Abstract
Twelve male patients with non-union of fracture neck femur of 6-12 months duration were managed by open reduction and internal fixation and tensor fascia lata or gluteus medius muscle pedicle bone grafting through the anterior route. Internal fixation was done with Knowles pins and Asinis screws or combination of both. Union could be achieved in 11 out of the 12 cases. Functional recovery of hip was good in 9, fair in 2 and poor in one.
KEY WORDS: Bone transplantation, Femur neck, Fractures, ununited, Fracture fixation, Tensor fascia lata
Introduction
Non-union is a familiar complication of intracapsular fracture of the neck of the femur. The work of Trueta and Harrison [1] indicated that in 85 per cent of displaced femoral neck fractures there is total or subtotal ischaemia of the femoral head. Various techniques have been proposed to restore the blood supply to the femoral head in order to achieve union and prevent avascular necrosis of femoral head. Frankel and Derian transplanted, in dogs, autogenous muscle pedicle grafts of either gluteus medius or the vastus lateralis into femoral heads made avascular experimentally [2]. They reported that both grafts restored circulation to the femoral head. Judet, and Doyen and Judet developed a technique for humans in which an autogenous muscle pedicle graft composed of the guadratus femoris muscle and the bone at its insertion were used [3]. Hewson also suggested the use of a pedicle graft from gluteus maximus applied to femoral neck fracture to increase both vascularity and fracture stability [4]. In the present study, muscle pedicle bone graft (MPBG) utilizing tensor fascia lata (TFL) or anterior 4 cm of gluteus medius (where TFL was found to be inadequate) was used to obtain union.
Material and Methods
During the period Oct 92 to Aug 94, 12 patients underwent TFL or gluteus medius MPBG operation for intracapsular fractures of the neck femur. Criteria used for case selection in the present study were: Ability to walk prior to fracture; ready to co-operate in post-operative physiotherapy and rehabilitation programme; and no serious intercurrent disease. All patients were males aged between 18 and 47 years. There were 5 patients between 18 to 25 years, 3 between 25 to 30 years and remaining 4 patients were between 38 to 48 years. Eight patients had fracture on right side and 4 on the left. Injury had been sustained during road traffic accidents in 6 cases, falls from bicycle in 2 cases and falls on uneven ground in the remaining 4.
Non-union was diagnosed both clinically and radiologically in all the patients. Before surgery none of the patients were ambulatory without support. Non-union had been present for varying periods ranging from 6 to 12 months before surgery was undertaken. Duration of non-union was 6 to 8 months in five patients, 8 to 10 months in another five patients and in 2 patients it was 10 to 12 months.
Seven out of 12 patients had had local treatment in the form of local massage, 2 had been managed with skeletal traction and 3 had undergone open reduction and internal fixation. Out of 12 cases 8 had basicervical fractures and 4 had transcervical fractures.
Operative procedure
Skin incision was made along the anterior border of TFL muscle, curving it posteriorly across the insertion of this muscle into the iliotibial band in the subtrochanteric region (usually at a point 8 to 10 cm below the base of the trochanter). The fracture site was exposed by Watson-Jones approach i.e., locate interval between gluteus medius and TFL and incise the anterior capsule of the hip joint longitudinally. The fracture was opened by laterally rotating the leg and fracture site freshened up. Fracture was reduced and fixed under direct vision utilizing 2 or 3 Asinis’ screws or Knowles pins or combination of both. After fixing the fracture, attention was diverted to harvesting of graft. A 4 cm × 1 cm × 0.5 cm, unicortical graft based on TFL was harvested from the iliac crest and mobilized distally to insertion of TFL. An appropriate sized slot was made on the anterior surface of the femur neck and greater trochanter extending onto the head. The graft was seated in this slot after bevelling its proximal end which was impacted into the head and fixed in the trochanteric region with a cortical screw. The edges of the TFL or gluteus medius were sutured to the capsule. The wound was irrigated and closed over a suction drain. Where the TFL was found to be inadequate, anterior 4 cm of gluteus medius was used as described for TFL. Post-operative active and passive movements of the hip were allowed as soon as pain subsided. Partial weight bearing was commenced 8 to 12 weeks after operation and full weight bearing was possible after about 4 months depending upon progression of radiological union.
