Abstract
Background
Differences in healthcare utilization after stroke may partly explain race or gender differences in stroke outcomes and identify factors that might reduce post-acute stroke care costs.
Aim
To examine systematic differences in Medicare claims for healthcare utilization after hospitalization for ischemic stroke in a United States (US) population-based sample.
Methods
Claims were examined over a 6-month period after hospitalization for 279 ischemic stroke survivors 65 years or older from the REasons for Geographic and Racial Differences in Stroke (REGARDS) study. Statistical analyses examined differences in post-acute healthcare utilization, adjusted for pre-stroke utilization, as a function of race (African American vs. White), gender, age, stroke belt residence, income, Medicaid dual-eligibility, Charlson comorbidity index, and whether the person lived with an available caregiver.
Results
After adjusting for covariates, women were more likely than men to receive home health care and to use emergency department services during the post-acute care period. These effects were maintained even after further adjustment for acute stroke severity. African Americans had more home health care visits than Whites among patients who received some home health care. Having a co-residing caregiver was associated with reduced acute hospitalization length of stay and fewer post-acute emergency department and primary care physician visits.
Conclusions
Underutilization of healthcare after stroke does not appear to explain poorer long-term stroke outcomes for women and African Americans in this epidemiologically-derived sample. Caregiver availability may contribute to reduced formal care and cost during the post-acute period.
Keywords: Stroke, Medicare, Healthcare utilization, Epidemiology, Population-based, Caregiving
Multiple studies in the United States (US) have found that African Americans experience more severe strokes and recover less completely than Whites,1–4 and that women have poorer functional outcomes after stroke than men.3,5,6 Most of the previous studies on post-acute care and outcome disparities after stroke have identified stroke survivors after their stroke events from clinical registries. Although clinical samples have important strengths, the enrolled patients from such studies may have more impairments and other differences from stroke survivors detected prospectively in epidemiological studies. Methodological differences in sample composition and the control of possible confounders, such as the availability of a co-residing caregiver, are especially important to consider when examining potential race- or gender-based disparities.
The economic costs of acute and post-acute healthcare for stroke in the US are projected to more than double over the next few decades.7 Because most stroke survivors are over age 65, most of this projected increasing cost is expected to be covered by the federal Medicare insurance program. Systematic studies of healthcare utilization after stroke using population-based samples are, therefore, needed to identify factors that may contribute to positive outcomes and to suggest reimbursement adjustments or other cost-saving innovations. The present study used claims data to examine demographic differences in post-acute healthcare utilization over a 6 month-period after hospitalization for ischemic stroke. All participants had traditional fee-for-service Medicare coverage, which is the most common form of health insurance for US citizens over age 65 and provides payments for individual services as opposed to bundled services.
Methods
Participants
Data were extracted from participants enrolled in the national REGARDS study that was designed to identify the causes of regional and racial disparities in stroke mortality. Potential participants were randomly sampled from a commercially available nationwide list of postal addresses and telephone numbers. Eligible participants had to be 45 or more years of age at enrollment and self-identify as either African American or White. African Americans and residents of the “stroke belt” (Southeastern states of the US) were oversampled by design. A population-based sample of 30,239 participants was therefore enrolled into the REGARDS study from 2003 until 2007 from the 48 contiguous States of the US. After an initial telephone interview, participants were examined in their homes and provided written informed consent that included consent to seek and obtain medical records and insurance claims related to possible stroke events. Additional details about the recruitment, enrollment, and assessment procedures for REGARDS have been described in more detail elsewhere.8,9 All procedures were approved by the institutional review boards of participating institutions.
The 279 REGARDS participants who selected for the present analyses were hospitalized for an ischemic stroke between July 2004 and June 2013, were 65 or more years of age at the time of stroke, survived for at least 6 months after the stroke, and had traditional fee-for-service Medicare coverage for 13 or more continuous months around the stroke date. For participants with multiple ischemic stroke hospitalizations, only the first event that met Medicare coverage criteria was included.
Procedures
Descriptive information (date of birth, education, income, marital status) were obtained during a computer-assisted telephone interview (CATI) conducted at enrollment into REGARDS. CATI questions also collected information on household composition and the availability of a potential family caregiver.
