2, 30.6) | |
| ≥400% FPL | 74,105,000 | 1,146 | 33.8 | (28.1, 40.0) | |
| Nativity | |||||
| US-born | 193,230,000 | 3,636 | 82.9 | (78.3, 86.6) | |
| Foreign-born | 39,969,000 | 1,437 | 17.1 | (13.4, 21.7) | |
a. Rounded to the nearest 1,000.
b. Restricted to aged >25 years.
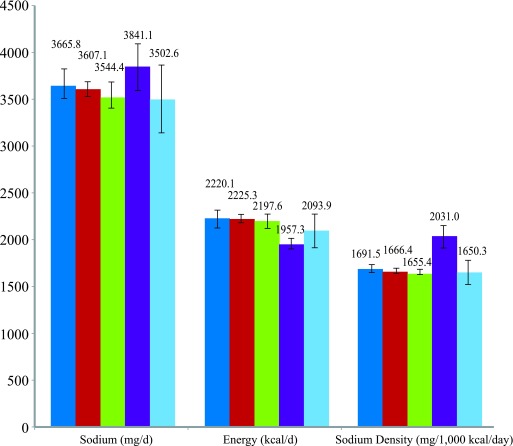
Mean Sodium, Energy and Sodium Density
Mean absolute sodium consumption did not vary significantly by race/ethnicity; however, mean differences in energy and sodium density by race/ethnicity were observed (Figure 1). Asian Americans consumed the fewest calories (1957.3, 95%CI: 1900.4, 2014.2) compared with other racial/ethnic groups (Hispanics: 2220.1, 95%CI: 2124.2, 2316.0; Whites 2225.3, 95%CI: 2179.4, 2271.2; and Blacks 2197.6, 95%CI: 2121.2, 2274.0; P for all <.01). Yet, sodium density (mg/1000kcal/day) was significantly higher among Asian Americans (2031.1, 95%CI: 1911.2, 2150.9) compared with Hispanics (1691.6, 95%CI: 1648.6, 1734.5), Whites (1666.5, 95%CI: 1638.0, 1694.9), Blacks (1655.5, 95%CI: 1627.2, 1683.7) and other (1650.4, 95%CI: 1520.9, 1779.8) (P for all<.01).
Figure 1. Blue, Hispanic; red, Non-Hispanic White; green, Non-Hispanic Black; purple, Non-Hispanic Asian; light blue, Other.
Food Category Sources of Sodium
Half of the sodium consumed by Asian Americans was from the top 10 food categories, compared with 43.6% for Hispanics, 39.0% for Whites, 36.8% for other, and 36.0% for Blacks (Table 2). Three food categories ranked in the top ten sources of sodium for every race/ethnicity: soups; chicken, whole pieces; and yeast breads. Four food categories were a top sodium source for Hispanics, Whites, Blacks, and other, but not Asian Americans: cold cuts and cured meats; meat mixed dishes; eggs and omelets; and cheese. There were six food categories that only appeared in the top 10 sources for Asians: rice; stir-fry and soy-based mixtures; fish; fried rice and lo/chow mein; soy-based condiments; and dips, gravies and other sauces.
Table 2. Ranked population proportions of sodium consumed from food categories by race/ethnicity, NHANES 2011-12, n=5076.