Osseous union was presumed when patient could walk without pain on full weight bearing and the fracture gap had disappeared radiologically. The results were assessed clinically and radiologically and grouped into 3 categories: Good (fracture united, no deformity, full range of painless hip movements, able to sit cross-legged and to squat, able to walk any distance without a walking-aid), Fair (fracture united with minimal shortening, movements more than 75 per cent of normal of hip joint, no pain on weight bearing, able to squat but unable to sit cross-legged, able to walk without a walking-aid), or Poor (fracture not united, shortening more than 1.5 cm, less than 50 per cent of normal movements at hip joint, movements painful at extremes, able to walk with walking-aids, not able to squat or sit cross-legged).
Results
Union of fracture could be achieved in all cases except one where deep infection marred the results. On final assessment function of the hip was good in 9 patients (75%), fair in 2 cases (17%) and poor in 1 case (8%) as assessed by criteria outlined above. Infection was the main complication and was encountered in 3 patients. Superficial infection was found in 2 cases and was managed conservatively. In the 3rd patient treatment of infection required removal of fixation devices and open drainage. On an average it took about 4 to 6 months before good radiological union was evident. All patients were reviewed periodically in the out-patient department. Follow-up ranged between 6 months and 24 months with an average of 18 months.
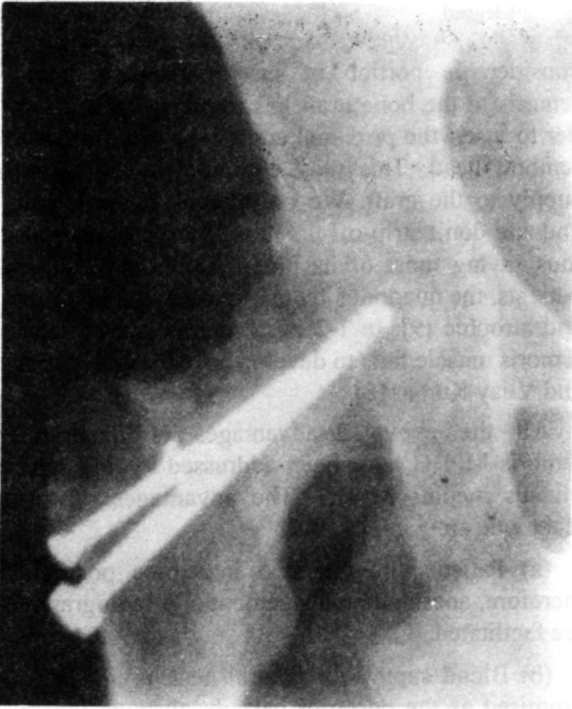
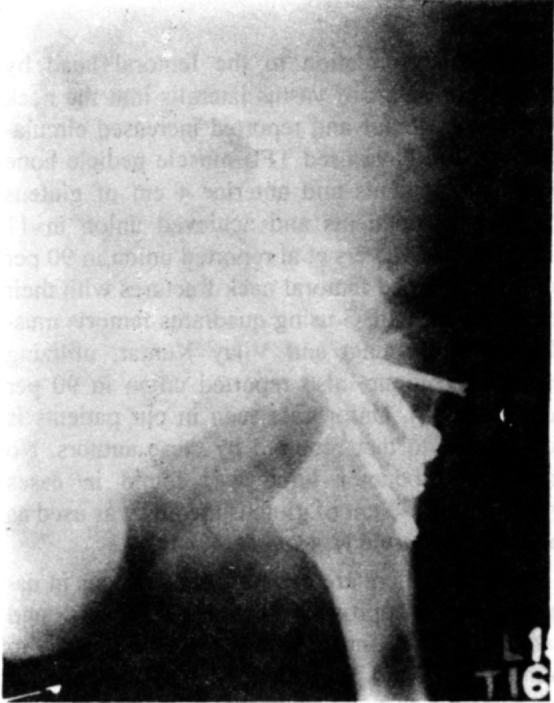
Figure 1 shows a case of non-union of fracture neck femur. Fig 2 demonstrates union obtained after internal fixation and TFL muscle pedicle bone grafting. Fig 3 and 4 show another case of fracture of neck of the femur before surgery and after 9 months follow-up. Fig 5 and 6 show ability of the patients to squat 6 months after surgery.