Follow-up CATIs are conducted every 6 months to inquire about hospitalizations and other incidents (e.g., symptoms, emergency room visits) that might indicate possible stroke events. Medical records are then retrieved, and all strokes examined in this report were confirmed to be ischemic stroke events by an adjudication committee consisting of neurologists and other physician adjudicators.9 Acute hospitalization records were also evaluated to obtain a retrospective assessment of stroke severity at discharge based on the National Institutes of Health Stroke Scale (NIHSS) for 249 (89%) of the patients.10
Measures Extracted from Medicare Claims Files
Multiple Medicare claims files were linked for each patient by a unique beneficiary identification number. Brief descriptions of the healthcare utilization measures extracted from these files are provided here. More detailed descriptions are available in a Supporting Information Table S1.
Charlson Comorbidity Index
The index was calculated using valid ICD 9 diagnosis codes from the inpatient, outpatient, and physician claim (carrier) files for the year preceding the stroke. These codes were then mapped to seventeen comorbid conditions, weights were assigned, and the index was calculated.11,12
Medicaid Dual-Eligibility Status
Patients with severely limited financial resources may also be eligible for State-sponsored Medicaid assistance. Participant who received such assistance during the month of the stroke or at any point in the 6 months after stroke were coded as dual eligible.
Inpatient Rehabilitation Facility (IRF) and Skilled Nursing Facility (SNF) Admissions
Admissions to an IRF or a SNF were identified from the inpatient base claim files and the SNF base claim files, respectively.
Lengths of Stay
Acute hospitalizations up to 15 days after the stroke event and admissions to an IRF were identified from the inpatient base claim file. The number of days between admission and discharge was calculated for the acute hospitalization length of stay. For IRF and SNF admissions, the duration in days was calculated from the difference in days between the first and last day in these facilities. Multiple adjacent claims with dates of admission within one day of a previous discharge date were combined into one continuous record.
Outpatient Physician Visits
Provider specialty codes were examined from outpatient and physician claim files to determine the number of visits to all physicians, to primary care physicians, and to neurology specialty care.
Home Health Agency (HHA) Visits
The number of HHA visits were extracted from the HHA revenue file. Each revenue center code represents 15 minutes (0.25 hours) of service.
Physical Therapy (PT), Occupational Therapy (OT) and Speech and Language Pathology (SLP)
Hours of therapy were calculated from revenue center codes for IRF, SNF, outpatient, and HHA files. Summing the total number of visits and dividing by 4 gives hours of each type of therapy.
Emergency Room (ER) Visits
The number of ER visits was calculated by examining the relevant revenue center codes in both the inpatient and outpatient files.
Statistical Analysis
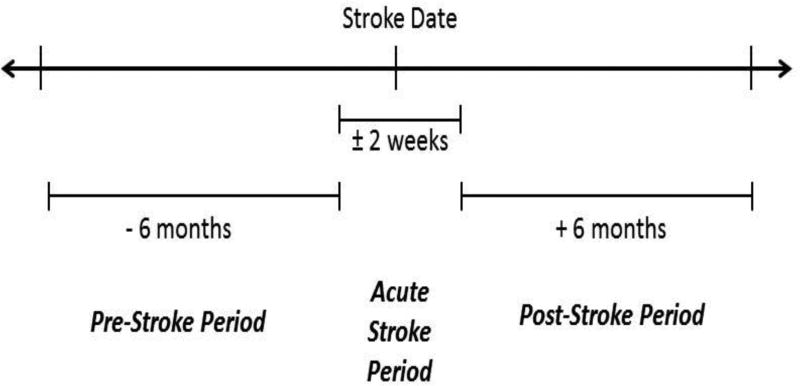
The primary goals were to examine demographic predictors of changes in healthcare utilization from before the index stroke event to the 6-month post-acute period after stroke. For many measures, utilization frequently occurred before the stroke event, and a pre-stroke utilization measure for the 6-month period before stroke was used as a covariate of post-stroke utilization. Figure 1 illustrates the definition of these periods and the overall 13-month time period for the analyses.
Figure 1.
Timeline of Pre-Stroke, Acute Stroke, and Post-Stroke Periods.
