Abstract
The study assessed 12-month chronic pain (CP)-related health care utilization and costs among chronic noncancer pain (CNCP) patients who initiated various long-term opioid treatments. Treatments included monotherapy with long-acting opioids (mono-LAOs), mono-therapy with short-acting opioids (mono-SAOs), both LAOs and SAOs (combination), and opioid therapy initiated with SAO or LAO and switched to the other class (switch). Using MarketScan® claims databases (2006–2012), we identified CNCP patients with ≥90 days opioid supply after pain diagnosis and continuous enrollment 12 months before pain diagnosis (baseline period) and 12 months after opioid start (post-index period). Outcomes included CP-related health care utilization and costs. Among CNCP patients (n=21,203), the cohort distribution was 74% mono-SAOs, 22% combination, 2% mono-LAOs, and 2% switch. During follow-up, the average daily morphine equivalent dose was highest in mono-LAO patients (96.4 mg) compared with combination patients (89.8 mg), switch patients (64.3 mg), and mono-SAO patients (36.2 mg). After adjusting for baseline differences, the mono-LAO cohort had lower total CP-related costs ($4,933) compared with the mono-SAO ($8,604), switch ($10,470), and combination ($15,190) cohorts (all: P<0.05). Mono-LAO patients had greater CP-related prescription costs but lower medical costs than the other cohorts during the follow-up period, including lower CP-related hospitalizations (1% vs 11%–20%), emergency department visits (4% vs 11%–18%), and diagnostic radiology use (21% vs 54%–61%) (all: P<0.001). Use of pain-related medications and other treatment modalities was also significantly lower in the mono-LAO cohort relative to the other cohorts. CNCP patients using long-term monotherapy with LAOs had the lowest CP-related total health care costs in the 12 months after opioid initiation compared with mono-SAO, switch, or combination patients despite higher opioid daily doses and higher prescription costs. Future research accounting for severity and duration of pain would aid in determining the optimal long-term opioid regimen for CNCP patients.
Keywords: chronic pain, long-acting opioids, short-acting opioids, health care claims, database study
Introduction
Chronic pain (CP), described as pain beyond the time of expected healing (e.g., 3–6 months),1 is common and experienced by 25.5 million adults in the USA.2 The associated costs are substantial, with annual direct and indirect costs of CP ranging from $560 to $635 billion (2010 USD).3 CP is managed with a number of pharmacologic and nonpharmacologic treatments.4 Pharmacologic options include nonopioid (e.g., acetaminophen, anticonvulsants, cyclo-oxygenase-2 inhibitors, nonsteroidal anti-inflammatory drugs [NSAIDs], skeletal muscle relaxants, topical agents) and opioid medications.4 Despite the variety of nonopioid pain medications, some of which can be used alone or in combination, a substantial number of patients do not attain adequate relief.5,6 Studies estimate that pain relief in at least 50% of patients with CP is inadequate with current pharmacologic treatments.5,6
The primary objective in the management of CP is to relieve pain and allow patients to maintain functionality and quality of life. Current treatment guidelines recommend use of opioids in select CP patients, including those with inadequate pain relief from nonopioid treatments.7,8 Short-acting opioids (SAOs) are used when patients experience episodic or breakthrough pain, and long-acting opioids (LAOs) are used alone or in combination with an SAO when patients require around-the-clock sustained analgesia or alternative treatment options after pain relief is inadequate.9 However, whereas opioids are an important tool in the management of CP,7,8,10–17 experts recognize a lack of published clinical evidence describing the long-term (≥1 year) outcomes of chronic opioid therapy and the role of SAOs and LAOs.7,8,11,18 Unfortunately, data are lacking for the use of nonopioid classes of analgesics as well.
The current study was conducted to observe opioid treatment patterns in patients with chronic noncancer pain (CNCP) receiving long-term opioid therapy and to describe the associated CNCP-related health care utilization and costs.
Materials and methods
Data source
Integrated medical and prescription claims data (January 2006–December 2012) were obtained from the Truven Health MarketScan Commercial Claims and Encounters Database (Commercial) and Medicare Supplemental and Coordination of Benefits Database (Medicare Supplemental). Both databases contain inpatient and outpatient medical and prescription claims, with information on diagnoses, procedures, prescription fills, dates of service, and person-level enrollment information. The Commercial database collects information annually from more than 40 million individuals, including employees, spouses, and dependents covered by employer-sponsored private health insurance. Health care for these individuals is provided under a variety of fee-for-service, fully capitated, and partially capitated health plans, including preferred and exclusive provider organizations, point-of-service plans, and health maintenance organizations. The Medicare Supplemental Database collects information annually from ~4.3 million Medicare-eligible persons who maintain supplemental insurance plans offered by former employers. The Medicare-covered portion of payment is captured as the coordination of benefits amount. Enrollees were followed longitudinally and as they move from the Commercial to Medicare Supplemental database through the use of a unique blinded identifier. All Truven Health MarketScan data are Health Insurance Portability and Accountability Act of 1996 compliant. As no patient identifiers are available and given the anonymous nature of the data, no patient consent or institutional review board approval was required for the conduct of this study.