Fig. 1.

Radiograph showing non-union of fracture neck femur in one of the patients.
Fig. 2.
Radiograph of same patient as Fig 1. Shows union obtained 6 months after internal fixation and tensor
Fig. 3.

Radiograph of another patient. Shows ununited fracture neck femur.
Fig. 4.
Radiograph of same patient as Fig 3. Shows union obtained 9 months after internal fixation and tensor fascia lata muscle pedicle bone grafting.
Fig. 5.
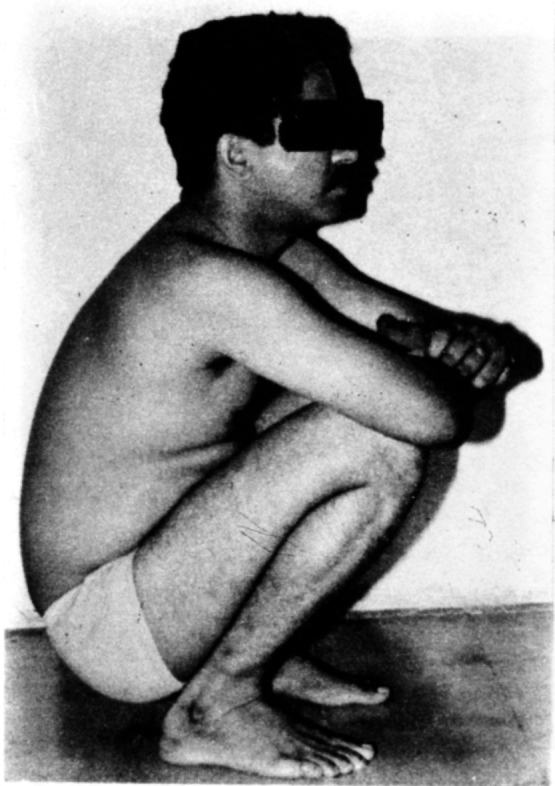
Photograph showing ability of a patient to squat 6 months after surgery.
Fig. 6.
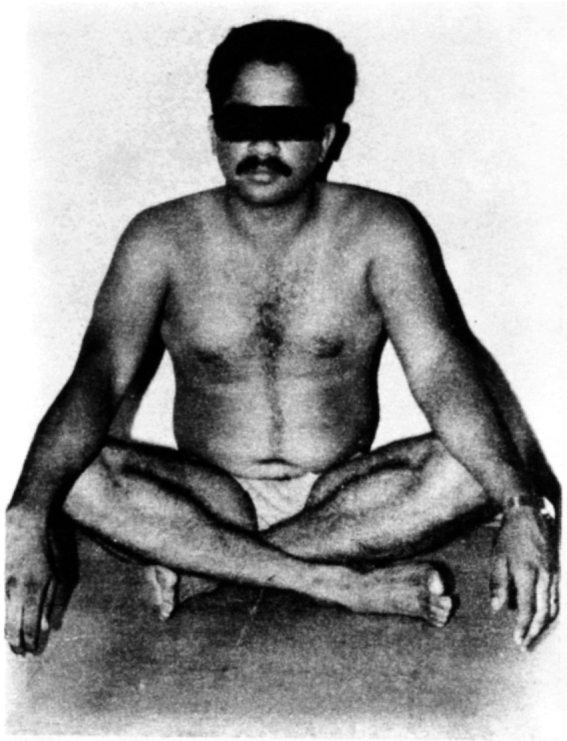
Same patient as Fig 5. Shows ability to sit cross-legged.
Discussion
The ideal bone graft is a vascularized autogenous bone graft. The next best is the MPBG which provides a living graft for rapid incorporation as well as provides collateral circulation to the avascular bone. Phemister reported use of a free fibular graft for treatment of necrotic head of the femur in non-union of fracture neck femur [5]. The fracture united promptly but weight bearing had to be delayed for several months. Since then various techniques have been proposed to restore blood supply to the proximal fragment of the fractures of neck femur. Stuck and Hinchey attempted to improve circulation to the femoral head by transplanting part of vastus lateralis into the neck of involved femur and reported increased circulation [6]. We have used TFL muscle pedicle bone graft in 9 patients and anterior 4 cm of gluteus medius in 3 patients and achieved union in 11 (92%) cases. Meyers et al reported union in 90 per cent of displaced femoral neck fractures with their technique of MPBG using quadratus femoris muscle [7]. Prem Lata and Vijay Kumar, utilizing Meyers technique, also reported union in 90 per cent cases [8]. Union rate seen in our patients is comparable to that reported by these authors. No significant abductor lurch was found in cases where anterior 4 cm of gluteus medius was used as most of the muscle was spared.