Our general analytic strategy was to examine each utilization measure in two complementary analyses. First, a binary logistic regression analysis was used to examine the predictors of having any (versus none) of a certain type of utilization (e.g., inpatient rehabilitation, HHA) after stroke. Second, among the subset of participants who had some utilization of a particular type, an analysis of covariance was used to examine differences in the amount of care received (e.g., number of days of inpatient rehabilitation, HHA visits). The primary predictor variables in both models were race (African American vs. White) and gender. Other predictors/covariates included the pre-stroke utilization measure, age, stroke belt residence (yes vs. no), income at the time of REGARDS enrollment (>= $35,000 per year, < $35,000 per year, missing), whether the person lived with an available caregiver at REGARDS enrollment, pre-stroke Charlson comorbidity index, and Medicaid dual-eligibility status. In addition, supplemental analyses were conducted that added the NIHSS stroke severity score at discharge as an additional covariate for the 248 patients for whom this score was available.
Results
Descriptive Information
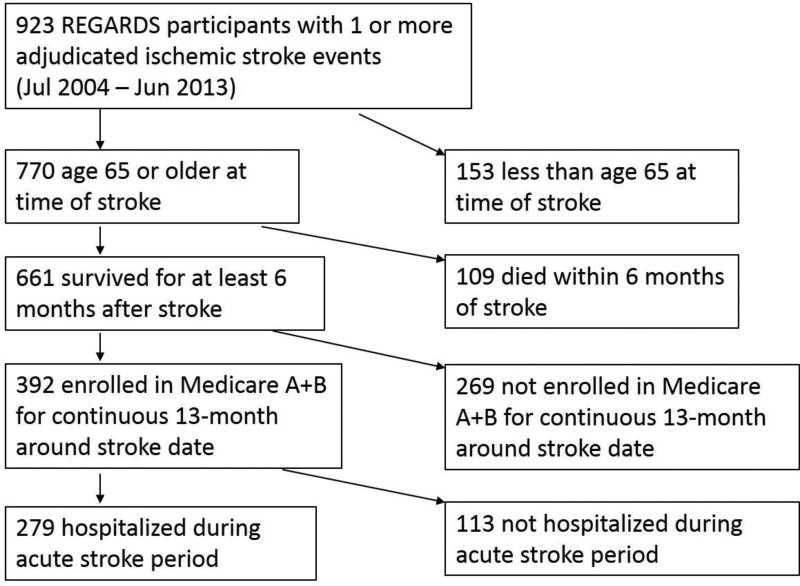
Figure 2 summarizes the selection criteria that resulted in an analytic sample of 279 stroke survivors from the 923 REGARDS participants who experienced an adjudicated ischemic stroke during the study period. Among the 661 stroke survivors who were 65 or more years of age, 392 (59%) had traditional fee-for-service Medicare coverage (Medicare A+B) throughout the 13-month analytic period. These participants were more likely to be White (66% vs. 49%) and male (54% vs. 34%) than participants who were not continuously enrolled in traditional Medicare (ps < .05).
Figure 2.
Flowchart of Participant Exclusions.
Descriptive data for the 279 patients included in the present analyses are summarized in Table 1. There were more men among the White than African American stroke survivors (57.9% vs. 42.6%, p = .014), so further race and gender comparisons on other descriptive variables were adjusted for this association. African Americans were significantly younger, less likely to be married, less likely to reside in the stroke belt, had lower incomes, higher Charlson comorbidity scores, and were more likely to be dual-eligible than Whites (all ps < .05). Similarly, women had lower incomes, were less likely to be married, less likely to be living with an available caregiver, and more likely to be dual-eligible than men (all ps < .01). No significant differences were found by either race or gender on the length of stay of acute stroke hospitalization.
Table 1.