Study design
This study was a retrospective cohort analysis of data from CNCP patients who have used opioid for a long term. Patients with CNCP were defined as those having ≥3 nondiagnostic medical claims 1–12 months apart with International Classification of Diseases, Ninth Revision, Clinical Modification diagnosis codes of the same pain type (back, neck, osteoarthritis, fibromyalgia, or neuropathic pain) in any position, between January 1, 2007, and December 31, 2011.
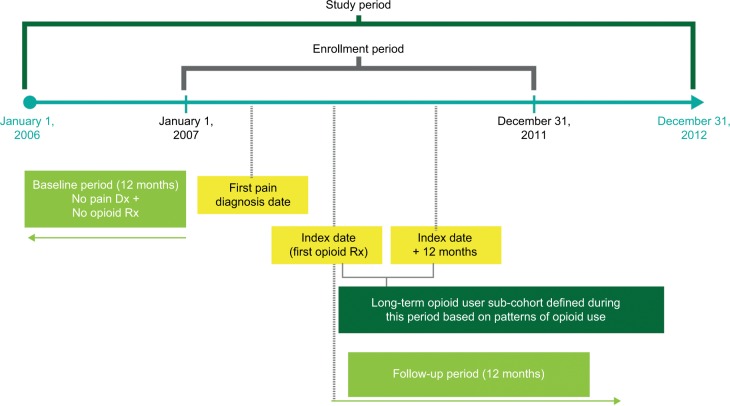
The index date was defined as the date of the first opioid prescription fill (Figure 1) after CNCP diagnosis, and long-term opioid therapy was defined as a 90-day opioid supply after CNCP diagnosis. A 12-month baseline period before the date of the first CP diagnosis was used to assess clinical characteristics of the study sample, and a 12-month follow-up period, beginning on the index date, was used to evaluate all study outcomes.
Figure 1.
Study design.
Notes: Patients were required to be enrolled for 12 months before the index date and for 12 months after the index date. Cohorts were defined by pattern of opioid use during the 12-month follow-up period.
Abbreviations: Dx, diagnosis; Rx, prescription.
Study cohorts and study criteria
Long-term opioid users were stratified into four cohorts based on pattern of opioid use in the 12-month follow-up period. A mono-LAO cohort and a mono-SAO cohort consisted of patients who filled prescriptions solely for LAOs or SAOs, respectively. A combination cohort consisted of patients who filled prescriptions for both LAOs and SAOs, with LAOs being filled regularly and SAOs filled intermittently. A switch cohort consisted of patients who first filled prescriptions for one opioid class and then began filling prescriptions for the alternative class without another prescription fill for the initial class.
Patients were required to be ≥18 years of age at the first pain diagnosis date, have no pain diagnosis and no prescription opioid claim in the 12 months before the first pain diagnosis date, have no diagnosis of a malignancy anytime in the 12 months before or anytime after the first pain diagnosis date, and have continuous medical and pharmacy coverage during the 12 months before the first pain diagnosis date and the 12 months after the index date. Patients who did not use prescription opioids or who used opioids for short term (<90 days supply) were excluded.
Baseline and opioid treatment measures
Baseline demographics included age, sex, health plan type, primary payer, and geographic region of residence on the date of the first CNCP diagnosis, and clinical characteristics included comorbidities and prescription medication history in the 12 months before CNCP diagnosis. Number of days from CNCP diagnosis to opioid initiation and total number of days of opioid supply in the 12 months after treatment initiation were captured. Average daily opioid dose in milligrams was converted to the daily morphine equivalent dose (MED) for each patient to standardize dosages across the many opioids and formulations used.