| Hispanic | White | Black | Asian | Other | |||||||||||
| FC | % Total (SE) | %a | FC | % Total (SE) | %a | FC | % Total (SE) | %a | FC | % Total (SE) | %a | FC | % Total (SE) | %a | |
| 1 | Burritos and tacos | 8.8 (1.8) | 8.8 | Pizza | 5.9 (.8) | 5.9 | Chicken, whole pieces | 6.6 (.2) | 6.6 | Soups | 16.0 (2.0) | 16.0 | Burritos and tacos | 5.0 (2.3) | 5.0 |
| 2 | Soups | 5.9 (.8) | 14.6 | Cold cuts and cured meats | 5.6 (.6) | 11.4 | Pizza | 4.4 (.7) | 11.0 | Rice | 9.0 (.3) | 25.0 | Yeast breads | 4.9 (.6) | 9.8 |
| 3 | Pizza | 4.4 (1.0) | 19.0 | Yeast breads | 4.5 (.2) | 15.9 | Cold cuts and cured meats | 4.2 (.4) | 15.1 | Yeast breads | 3.9 (.5) | 28.9 | Chicken, whole pieces | 4.0 (1.0) | 13.8 |
| 4 | Chicken, whole pieces | 4.2 (.6) | 23.3 | Soups | 4.0 (.5) | 20.0 | Yeast breads | 4.0 (.2) | 19.1 | Stir-fry and soy-based sauces | 3.5 (.6) | 32.4 | Cold cuts and cured meats | 3.8 (1.1) | 17.6 |
| 5 | Other Mexican mixed dishes | 3.9 (.8) | 27.1 | Cheese | 3.6 (.4) | 23.6 | Soups | 3.2 (.4) | 22.4 | Fish | 3.4 (.3) | 35.7 | Soups | 3.6 (1.1) | 21.2 |
| 6 | Cold cuts and cured meats | 3.7 (.4) | 30.8 | Meat mixed dishes | 3.6 (.6) | 27.1 | Pasta mixed dishes, no mac/ch | 3.1 (.5) | 25.4 | Chicken, whole pieces | 3.3 (.4) | 39.0 | Burgers | 3.5 (1.9) | 24.7 |
| 7 | Meat mixed dishes | 3.5 (.5) | 34.3 | Burritos and tacos | 3.4 (.3) | 30.6 | Cheese | 3.0 (.4) | 28.5 | Fried rice and lo/chow mein | 2.9 (.5) | 41.9 | Meat mixed dishes | 3.5 (1.4) | 28.2 |
| 8 | Eggs and omelets | 3.3 (.3) | 37.6 | Pasta mixed dishes, no mac/ch | 2.9 (.4) | 33.5 | Eggs and omelets | 2.7 (.2) | 31.2 | Soy-based condiment | 2.8 (.5) | 44.7 | Eggs and omelets | 3.2 (.5) | 31.3 |
| 9 | Yeast breads | 3.2 (.3) | 40.9 | Chicken, whole pieces | 2.8 (.4) | 36.3 | Meat mixed dishes | 2.6 (.4) | 33.8 | Pizza | 2.8 (.5) | 47.4 | Pasta mixed dishes, no mac/ch | 3.0 (1.4) | 34.3 |
| 10 | Cheese | 2.7 (.3) | 43.6 | Eggs and omelets | 2.7 (.2) | 39.0 | Burgers | 2.3 (.3) | 36.0 | Dips, gravies, other sauces | 2.6 (.6) | 50.0 | Cheese | 2.5 (.5) | 36.8 |
a. Cumulative %.
FC, food category; mac/ch, macaroni and cheese
Salt Behaviors
Overall, 57.3% (95%CI: 51.4%, 63.1%) of Asian Americans reported rarely adding salt at the table, significantly more than Whites (41.7%, 95%CI: 37.5%, 46.0%; P<.01), Blacks (48.5%, 95%CI: 42.7%, 54.4%; P=.03) and other (48.3%, 95%CI: 41.4%, 55.3%; P=.01). By contrast, 57.4% (95%CI: 52.4%, 62.3%) of Asian Americans reported using salt in preparation ‘very often,’ which is significantly higher than reported by Whites and Blacks (P for both<.01). (Table 3)
Table 3. Proportions of salt behaviors by race/ethnicity, NHANES 2011-12.
| Hispanic | White | Black | Asian American (ref) | Other | ||||||
| % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | |
| Salt added at table, n=3,331 | ||||||||||
| Rarely | 52.8 | (47.3, 58.1) | 41.7a | (37.5, 46.0) | 48.5a | (42.7, 54.4) | 57.3 | (51.4, 63.1) | 48.3a | (41.4, 55.2) |
| Occasionally | 26.9 | (22.0, 32.5) | 38.1a | (32.8, 43.7) | 29.9 | (25.5, 34.7) | 26.2 | (21.5, 31.5) | 27.6 | (18.9, 38.2) |
| Very often | 20.3 | (16.0, 25.5) | 20.3 | (15.6, 25.8) | 21.5 | (17.7, 26.0) | 16.5 | (11.9, 22.4) | 24.2 | (16.1, 34.6) |
| Salt used in preparation, n=4,978 | ||||||||||
| Never | 4.4a | (3.2, 6.0) | 8.6a | (6.9, 10.6) | 7.5a | (5.9, 9.5) | 2.4 | (1.7, 3.5) | 7.7b | (3.3, 16.9) |
| Rarely | 15.2a | (12.4, 18.5) | 20.9a | (18.9, 23.1) | 14.9a | (12.0, 18.4) | 10.2 | (7.3, 14.1) | 16.8b | (7.8, 32.4) |
| Occasionally | 29.8 | (25.7, 34.3) | 39.7a | (36.2, 43.3) | 32.6 | (28.5, 37.1) | 30.0 | (26.7, 33.4) | 33.8b | (23.6, 45.8) |
| Very often | 50.6 | (46.1, 55.1) | 30.8a | (26.7, 35.4) | 44.9a | (42.1, 47.8) | 57.4 | (52.4, 62.3) | 41.8ab | (28.7, 56.1) |
a. Significant at P<.05 compared with Asian.
b. Estimate’s relative standard error (a measure of estimate precision) is >30% or the sample size is <50, making the estimate potentially unreliable.
