Figure 2.
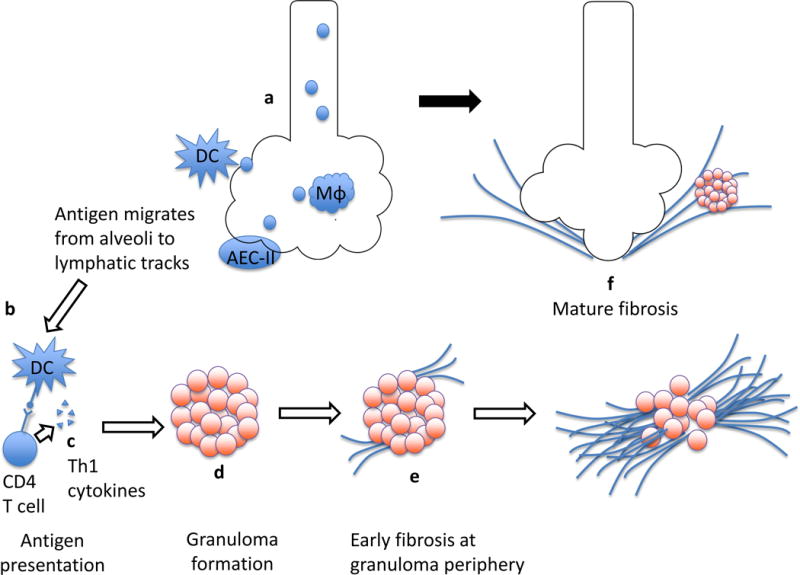
Granulomatous inflammation transitions to fibrosis. The pathophysiology of sarcoidosis begins with exposure to putative inhaled antigen(s) that in the appropriate genetic and epigenetic context initiate an immune cascade via activation of interstitial dendritic cells (DC), alveolar macrophages (Mφ), and type 2 alveolar epithelial cells (AEC-II) (a). Antigen is presented by cells such as DC and recognized by CD4+ T cells (b). The engagement of CD4+ cells leads to their activation and proliferation, and release of an array of pro-inflammatory cytokines (c). Antigen features, Th1 polarization of CD4+ lymphocytes, and the cytokine milieu all likely contribute to the recruitment and organization of macrophages into granulomas within lymphatic tracks (d). In some cases, fibrosis begins at the periphery of sarcoid granulomas (e), which serves to contain if not break up active granulomas. As it extends over time, this deposition of collagen results in mature fibrosis which obliterates parenchymal tissue, resulting in “end-stage” sarcoidosis (f).