Descriptive Information by Race and Gender
| African Americans | Whites | |||
|---|---|---|---|---|
|
| ||||
| Variable | Men | Women | Men | Women |
|
| ||||
| N | 43 | 58 | 103 | 75 |
|
| ||||
| Age at Stroke (M ± SD) | 73.7 ± 6.2 | 74.2 ± 6.0 | 76.8 ± 6.3 | 77.8 ± 6.1 |
|
| ||||
| Stroke belt residence – Yes (N, %) | 22, 51.2 | 31, 53.5 | 66, 64.1 | 54, 72.0 |
|
| ||||
| Income > $35,000 (N, %) | 15, 34.9 | 11, 19.0 | 58, 56.3 | 17, 22.7 |
|
| ||||
| Marital Status – Married (N, %) | 31, 72.1 | 13, 22.4 | 88, 85.4 | 20, 26.7 |
|
| ||||
| Live with available caregiver – Yes (N, %) | 25, 58.1 | 6, 10.3 | 71, 68.9 | 15, 20.0 |
|
| ||||
| Charlson comorbidity Index (M ± SD) | 3.5 ± 2.1 | 3.4 ± 2.3 | 2.7 ± 1.8 | 2.6 ± 1.9 |
|
| ||||
| Medicaid dual-eligibility | ||||
| Yes (N, %) | 5, 11.6 | 23, 39.7 | 7, 6.8 | 12, 16.0 |
| No (N, %) | 38, 88.4 | 35, 60.3 | 96, 93.2 | 63, 84.0 |
|
| ||||
| Interval between enrollment date and date of stroke – Years (M ± SD) | 3.8 ± 2.2 | 3.9 ± 2.4 | 4.0 ± 2.4 | 3.5 ± 2.1 |
|
| ||||
| Acute hospitalization length of stay (M ± SD) | 4.7 ± 3.3 | 5.5 ± 4.1 | 4.6 ± 4.6 | 5.0 ± 3.5 |
Descriptive analyses of post-acute care patterns indicated that 27.6% of the 279 patients were admitted to an IRF, 19.7% were admitted to a SNF, and 34.4% received HHA care. Only 12 patients (4.3%) received all 3 types of post-acute care, whereas 132 patients (47.3%) did not receive any of these 3 types of post-acute care.
Race and Gender Differences in Post-Acute Healthcare Utilization
The statistical tests of possible race and gender effects from the multivariable logistic regression analyses that examined health care utilization over the 6-month post-acute period are summarized in Table 2. No significant differences by race or gender were found for IRF admission, SNF admission, or other types of hospitalization. In addition, among those who were admitted to rehabilitation facilities, no race or gender differences were found on the number of days spent in IRF or SNF from the linear regression analyses.
Table 2.
Differences by Race and Gender in Healthcare Utilization over the Six Month Post-Acute Stroke Period (N = 279)
| Utilization Measure | Overall Utilization Rate (N, %) |
Adjusted Odds Ratio for Race (African American vs. White) |
95% confidence interval |
Adjusted Odds Ratio for Gender (Women vs. Men) |
95% confidence interval |
|---|---|---|---|---|---|
| Inpatient Rehabilitation | 77, 27.6 | 1.543 | 0.844 – 2.821 | 0.909 | 0.476 – 1.735 |
| Hospitalizations other than Rehabilitation | 80, 28.7 | 0.914 | 0.492 – 1.700 | 1.379 | 0.718 – 2.650 |
| Emergency Room Visits | 112, 40.1 | 1.074 | 0.605 – 1.907 | 2.373 | 1.285 – 4.382 |
| Skilled Nursing Facility Admission | 55, 19.7 | 0.631 | 0.298 – 1.337 | 1.713 | 0.794 – 3.695 |
| Home Health Agency Visits | 96, 34.4 | 1.504 | 0.835 – 2.709 | 1.918 | 1.023 – 3.597 |
| Physical Therapy | 159, 57.0 | 1.064 | 0.603 – 1.875 | 1.789 | 0.987 – 3.243 |
| Occupational Therapy | 127, 45.5 | 1.356 | 0.779 – 2.358 | 1.531 | 0.854 – 2.744 |
| Speech Therapy | 94, 33.7 | 1.296 | 0.731 – 2.298 | 1.127 | 0.613– 2.070 |
Note: All odds ratios adjusted for the 6-month pre-stroke measure of the same variable, age at time of stroke, residence in or outside the stroke belt, income, whether the person lived with an available caregiver, Charlson comorbidity index, and Medicaid dual-eligibility status.