Discussion
This study identified the top 10 dietary sources of sodium and salt behaviors among Asian Americans compared with other racial/ethnic groups. While there were differences in the food category rankings for all racial/ethnic groups, the biggest differences were observed among Asian Americans. The top 10 sources account for a greater proportion of dietary sodium for Asian Americans compared with other racial/ethnic groups – bearing implication that activities targeting very few products could have a large impact on sodium intakes in this group. Of the 10 food categories most frequently cited by Asian Americans, six were not ranked in the top 10 of other racial/ethnic groups, including dietary staples for Asian Americans such as rice, fish and soy-based condiments.
This analysis is aligned with local and national activity around nutrition improvements to reduce chronic disease risk. Over the last decade, the NYC Health Department introduced innovative programming nationally and locally to improve adult diets. One example is the National Salt Reduction Initiative, a national effort to reduce population sodium intake through corporate commitments to lowering sodium in packaged and restaurant foods.20 Recent results demonstrate modest success in decreasing sodium content in these products, as well as decreases of sales-weighted mean sodium density (by 6.8%, P<.001) in nearly half of all food categories (43%).21 Companies continue commitments to reducing sodium in foods; PepsiCo recently announced it will have at least three-quarters of its global foods portfolio volume restricted to ≤1.3mg of sodium/calorie.22 In 2016, the US Food and Drug Administration announced a voluntary sodium reduction strategy for the food industry.23 Local sodium reduction strategies include introduction of nutrition standards at city agencies,24 educational media campaigns, and multiple efforts by community-based and other national organizations including the American Heart Association.23,25-27
While increasing prioritization has been placed on reducing average population sodium intake,5-7,28 limited evidence to monitor intake suggests no change or increases, which may in part be due to policies that, by design, may not reach all sub-populations. In the United States, in a systematic review of 38 studies published from 1957 to 2003 reporting adult 24-hour urinary sodium values, authors estimated a mean sodium excretion of 3,526 mg/day, and reported that sodium intake has not significantly changed over time overall or in sex/race subgroups.29 Changes in sodium intake over time have also been reported using repository-based analyses of spot urine samples and application of recalibration equations to estimate 24-hour excretion in NHANES.30 Between 1988 and 2010, estimated 24-hour urinary sodium excretion increased by 130mg/day; however, increasing BMI over the same time period likely contributed to these increases.30
Current efforts for reducing population sodium intake are geared toward reformulation and increasing consumer awareness of sodium in packaged and restaurant foods. However, the reach to Asian Americans, who have high sodium intakes,12 may be limited for two reasons. First, the primary sources of sodium consumed in Asian Americans appear to be salt added during cooking, not from packaged and restaurant foods;13,31,32 and second, Asian Americans may retain traditional dietary practices post-migration to America.33,34 Examination of Asian American demographics in NHANES reveals that NHANES appears to have recruited one portion of this population: highly educated, high-income earners35,36 – with these individuals likely being more acculturated,37 meaning they have adopted more US cultural practices. This implies that even among more acculturated individuals, dietary practices are retained. Further, data suggest increased consumption of traditional ‘festival foods’ (high in carbohydrates, animal protein, sugar and fat) as opposed to the traditional idea of a ‘Westernization of diet’ among Asian Americans and other immigrant groups as an explanatory factor in increased cardio-metabolic risk in these populations.33 Due to acculturative stress, immigrants may seek these foods as a source of comfort and maintenance of ethnic identity.33
Our results offer preliminary support for these patterns, and demonstrate the need for approaches that target sodium sources specific to Asian Americans, both through policy and coordinated programming. Strategies similar to those in China, Japan and South Korea, which focus on food preparation and education rather than product reformulation25 may be an additional way to reach Asian Americans. This offers an opportunity to improve sodium reduction initiatives by incorporating public health strategies and dietary messaging that are more likely to impact subgroups with the highest sodium intake levels.