Outcomes
Outcomes evaluated during the 12-month follow-up period included CNCP-related health care costs, health care utilization by type of service, prescription medications, and other pain-related treatment modalities. CNCP-related costs included all payments received by health care providers, including those paid by the insurer (payer plus coordination of benefits) and the patient (deductible plus copayment plus coinsurance) for medical claims with a primary diagnosis for any of the five CNCP diagnoses or pain-related prescription medications. Total CNCP-related cost and cost components (medical and prescription) were standardized to USD 2012 using the medical component of the consumer price index. CNCP-related medical resource use was categorized by setting of care (e.g., hospitalization, emergency department [ED], office visit, radiology, laboratory/other outpatient). Use of prescription pain treatments in addition to opioids and other treatment modalities (e.g., nerve blocks, physical therapy, epidural injections) was also assessed.19,20
Statistical analysis
Descriptive statistics were used to characterize the study sample during the baseline period. Inferential statistics, including one-way analysis of variance F-tests for continuous measures and chi-square for categorical measures, were used to compare sample characteristics and outcomes across the four study cohorts. Multivariate analyses using generalized linear models with log-link function and gamma distribution were used to assess differences in total CNCP-related health care costs and cost components (medical and prescription) across the opioid user cohorts. All models controlled for demographic and clinical characteristics assessed at baseline: age, sex, region, Charlson Comorbidity Index (CCI), urban or rural residence, health plan type, primary payer, index year, type of CP diagnosis, number of CP diagnoses, baseline comorbid conditions, and baseline use of pain-related prescription medications. Adjusted average costs with 95% CI for total, medical, and prescription utilization are presented.
Results
Patients and baseline characteristics
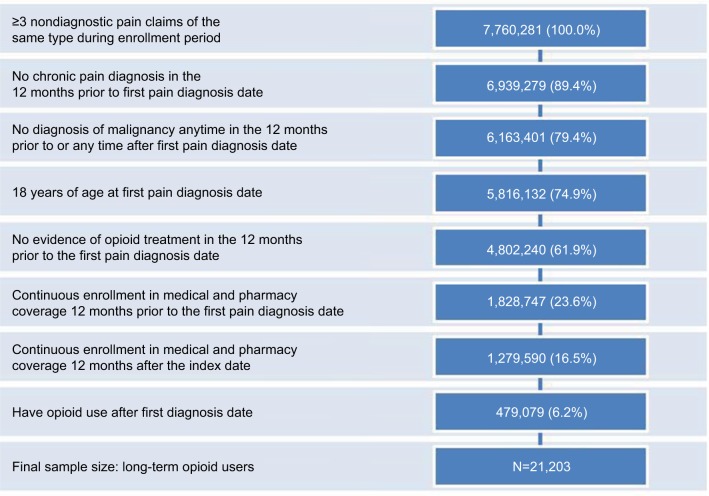
A total of 21,203 patients were included in the final sample: 2% mono-LAO, 74% mono-SAO, 22% combination, and 2% switch (Table 1; Figure 2). Combination users were mainly LAO users filling SAO prescriptions intermittently, and switch users were primarily SAO users who eventually either added or switched to LAO therapy (71%). Overall, opioid users (mono-LAO and mono-SAO) were aged 52.7±14.7 years, 51% were women, and the majority had a CNCP diagnosis of low back pain. The combination cohort was the most likely to have ≥2 CNCP diagnoses (P<0.001). The mono-LAO cohort had the highest average CCI (0.96 vs 0.61–0.81 [P<0.001]), highest rate of diagnosed depression (19% vs 12%–17% [P<0.001]), highest rate of diagnosed drug abuse and/or dependence (14% vs 1%–4% [P<0.001]), and the lowest rate of NSAID/acetaminophen, muscle relaxant, and corticosteroid use before CP diagnosis and opioid initiation (P<0.001 for each).
Table 1.