Women were more likely than men to have an ER claim (adjusted OR = 2.373, p = .006) and to receive HHA care during the 6-month post-acute period (adjusted OR = 1.918, p = .042). Among the 112 participants with at least one ER visit, the linear regression models revealed no differences by race or gender in the total number of ER visits. For HHA care, African Americans had more HHA visits than Whites (adjusted means = 7.4 and 3.8, respectively, p = .003) among the 96 patients who received some HHA care. There were no significant differences in the rates of receipt or number of hours of PT, OT, or SLP by race, but there was a trend that approached statistical significance for women to be more likely to receive physical therapy than men (adjusted OR = 1.789, p = .055).
Supplemental analyses of 248 patients with NIHSS severity scores at discharge found that women (M = 2.63) had worse scores than men (M = 1.88 p = .048). When NIHSS score was added as an additional covariate to the models summarized in Table 2, both of the significant effects for gender remained (ps < .05; see Table S2).
Effects of Covariates
Many of the covariates (age, stroke belt residence, income, co-residing caregiver availability, Charlson comorbidity index, dual eligibility status) did not have significant unique effects on most healthcare utilization measures. However, after adjusting for the other covariates, a higher Charlson comorbidity score was associated with longer acute stroke period length of stay (b = 0.355, p = .004), more primary care outpatient physician visits (b = 0.050, p = .008), an increased likelihood of receiving physical therapy (adjusted OR=1.148, p=0.049), and an increased likelihood of SNF admission (adjusted OR=1.162, p=0.047). Older patients were more likely than younger patients to be admitted to a SNF (adjusted OR = 1.084, p = .002) and were more likely to be hospitalized in the 6-month post-acute period for reasons other than rehabilitation (adjusted OR = 1.051, p=0.029). Medicaid dual eligibility was associated with a longer acute period length of stay (b = 1.342, p = 0.049), a greater likelihood of HHA visits (adjusted OR = 2.116, p = 0.040), and with more claims for primary care outpatient physician visits (b = 0.255, p = .016). In addition, living with an available caregiver was associated with reduced utilization including a shorter acute stroke period length of stay (b= −1.123, p=0.0496), fewer primary care visits (b = −0.178, p = .041) and fewer ER visits after stroke (b = −0.100, p = 0.042).
Discussion
The present analyses of US Medicare claims data indicated a wide variety of post-acute care patterns after ischemic stroke. Although poorer outcomes after stroke have been reported for African Americans1–4 and for women,3,5–6 these effects do not appear to be due to an underutilization of healthcare after stroke for patients from these two groups. Our covariate-adjusted analyses did not reveal any measures for which African Americans or women received less care after stroke than Whites or men, respectively. Some previous studies have reported that African Americans were more likely than Whites to receive rehabilitation services after stroke or to have longer stays in rehabilitation facitlities,13,14 but the evidence is mixed,14 and no race differences on post-stroke rehabilitation utilization have been found in earlier US samples of older Medicare beneficiaries15 or predominantly-male military veterans.16 Taken together, our findings are consistent with the bulk of the existing evidence and suggest that African Americans in the US do not consistently receive less post-acute care after stroke than Whites.
Significant differences were found between women and men in our analyses on multiple post-acute healthcare utilization measures. After controlling for many covariates that might also affect healthcare utilization (e.g., age, income, comorbidity, Medicaid dual eligibility, caregiver availability, initial stroke severity), women received more home-based care and ER care in the 6-month post-acute period than men. Several widely-studied demographic variables (e.g., age, comorbidity, dual eligibility status) were also associated, as expected, with higher post-acute care.
One variable that is less commonly studied in stroke research is caregiver availability, and our findings revealed that living with a co-residing caregiver was associated with a shorter acute period length of stay, fewer ER visits, and fewer primary care physician visits after controlling for covariates. Having an available caregiver might facilitate post-acute care options, such as early supported discharge,17 and this may result in shorter acute hospitalization lengths of stay. The additional caregiver availability findings are consistent with broader health services research on the potential for informal, unpaid care to reduce the needs for some more formal healthcare services.18
Limitations of our findings include a reliance on Medicare claims to assess health care utilization after the acute hospitalization. Claims are submitted for reimbursement purposes and not for documenting the type of care actually provided.19 For some patients, care may have been provided but reimbursement claims were not submitted. In addition, all patients in our analyses were 65 or more years of age and traditional Medicare beneficiaries. Race disparities may be more likely for younger stroke survivors, or for those with non-traditional managed care Medicare coverage, where differences in insurance coverage might have more impact. Additional research is necessary to examine possible care disparities among the populations that were not included in the present analyses.