Strengths and Limitations
Strengths of this study include a sample representative of the US non-institutionalized population and an oversample of Asian Americans allowing for comparisons of Asian Americans sources and salt behaviors to other racial/ethnic groups. Focusing on Asian Americans compared with other racial/ethnic groups and including sodium density helps us to better understand factors accounting for high sodium consumption across racial/ethnic groups.
There are several limitations that should be noted. A single dietary recall provided a preliminary snapshot of two years of a four-year NHANES cycle to include a representative subsample of Asian Americans.38 Furthermore, the Asian Americans subsample was not large enough to distinguish between subpopulations (ie, Chinese, Indian, Filipino), potentially masking disparities by ethnicity and country of origin among Asian Americans.39,40 Data from Asia indicates that high sodium intake exists across Asian subgroups.11,32 Although rigorous methods were used for dietary recall that allow for incorporation of diverse dietary patterns, a lack of representativeness for ethnic diets in FNDDS food codes may have resulted in misclassification, and data are subject to measurement error (ie, recall and coding errors). A validation study using 24-hour urinary sodium as the reference measure found differential misreporting of sodium intake by sex and BMI, but not race/ethnicity, although the sample was not large enough to allow for an Asian American sub-category.41 Sodium added at the table and from supplements and medicines are not included, which may result in underestimations of consumption.42 Lastly, it is unclear whether the Asian Americans sampled in NHANES are representative of all Asian Americans; NHANES recruited highly educated, high income earners37 – though a stark bimodal income distribution exists for Asian Americans.35 By potentially missing less acculturated individuals, sodium intakes may not be generalizable to all Asian Americans.
Conclusion
This analysis highlights racial/ethnic differences in top sources of sodium, which is important for developing targeted efforts to reduce sodium among high-risk subpopulations. Public health strategies that encourage salt reduction in food preparation and condiments in Asian Americans have the potential to shift the overall population sodium intake distribution downwards.
Acknowledgments
This research was supported in part by P60MD000538 from the National Institutes of Health (NIH) National Institute on Minority Health and Health Disparities, U48DP005008 and U58DP005621 from the Centers for Disease Control and Prevention (CDC) and UL1TR001445 from NCATS/NIH. The contents of this publication are solely the responsibility of the authors and do not necessarily represent the official views of the NIH and CDC. NHANES 2011-2012 was approved by the National Center for Health Statistics (NCHS) Research Ethics Review Board (Protocol #2011-17). Signed informed consent was obtained from all NHANES participants or their proxies in accordance with section 308(d) of the Public Health Service Act (42 U.S.C. 242m).
References
- 1.National Vital Statistics Reports, Deaths: Final Data for 2009.60(3). [PubMed]
- 2. Brown IJ, Tzoulaki I, Candeias V, Elliott P. Salt intakes around the world: implications for public health. Int J Epidemiol. 2009;38(3):791-813. 10.1093/ije/dyp139 [DOI] [PubMed] [Google Scholar]
- 3. U.S. Department of Health and Human Services, U.S. Department of Agriculture 2015-2020 Dietary Guidelines for Americans. 2015; 8th Edition: Last accessed May 25, 2017 from http://health.gov/dietaryguidelines/2015/guidelines/.
- 4. Jackson SL, King SM, Zhao L, Cogswell ME Prevalence of excess sodium intake in the United States - NHANES, 2009-2012. MMWR Morb Mortal Wkly Rep. 2016;64(52):1393- 1397. https://doi.org/ 10.15585/mmwr. mm6452a1. PMID:26741238. [DOI] [PubMed]
- 5. Gunn JP, Kuklina EV, Keenan NL, Labarth DR; Centers for Disease Control and Prevention (CDC) . Sodium intake among adults - United States, 2005-2006. MMWR Morb Mortal Wkly Rep. 2010;59(24):746-749. [PubMed] [Google Scholar]
- 6. U.S. Department of Health and Human Services Healthy People 2020. Last accessed September 10, 2016 from http://www.healthypeople.gov/2020/default.aspx.