Baseline comparison among opioid user type cohorts
| Characteristics | Mono-LAO | Mono-SAO | Combination | Switch | P-valuea |
|---|---|---|---|---|---|
| Population, n (%) | 407 (1.9) | 15,707 (74.1) | 4,593 (21.7) | 496 (2.3) | |
| Demographic | |||||
| Age, years, mean (SD) | 53.5 (18.2) | 52.5 (14.5) | 53.0 (14.8) | 55.0 (18.0) | 0.0005 |
| Age group, years, n (%) | |||||
| 18–44 | 127 (31.2) | 4,455 (28.4) | 1,221 (26.6) | 141 (28.4) | <0.0001 |
| 45–64 | 189 (46.4) | 8,662 (55.2) | 2,596 (56.5) | 229 (46.2) | |
| ≥65 | 91 (22.4) | 2,590 (16.5) | 776 (16.9) | 126 (25.4) | |
| Male, n (%) | 184 (45.2) | 7,670 (48.8) | 2,257 (49.1) | 229 (46.2) | 0.2977 |
| Residence type, n (%) | |||||
| Urban | 333 (81.8) | 12,052 (76.7) | 3,661 (79.7) | 404 (81.5) | <0.0001 |
| Rural | 72 (17.7) | 3,454 (22.0) | 865 (18.8) | 88 (17.7) | |
| Unknown | 2 (0.5) | 201 (1.3) | 67 (1.5) | 4 (0.8) | |
| Geographic region, n (%) | |||||
| Northeast | 68 (16.7) | 1,652 (10.5) | 598 (13.0) | 80 (16.1) | <0.0001 |
| North Central | 126 (31.0) | 4,660 (29.7) | 1,413 (30.8) | 151 (30.4) | |
| South | 136 (33.4) | 6,743 (42.9) | 1,653 (36.0) | 162 (32.7) | |
| West | 75 (18.4) | 2,450 (15.6) | 862 (18.8) | 97 (19.6) | |
| Unknown | 2 (0.5) | 202 (1.3) | 67 (1.5) | 6 (1.2) | |
| Payer, n (%) | |||||
| Commercial | 315 (77.4) | 13,204 (84.1) | 3,846 (83.7) | 373 (75.2) | <0.0001 |
| Medicare Supplemental | 92 (22.6) | 2,503 (15.9) | 747 (16.3) | 123 (24.8) | |
| Clinical | |||||
| Index year, n (%) | |||||
| 2007 | 144 (35.4) | 3,743 (23.8) | 1,305 (28.4) | 120 (24.2) | <0.0001 |
| 2008 | 83 (20.4) | 3,157 (20.1) | 946 (20.6) | 94 (19.0) | |
| 2009 | 66 (16.2) | 3,480 (22.2) | 950 (20.7) | 115 (23.2) | |
| 2010 | 70 (17.2) | 3,070 (19.6) | 808 (17.6) | 85 (17.1) | |
| 2011 | 44 (10.8) | 2,257 (14.4) | 584 (12.7) | 82 (16.5) | |
| Type of chronic pain diagnosis – nonmutually exclusive categories, n (%) | |||||
| Low back | 364 (89.4) | 14,044 (89.4) | 4,184 (91.1) | 454 (91.5) | 0.0054 |
| Neck | 143 (35.1) | 7,874 (50.1) | 2,489 (54.2) | 242 (48.8) | <0.0001 |
| Osteoarthritis | 169 (41.5) | 7,162 (45.6) | 2,185 (47.6) | 209 (42.1) | 0.0084 |
| Number of chronic pain diagnoses, n (%) | |||||
| 1 | 296 (72.7) | 10,798 (68.8) | 2,915 (63.5) | 346 (69.8) | <0.0001 |
| 2 | 94 (23.1) | 4,106 (26.1) | 1,320 (28.7) | 121 (24.4) | |
| ≥3 | 17 (4.2) | 803 (5.1) | 358 (7.8) | 29 (5.9) | |
| CCI, mean (SD) | 0.96 (1.5) | 0.61 (1.1) | 0.78 (1.2) | 0.81 (1.2) | <0.0001 |
| Comorbid conditions, n (%) | |||||
| Depression | 77 (18.9) | 1,940 (12.4) | 768 (16.7) | 84 (16.9) | <0.0001 |
| Anxiety | 41 (10.1) | 1,414 (9.0) | 467 (10.2) | 47 (9.5) | 0.1088 |
| Sleep disturbance | 48 (11.8) | 1,435 (9.1) | 471 (10.3) | 49 (9.9) | 0.0459 |
| Hypertension | 156 (38.3) | 6,240 (39.7) | 1,847 (40.2) | 207 (41.7) | 0.6873 |
| Other cardiovascular disease | 79 (19.4) | 2,034 (13.0) | 769 (16.7) | 111 (22.4) | <0.0001 |
| Ischemic heart disease | 43 (10.6) | 1,361 (8.7) | 473 (10.3) | 54 (10.9) | 0.0023 |
| Diabetes | 73 (17.9) | 2,499 (15.9) | 763 (16.6) | 86 (17.3) | 0.4126 |
| Drug abuse/dependence | 58 (14.3) | 196 (1.3) | 145 (3.2) | 21 (4.2) | <0.0001 |
| Alcohol abuse | 8 (2.0) | 339 (2.2) | 121 (2.6) | 13 (2.6) | 0.2528 |
| Alcohol dependence | 7 (1.7) | 314 (2.0) | 115 (2.5) | 14 (2.8) | 0.1189 |
| Concomitant medications, n (%) | |||||
| NSAIDs/acetaminophen | 118 (29.0) | 6,953 (44.3) | 1,692 (36.8) | 203 (40.9) | <0.0001 |
| Muscle relaxants | 85 (20.9) | 5,444 (34.7) | 1,488 (32.4) | 174 (35.1) | <0.0001 |
| Corticosteroids | 58 (14.3) | 3,620 (23.1) | 1,018 (22.2) | 123 (24.8) | 0.0002 |
| Antidepressants | 145 (35.6) | 4,604 (29.3) | 1,532 (33.4) | 167 (33.7) | <0.0001 |
| Anticonvulsants | 106 (26.0) | 2,800 (17.8) | 1,007 (21.9) | 131 (26.4) | <0.0001 |
| Benzodiazepines | 68 (16.7) | 3,024 (19.3) | 951 (20.7) | 101 (20.4) | 0.0693 |
Note:
Overall P-value indicates statistical difference across all cohorts.