Strengths of our analyses include the national, population-based sample, use of a standardized claims database, and statistical adjustment for utilization levels before the ischemic stroke hospitalization. All strokes were adjudicated as ischemic stroke events by an expert review panel, and previous analyses have found considerable agreement between those adjudication decisions and the diagnostic codes in the Medicare claims files.20
Future work should incorporate long-term analyses of care utilization that are linked to comprehensive assessments of functional outcomes. A subset of the REGARDS stroke survivors have been enrolled in a long-term observational study of stroke outcomes,3,21 and additional analyses of these stroke survivors should be informative for examining links between stroke severity, care utilization, and psychosocial influences on long-term functional outcomes.
Acknowledgments
Funding
This research project is supported by a cooperative agreement U01 NS041588 from the National Institute of Neurological Disorders and Stroke (NINDS), National Institutes of Health (NIH), Department of Health and Human Service. Additional funding was provided by investigator-initiated grants R01 NS045789 and R01 NS075047 from NINDS. The content is solely the responsibility of the authors and does not necessarily represent the official views of NINDS or NIH.
The authors thank the other investigators, the staff, and the participants of the REGARDS study for their valuable contributions. A full list of participating REGARDS investigators and institutions can be found at http://www.regardsstudy.org.
Footnotes
- Study concept and design: DLR, BK, WEH.
- Data acquisition: JDR, DLR, SJ.
- Data analysis and interpretation: DLR, OCS, JH, MK, JPB, WEH.
- Drafting of manuscript: DLR, OCS, JH, WEH.
- Critical revision of the manuscript: All authors.
References
- 1.Bhandari VK, Kushel M, Price L, Schillinger D. Racial disparities in outcomes of inpatient stroke rehabilitation. Arch Phys Med Rehabil. 2005;86:2081–2086. doi: 10.1016/j.apmr.2005.05.008. [DOI] [PubMed] [Google Scholar]
- 2.Burke JF, Freedman VA, Lisabeth LD, Brown DL, Haggins A, Skolarus LE. Racial differences in disability after stroke. Neurology. 2014;83:390–397. doi: 10.1212/WNL.0000000000000640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Roth DL, Haley WE, Clay OJ, et al. Race and gender differences in one-year stroke outcomes for community-dwelling stroke survivors with family caregivers. Stroke. 2011;42:626–631. doi: 10.1161/STROKEAHA.110.595322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Stansbury JP, Jia H, Williams LS, Vogel WB, Duncan PW. Ethnic disparities in stroke: epidemiology, acute care, and postacute outcomes. Stroke. 2005;36:374–386. doi: 10.1161/01.STR.0000153065.39325.fd. 2005. [DOI] [PubMed] [Google Scholar]
- 5.Fukuda M, Kanda T, Kamide N, Akutsu T, Sakai F. Gender differences in long-term functional outcome after first-ever ischemic stroke. Intern Med. 2009;48:967–973. doi: 10.2169/internalmedicine.48.1757. [DOI] [PubMed] [Google Scholar]
- 6.Petrea RE, Beiser AS, Seshadri S, Kelly-Hayes M, Kase CS, Wolf PA. Gender differences in stroke incidence and poststroke disability in the Framingham Heart Study. Stroke. 2009;40:1032–1037. doi: 10.1161/STROKEAHA.108.542894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ovbiagele B, Goldstein LB, Higashida RT, et al. Forecasting the future of stroke in the United States: A policy statement from the American Heart Association and American Stroke Association. Stroke. 2013;44:2361–2375. doi: 10.1161/STR.0b013e31829734f2. [DOI] [PubMed] [Google Scholar]