- 7. Institutes of Medicine (US) Strategies to Reduce Sodium Intake in the United States. Washington, DC; 2010. [Google Scholar]
- 8. Ganda OP, Fonseca VA. Salt sensitivity, insulin resistance, and public health in India. Endocr Pract. 2010;16(6):940-944. 10.4158/EP10103.OR [DOI] [PubMed] [Google Scholar]
- 9. Katsuya T, Ishikawa K, Sugimoto K, Rakugi H, Ogihara T. Salt sensitivity of Japanese from the viewpoint of gene polymorphism. Hypertens Res. 2003;26(7):521-525. 10.1291/hypres.26.521 [DOI] [PubMed] [Google Scholar]
- 10. Vollmer WM, Sacks FM, Ard J, et al. ; DASH-Sodium Trial Collaborative Research Group . Effects of diet and sodium intake on blood pressure: subgroup analysis of the DASH-sodium trial. Ann Intern Med. 2001;135(12):1019-1028. 10.7326/0003-4819-135-12-200112180-00005 10.7326/0003-4819-135-12-200112180-00005 [DOI] [PubMed] [Google Scholar]
- 11. Powles J, Fahimi S, Micha R, et al. ; Global Burden of Diseases Nutrition and Chronic Diseases Expert Group (NutriCoDE) . Global, regional and national sodium intakes in 1990 and 2010: a systematic analysis of 24 h urinary sodium excretion and dietary surveys worldwide. BMJ Open. 2013;3(12):e003733. 10.1136/bmjopen-2013-003733 10.1136/bmjopen-2013-003733 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Bailey RL, Parker EA, Rhodes DG, et al. . Estimating sodium and potassium intakes and their ratio in the American diet: data from the 2011-2012 NHANES. J Nutr. 2016;146(4):745-750. 10.3945/jn.115.221184 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Anderson CA, Appel LJ, Okuda N, et al. . Dietary sources of sodium in China, Japan, the United Kingdom, and the United States, women and men aged 40 to 59 years: the INTERMAP study. J Am Diet Assoc. 2010;110(5):736-745. 10.1016/j.jada.2010.02.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Eyles H, Shields E, Webster J, Ni Mhurchu C. Achieving the WHO sodium target: estimation of reductions required in the sodium content of packaged foods and other sources of dietary sodium. Am J Clin Nutr. 2016;104(2):470-479. 10.3945/ajcn.115.125146 10.3945/ajcn.115.125146 [DOI] [PubMed] [Google Scholar]
- 15. Johnson CL, Dohrmann SM, Burt VL, Mohadjer LK. National Health and Nutrition Examination Survey: Sample design, 2011- 2014. National Center for Health Statistics; 2014. [PubMed] [Google Scholar]
- 16. U.S. Department of Agriculture Agricultural Research Service USDA Food and Nutrient Database for Dietary Studies 2011-2012. 2014.
- 17. U.S. Department of Agriculture Agricultural Research Service What We Eat in America Food Categories 2011-2012. 2015. Last accessed August 4, 2016 from http://www.ars.usda.gov/nea/bhnrc/fsrg.
- 18. Krebs-Smith SM, Kott PS, Guenther PM. Mean proportion and population proportion: two answers to the same question? J Am Diet Assoc. 1989;89(5):671-676. [PubMed] [Google Scholar]
- 19. Streiner DL, Norman GR. Correction for multiple testing: is there a resolution? Chest. 2011;140(1):16-18. 10.1378/chest.11-0523 10.1378/chest.11-0523 [DOI] [PubMed] [Google Scholar]
- 20. National Salt Reduction Initiative Last accessed December 5, 2016 from http://www.nyc.gov/health/salt.
- 21. Curtis CJ, Clapp J, Niederman SA, Ng SW, Angell SY. US Food Industry Progress During the National Salt Reduction Initiative: 2009-2014. Am J Public Health. 2016;106(10):1815-1819. 10.2105/AJPH.2016.303397 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.PepsiCo Launches 2025 Sustainability Agenda Designed to Meet Changing Consumer and Societal Needs [press release]. 2016. Last accessed May 25, 2017 from http://www.pepsico.com/live/pressrelease/pepsico-launches-2025-sustainability-agenda-designed-to-meetchanging-consumer-a10172016
- 23. US Food and Drug Administration , Voluntary Sodium Reduction Targets Draft Guidance (video). Last accessed May 25, 2017 from http://www.fda.gov/Food/NewsEvents/WorkshopsMeetingsConferences/ucm505849.htm
- 24. Lederer A, Curtis CJ, Silver LD, Angell SY. Toward a healthier city: nutrition standards for New York City government. Am J Prev Med. 2014;46(4):423-428. 10.1016/j.amepre.2013.11.011 [DOI] [PubMed] [Google Scholar]
- 25. Trieu K, Neal B, Hawkes C, et al. Salt Reduction Initiatives around the World - A Systematic Review of Progress towards the Global Target. PLoS One. 2015;10(7):e0130247. https://doi.org/ 10.1371/journal. pone.0130247. PMID:26201031. [DOI] [PMC free article] [PubMed]
- 26. Korean Community Services of New York , Healthy Eating. Last accessed August 5, 2016 from http://www.kcsny.org/en/healthy-eating/.