Abbreviations: CCI, Charlson Comorbidity Index; LAO, long-acting opioid; NSAID, nonsteroidal anti-inflammatory drug; SAO, short-acting opioid.
Figure 2.
Study attrition.
Twelve-month follow-up
Mono-LAO patients had the longest time to opioid initiation from the date of the first CP diagnosis (265.0±320.2 days), which was more than 100 days longer than in the other cohorts (Table 2). This cohort also had the highest average daily dose of opioids (96.4±84.6 mg), which was 7 mg MED greater than combination cohort, 32 mg MED greater than switch cohort, and 60 mg MED greater than mono-SAO cohort. In addition, the mono-LAO and combination cohorts had the greatest days of opioid supply (285 days each), 30 and 45 days longer than in the switch and mono-SAO cohorts, respectively.
Table 2.
Opioid treatment characteristics during 1-year follow-up
| Opioid treatment characteristic, mean (SD) | Mono-LAO | Mono-SAO | Combination | Switch | P-valuea |
|---|---|---|---|---|---|
| Time from pain diagnosis to opioid initiation, days | 265.0 (320.2) | 154.6 (243.1) | 163.0 (248.5) | 153.0 (239.8) | <0.001 |
| Average daily dose, mg MED | 96.4 (84.6) | 36.2 (27.7) | 89.8 (81.8) | 64.3 (55.4) | <0.001 |
| Total days supply | 285.4 (93.9) | 240.2 (96.1) | 285.1 (97.2) | 255.1 (101.0) | <0.001 |
Note:
Overall P-value indicates statistical difference across all cohorts.
Abbreviations: LAO, long-acting opioid; MED, morphine equivalent dose; SAO, short-acting opioid.
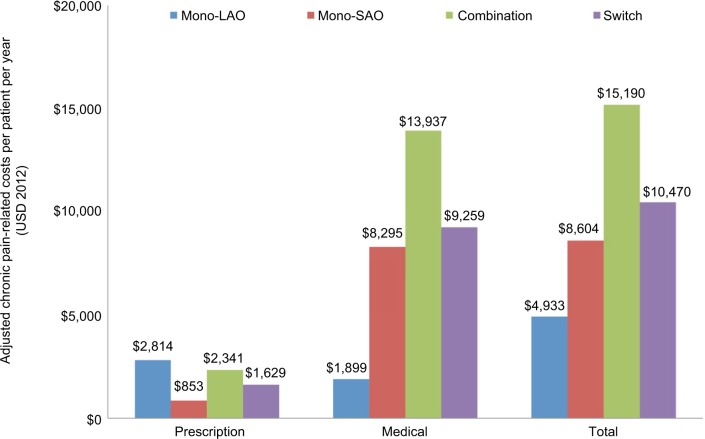
The mono-LAO cohort had the lowest average CNCP-related medical cost ($1,899), leading to the lowest annual adjusted per-patient total CNCP-related health care cost ($4,933), despite the highest average CNCP-related prescription cost ($2,814) (Figure 3). The combination cohort had the second highest average CNCP-related prescription cost ($2,341) and the highest CNCP-related medical cost ($13,937) and thus the highest total CNCP-related health care cost ($15,190).
Figure 3.
The adjusted chronic pain-related costs per patient per year (USD 2012) during follow-up.
Notes: Despite having the highest prescription costs, total costs were lowest in the mono-LAO cohort. Each cost component is estimated from separate regression models and represents a predicted, rather than an observed, value. Therefore, prescription and medical cost components may not add up to the total cost.
Abbreviations: LAO, long-acting opioid; SAO, short-acting opioid; USD, US dollars.