- 8.Howard VJ, Cushman M, Pulley L, et al. The Reasons for Geographic And Racial Differences in Stroke study: Objectives and design. Neuroepidemiology. 2005;25:135–143. doi: 10.1159/000086678. [DOI] [PubMed] [Google Scholar]
- 9.O’Neal WT, Quershi WT, Judd SE, et al. Heart rate and ischemic stroke: The REasons for Geographic and Racial Differences in Stroke (REGARDS) study. Int J Stroke. 2015;10:1229–1235. doi: 10.1111/ijs.12620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Williams LS, Yilmaz EY, Lopez-Yunez AM. Retrospective assessment of initial stroke severity with the NIH Stroke Scale. Stroke. 2000;31:858–862. doi: 10.1161/01.str.31.4.858. [DOI] [PubMed] [Google Scholar]
- 11.SEER-Medicare: Calculation of Comorbidity Weights [Internet] Bethesda (MD): National Cancer Institute; [[publication date unknown] [updated 2015 May 2; cited 2015 Oct 9]]. Available from: http://healthcaredelivery.cancer.gov/seermedicare/program/comorbidity.html. [Google Scholar]
- 12.Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities in ICD-9-CM and in ICD-10 administrative data. Med Care. 2005;43:1130–1139. doi: 10.1097/01.mlr.0000182534.19832.83. [DOI] [PubMed] [Google Scholar]
- 13.Gregory PC, Han E, Morozova O, Kuhlemeier KV. Do racial disparities exist in access to inpatient stroke rehabilitation in the State of Maryland? Am J Phys Med Rehabil. 2006;85:814–819. doi: 10.1097/01.phm.0000237870.07136.24. [DOI] [PubMed] [Google Scholar]
- 14.Ellis C, Breland HL, Egede LE. Racial/ethnic differences in utilization of post-stroke rehabilitation services: A systematic review. Ethn Dis. 2008;18:365–372. [PubMed] [Google Scholar]
- 15.Horner RD, Hoenig H, Sloane R, Rubenstein LV, Kahn KL. Racial differences in the utilization of inpatient rehabilitation services among elderly stroke patients. Stroke. 1997;28:19–25. doi: 10.1161/01.str.28.1.19. [DOI] [PubMed] [Google Scholar]
- 16.Horner RD, Swanson JW, Bosworth HB, Matchar DB. Effects of race and poverty on the process and outcome of inpatient rehabilitation services among stroke patients. Stroke. 2003;34:1027–1031. doi: 10.1161/01.STR.0000060028.60365.5D. [DOI] [PubMed] [Google Scholar]
- 17.Mas MA, Inzitari M. A critical review of Early Supported Discharge for stroke patients: from evidence to implementation into practice. Int J Stroke. 2015;10:7–12. doi: 10.1111/j.1747-4949.2012.00950.x. [DOI] [PubMed] [Google Scholar]
- 18.Jacobs JC, Lilly MB, Ng C, Coyte PC. The fiscal impact of informal caregiving to home care recipients in Canada: How the intensity of care influences costs and benefits to government. Soc Sci Med. 2013;81:102–109. doi: 10.1016/j.socscimed.2012.12.015. [DOI] [PubMed] [Google Scholar]
- 19.Lichtman JH, Leifheit-Limson EC, Goldstein LB. Centers for Medicare and Medicaid Services Medicare data and stroke research: Goldmine or landmine? Stroke. 2015;46:598–604. doi: 10.1161/STROKEAHA.114.003255. [DOI] [PubMed] [Google Scholar]
- 20.Kumamaru H, Judd SE, Curtis JR, et al. Validity of claims-based stroke algorithms in contemporary Medicare data: Reasons for Geographic And Racial Differences in Stroke (REGARDS) study linked with Medicare claims. Circ Cardiovasc Qual Outcomes. 2014;7:611–619. doi: 10.1161/CIRCOUTCOMES.113.000743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Haley WE, Roth DL, Hovater M, Clay OJ. Long-term impact of stroke on family caregiver well-being: A population-based case-control study. Neurology. 2015;84:1323–1329. doi: 10.1212/WNL.0000000000001418. [DOI] [PMC free article] [PubMed] [Google Scholar]