However, there are certain disadvantages in using posterior approach utilized by Meyers, and Lata and Vijay Kumar. Firstly, the blood supply to the femoral head runs along the posterosuperior aspect of the femoral neck, therefore, any grafting procedure on this aspect may further compromise the already precarious blood supply. Secondly, a considerable portion of insertion of quadratus femoris to the bone graft has to be stripped in order to insert the proximal end of the graft into the femoral head. This may compromise the blood supply to the graft. We only bevel the proximal end and don't strip-off the muscle from bone graft thus saving most of its blood supply. In elderly patients, the quadratus femoris muscle may be thin and atrophic [9]. In 1-2 per cent cases, quadratus femoris muscle fails to develop as reported by Lata and Vijay Kumar [8].
All the above disadvantages of quadratus femoris MPBG have been addressed by TFL and gluteus medius MPBG. The advantages of this technique are :
-
(a)
Patients are operated in supine position, therefore, anesthetic management and radiography are facilitated.
-
(b)
Blood supply to femoral neck is not compromised as the posterior capsule, through which the main blood supply runs, is left intact.
-
(c)
The trochanteric region is not weakened as happens with quadratus femoris MPBG.
To achieve best results essential requirements are an anatomically accurate reduction, impaction of fragments and stable fixation. While transferring the MPBG to its recipient site, any torsion or tension on muscle pedicle should be avoided.
Thus to conclude, a TFL or gluteus medius MPBG appears to be an useful technique in the management of non-union of fractures of the femoral neck.
REFERENCES
- 1.Tructa J. Harrison MHM. The normal vascular anatomy of the femoral head in adult man. J Bone Joint Surg. 1953;35B:442–461. doi: 10.1302/0301-620X.35B3.442. [DOI] [PubMed] [Google Scholar]
- 2.Frankel CJ, Derian PS. The introduction subcapital femoral circulation by means of an autogenous muscle pedicle graft. Surg Gynecol Obstet. 1962;115:473–477. [PubMed] [Google Scholar]
- 3.Judet R. Treatment des fractures du col du femur par greffe pediculee. Acta Orthop Scandinavice. 1962;32:421–427. doi: 10.3109/17453676208989601. and Doyen G and R Judet Donnes experimentales sur le pediculee dans les fractures due col du femur epaules fractures du col du femur, Paris, Massonet Cie 1963 Quoted by Meyers MH (6) [DOI] [PubMed] [Google Scholar]
- 4.Hewson JS. Treatment of intracapsular fractures of the hip with primary bone graft from greater trochanter. Clin Orthop. 1971:76–100. doi: 10.1097/00003086-197105000-00015. [DOI] [PubMed] [Google Scholar]
- 5.Phemister DB. Treatment of the necrotic head of femur in adults. J Bone Joint Surg. 1949;31a:55–66. [PubMed] [Google Scholar]
- 6.Stuck WG, Hinchey JJ. Experimentally increased blood supply to head and neck of femur. Surg Gynecol Obstet. 1944;78:160–163. [Google Scholar]
- 7.Meyers MH, Harvey JP, Jr, Moore TM. Treatment of displaced subcapital transcervical fracture of the femoral neck by muscle pedicle bone graft and internal fixation. J Bone Joint Surg. 1973;55A:257–274. [PubMed] [Google Scholar]
- 8.Lata P, Kumar BG Vijay. Results of muscle pedicle bone graft and internal fixation in femoral neck fractures. Indian Journal of Orthopedics. 1993;27:166–170. [Google Scholar]
- 9.Baksi DP. Treatment of post-traumatic avascular necrosis of femoral head by multiple drilling and muscle pedicle bone graft. J Bone Joint Surg. 1983;65b:268–273. doi: 10.1302/0301-620X.65B3.6341373. [DOI] [PubMed] [Google Scholar]