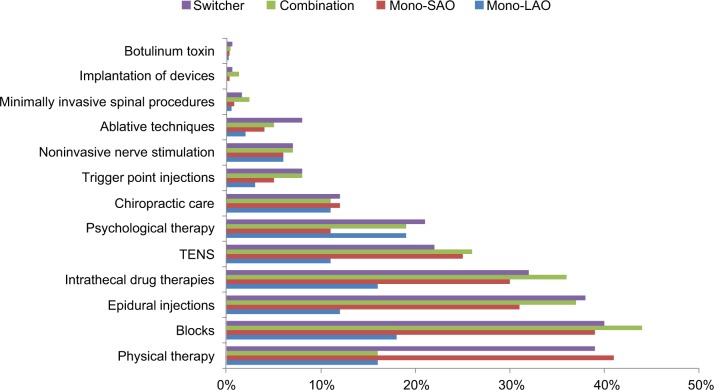
Cost differences reflected the differences in CNCP-related health care resource use. The combination cohort had the greatest proportion of patients using nearly all concomitant pain-related prescription medications, and the mono-LAO cohort had the fewest patients using most of these same treatments, including NSAIDs/acetaminophen, muscle relaxants, and corticosteroids (data not shown). The use of most pain-related nonprescription drug treatment modalities was also significantly lower for the mono-LAO patients compared with the other cohorts (Figure 4). The differences were most pronounced for physical therapy, epidurals, nerve blocks, transcutaneous electrical nerve stimulation (TENS), and intrathecal drug therapies (P<0.001 for all).
Figure 4.
The use of pain-related treatment modalities during the 12-month follow-up, by cohort.
Notes: Statistical significance was P<0.001 for all modalities except acupuncture (P=0.006), chiropractic care (P=NS), and botulinum toxin (P=NS).
Abbreviations: LAO, long-acting opioid; NS, not significant; SAO, short-acting opioid; TENS, transcutaneous electrical nerve stimulation.
Patients receiving mono-LAO treatment had significantly lower CNCP-related health care utilization across all settings of care for both rates of use and number of services in the year post-opioid initiation (Table 3). The lower medical costs appeared to be driven by lower rates of hospitalizations (1.2% vs 11.3%–20.1%) and ED visits (3.7% vs 10.6%–18.4%). Conversely, those receiving combination opioid therapies had the highest rates of health care utilization in all care settings.
Table 3.
Chronic pain-related medical utilization during 1-year follow-up
| CP-related utilization category | Mono-LAO | Mono-SAO | Combination | Switch | P-valuea |
|---|---|---|---|---|---|
| Hospitalization, n (%) | 5 (1.2) | 2,005 (12.8) | 923 (20.1) | 56 (11.3) | <0.001 |
| Number of visits, mean (SD)b | 1.0 (0.0) | 1.1 (0.3) | 1.1 (0.4) | 1.1 (0.3) | 0.020 |
| Average LOS, mean (SD)b | 3.0 (0.7) | 2.9 (2.1) | 3.6 (3.0) | 3.6 (3.6) | <0.001 |
| Emergency department visits, n (%) | 15 (3.7) | 1,667 (10.6) | 843 (18.4) | 72 (14.5) | <0.001 |
| Number of visits, mean (SD)b | 1.2 (0.4) | 1.3 (0.8) | 1.7 (1.4) | 1.3 (1.1) | <0.001 |
| Physician office visits, n (%) | 301 (74.0) | 13,885 (88.4) | 4,127 (89.9) | 435 (87.7) | <0.001 |
| Number of visits, mean (SD)b | 4.3 (3.2) | 5.0 (3.9) | 6.4 (4.7) | 5.8 (4.5) | <0.001 |
| Radiology services, n (%) | 87 (21.4) | 8,471 (53.9) | 2,801 (61.0) | 280 (56.5) | <0.001 |
| Number of services, mean (SD)b | 1.7 (1.3) | 2.3 (1.6) | 2.6 (1.9) | 2.5 (2.2) | <0.001 |
| Laboratory and other OP services, n (%) | 163 (40.0) | 9,961 (63.4) | 3,271 (71.2) | 334 (67.3) | <0.001 |
| Number of services, mean (SD)b | 5.4 (6.8) | 7.8 (9.8) | 8.8 (11.2) | 7.3 (8.4) | <0.001 |
Notes:
Overall P-value indicates statistical difference across all cohorts;
this outcome computed among patients with visits or services.
Abbreviations: CP, chronic pain; LAO, long-acting opioid; LOS, length of stay; OP, outpatient; SAO, short-acting opioid.