- 27. American Heart Association , Sodium & Salt (web page). Last accessed May 25, 2017 from http://www.heart.org/HEARTORG/Healthy-Living/HealthyEating/Nutrition/Sodium-and-Salt_UCM_303290_Article.jsp
- 28.Global Strategy on Diet, Physical Activity and Health: Population sodium reduction strategies. Last accessed December 4, 2014 from http://www.who.int/dietphysicalactivity/reducingsalt/en/
- 29. Bernstein AM, Willett WC. Trends in 24-h urinary sodium excretion in the United States, 1957-2003: a systematic review. Am J Clin Nutr. 2010;92(5):1172-1180. 10.3945/ajcn.2010.29367 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Pfeiffer CM, Hughes JP, Cogswell ME, et al. . Urine sodium excretion increased slightly among U.S. adults between 1988 and 2010. J Nutr. 2014;144(5):698-705. 10.3945/jn.113.187914 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Lee HS, Duffey KJ, Popkin BM. Sodium and potassium intake patterns and trends in South Korea. J Hum Hypertens. 2013;27(5):298-303. 10.1038/jhh.2012.43 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Ravi S, Bermudez OI, Harivanzan V, et al. . Sodium intake, blood pressure, and dietary sources of sodium in an adult South Indian population. Ann Glob Health. 2016;82(2):234-242. 10.1016/j.aogh.2016.02.001 [DOI] [PubMed] [Google Scholar]
- 33. Azar KM, Chen E, Holland AT, Palaniappan LP. Festival foods in the immigrant diet. J Immigr Minor Health. 2013;15(5):953-960. 10.1007/s10903-012-9705-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Lee YH, Lee J, Kim MT, Han HR. In-depth assessment of the nutritional status of Korean American elderly. Geriatr Nurs. 2009;30(5):304-311. 10.1016/j.gerinurse.2009.02.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Ramakrishnan K, Ahmad FZ State of Asian Americans and Pacific Islanders: Income and Poverty. 2014. Last accessed May 19, 2015 from https://cdn.americanprogress.org/wpcontent/uploads/2014/08/AAPI-IncomePoverty.pdf.
- 36. United States Department of Labor, The Economic Status of Asian Americans and Pacific Islanders 2016. Last accessed October 10, 2016 from https://www.dol.gov/_sec/media/reports/AsianLaborForce/2016AsianLaborForce.pdf.
- 37. Haughton CF, Wang ML, Lemon SC Racial/ ethnic disparities in meeting 5-2-1-0 recommendations among children and adolescents in the United States. J Pediatr. 2016;175:188- 194.e1. https://doi.org/ 10.1016/j. jpeds.2016.03.055. PMID:27112040. [DOI] [PMC free article] [PubMed]
- 38. Centers for Disease Control and Prevention, National Center for Health Statistics, Division of Health and Nutrition Examination Surveys National Health and Nutrition Examination Survey: Analytic Guidelines, 2011-2012. 2013.
- 39. Holland AT, Palaniappan LP. Problems with the collection and interpretation of Asian-American health data: omission, aggregation, and extrapolation. Ann Epidemiol. 2012;22(6):397-405. 10.1016/j.annepidem.2012.04.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Islam NS, Khan S, Kwon S, Jang D, Ro M, Trinh-Shevrin C. Methodological issues in the collection, analysis, and reporting of granular data in Asian American populations: historical challenges and potential solutions. J Health Care Poor Underserved. 2010;21(4):1354-1381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Mercado CI, Cogswell ME, Valderrama AL, et al. . Difference between 24-h diet recall and urine excretion for assessing population sodium and potassium intake in adults aged 18-39 y. Am J Clin Nutr. 2015;101(2):376-386. 10.3945/ajcn.113.081604 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Rhodes DG, Murayi T, Clemens JC, Baer DJ, Sebastian RS, Moshfegh AJ. The USDA Automated Multiple-Pass Method accurately assesses population sodium intakes. Am J Clin Nutr. 2013;97(5):958-964. 10.3945/ajcn.112.044982 10.3945/ajcn.112.044982 [DOI] [PubMed] [Google Scholar]