Discussion
The majority (74.1%) of patients in the current study used only SAOs, while 21.7% used a combination of SAOs and LAOs. Only 2.3% switched between SAOs and LAOs (or vice versa), and 1.9% used LAOs exclusively. LAOs are indicated for around-the-clock pain and can be used either alone or in combination with SAOs to manage patients with severe continuous pain.7,21 However, according to this analysis, the majority of patients with CNCP are using SAOs exclusively. The average daily MED in the current study was lowest in the mono-SAO cohort (36.2 mg) and highest in the mono-LAO cohort (84.6 mg), which is similar to what has been observed previously.7,22
This study observed that CNCP patients who used LAO monotherapy had lower costs and potentially better clinical outcomes than those CNCP patients using other long-term opioid treatment regimens. Despite having the highest prescription costs in the mono-LAO cohort, total CNCP-related costs were lowest for these patients. While total annual prescription costs were lowest in the mono-SAO cohort ($853) and highest in the mono-LAO cohort ($2,814), total costs were higher in the mono-SAO cohort ($8,604) than in the mono-LAO cohort ($4,933). Patients in the mono-LAO cohort had the lowest rates of medical utilization in all categories, including hospitalizations and ED visits and used concomitant pain medications (except antidepressants) and other treatment modalities (particularly epidurals, physical therapy, nerve blocks, TENS, and intrathecal drug therapies) at a lower rate than patients using other opioid regimens. This may imply a reduced need for additional therapies because of greater pain relief obtained with the observed higher daily doses and greater days of use among mono-LAO patients. More adequate pain relief may also have resulted in less need for other more invasive interventions, such as surgery, as evidenced by the lower rates of hospitalizations. While differences in baseline characteristics (e.g., age, CNCP diagnosis) could potentially affect costs and health care utilization rates, baseline characteristics were accounted for in the analyses of these outcomes.
The general description of opioid users at baseline in our study is similar to that of previous reports. Hudson et al described opioid users from a general household survey and observed that patients had multiple pain conditions and comorbidities, as was noted in the current analysis.23 However, in our population, the mono-LAO cohort had poorer health status, as evidenced by a higher CCI than the other cohorts. Our population was also similar to other CNCP cohorts described in claims analyses. For example, Gore et al described the health care costs of CNCP patients relative to controls. In the CNCP cohort, total direct costs (2008; cause not specified) were $11,829 to $15,368, depending on diagnosis.24 In our study, total CNCP-related costs ranged from $4,933 to $15,190, depending on opioid-user type. Gore et al also found that 20% of total costs were attributable to prescription drugs.24 During the 1-year follow-up in our study, 12.5% of costs were attributable to CNCP-related prescription drugs and ranged from 10% to 57% of total costs, depending on the opioid regimen.
While there is substantial literature to describe opioid use and its economic impact on payers and patients,20,25–28 our study is unique in that it is specific to CNCP and assessed costs and health care utilization by opioid regimen among long-term opioid users. To our knowledge, a study that specifically looks at CNCP-specific health care utilization and cost outcomes by opioid regimen has not previously been published.
These findings should be of particular interest to primary care providers (PCPs), as ~50% of CP patients are treated by PCPs,29 and PCPs are responsible for nearly 30% of all opioid prescriptions.30 It is pertinent to look at the available data by opioid regimen, because while LAOs were developed and initially used based on the potential clinical benefits associated with their long-acting pharmacokinetic profile, clinical data substantiating these benefits are scarce. The current real-world data presented here begin to fill this evidence gap. These data suggest that using LAOs to manage CNCP is associated with the tangible benefits of decreased hospitalizations, ED visits, office visits, and the resulting total costs.
As with all claims database studies there are several limitations that must be considered when interpreting the results. Claims data are not collected for research; thus, the accuracy and completeness of the available data may be limited. Also, data on pain severity, pain control, and impact of pain on daily activities are not available. In addition, claims data are only indicative of prescription filling behavior and may not correlate with actual usage.
This study evaluated new initiators of opioid therapy; thus, the mono-LAO cohort by definition initiated opioid therapy directly on an LAO and may represent a unique subset of patients. The study was limited in considering individual or aggregate patient pain characteristics such as severity and duration of pain as these variables are not available in claims data. Claims data are limited as there is no indication of the reasons for observed patterns of care. Future studies should evaluate the nature and extent of this patient population. It is possible that these patients initiated opioid therapy with an SAO during an inpatient stay; however, information on the use of inpatient drug use is not available in administrative claims data to confirm this hypothesis.
In this study specifically, the LAO cohort was small relative to the other cohorts; however, the differences found between this and the other cohorts were sufficiently large to conclude that the observed differences were unlikely to have arisen by chance. On the other hand, statistically significant differences may have been driven by the large sample size, and future studies could investigate specific between-group differences. This study served as an exploratory assessment of costs by pattern of opioid use. Additionally, certain assumptions were made when delineating the cohorts. The use of SAOs may be on an as-needed basis. In an attempt to control for this, a stable dosing schedule was assumed for CP, and days supply and quantity were used to calculate average daily dose. However, this may underestimate the average daily dose for patients using SAO formulations. In this study, we found that mono-SAO patients had the lowest days supply and a greater use of alternative prescription and medical treatments.
Conclusion
The current data are intriguing and suggest that there is a need for further investigation of the use of long-term LAO therapies in the treatment of CNCP. Patients treated with mono-LAO therapy received higher opioid doses, had less use of other pain-relieving treatment modalities, and had lower costs and health care utilization, including hospitalizations and ED visits than patients treated with mono-SAOs or other opioid regimens. This study provides initial evidence that how opioids are used and may be important for optimizing clinical outcomes. Results also suggest a specific role for use of LAOs in the management of CNCP patients. Further research, such as clinical trials or observational studies that directly measure pain intensity and treatment tolerability, is needed to confirm that the health care cost and utilization benefits of LAO monotherapy observed in the current study translate to measurable clinical efficacy and/or safety benefits.
Acknowledgments
Funding for this research study was provided by Teva Pharmaceuticals. Bethany Sawchyn provided writing support for the manuscript. Editorial assistance was provided by Peloton Advantage and was funded by Teva Global Health Economics and Outcomes Research (Frazer, PA). Teva provided a full review of the article.
Data presented at the National Conference on Pain (PAIN-Week), September 8–12, 2015, Las Vegas, NV.
Footnotes
Disclosure
KG and PPY are employees of Teva Pharmaceuticals, Inc. RW was an employee of Teva Pharmaceuticals, Inc., at the time this research was conducted. PBL-B and AOD are employees of Xcenda, which has received research funding from Teva Pharmaceuticals, Inc., for the conduct of this study and for the preparation of this manuscript. SLC was an employee of Xcenda at the time this research was conducted; he is now an employee of Galaxy Informatica, Maharashtra, India. NK has received research funding and consulting fees from Teva Pharmaceuticals, Inc. The authors report no other conflicts of interest in this work.
References
- 1.Institute of Medicine Relieving pain in America: a blueprint for transforming prevention, care, education, and research. 2011. [Accessed December 16, 2016]. Available from: http://nationalacademies.org/HMD/Reports/2011/Relieving-Pain-in-America-A-Blueprint-for-Transforming-Prevention-Care-Education-Research.aspx.
- 2.Nahin RL. Estimates of pain prevalence and severity in adults: United States, 2012. J Pain. 2015;16(8):769–780. doi: 10.1016/j.jpain.2015.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gaskin DJ, Richard P. The economic costs of pain in the United States. J Pain. 2012;13(8):715–724. doi: 10.1016/j.jpain.2012.03.009. [DOI] [PubMed] [Google Scholar]
- 4.American Society of Anesthesiologists Task Force on Chronic Pain Management. American Society of Regional Anesthesia and Pain Medicine Practice guidelines for chronic pain management: an updated report by the American Society of Anesthesiologists Task Force on chronic pain management and the American Society of Regional Anesthesia and Pain Medicine. Anesthesiology. 2010;112(4):810–833. doi: 10.1097/ALN.0b013e3181c43103. [DOI] [PubMed] [Google Scholar]
- 5.Conaghan PG, Peloso PM, Everett SV, et al. Inadequate pain relief and large functional loss among patients with knee osteoarthritis: evidence from a prospective multinational longitudinal study of osteoarthritis real-world therapies. Rheumatology. 2015;54(2):270–277. doi: 10.1093/rheumatology/keu332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ziegler D. Painful diabetic neuropathy: advantage of novel drugs over old drugs? Diabetes Care. 2009;32(Suppl 2):S414–S419. doi: 10.2337/dc09-S350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dowell D, Haegerich TM, Chou R. CDC guideline for prescribing opioids for chronic pain—United States, 2016. MMWR Recomm Rep. 2016;65(1):1–49. doi: 10.15585/mmwr.rr6501e1. [DOI] [PubMed] [Google Scholar]
- 8.Manchikanti L, Abdi S, Atluri S, et al. American Society of Interventional Pain Physicians (ASIPP) guidelines for responsible opioid prescribing in chronic non-cancer pain: part I—evidence assessment. Pain Physician. 2012;15(Suppl 3):S1–S65. [PubMed] [Google Scholar]
- 9.Fine PG, Mahajan G, McPherson ML. Long-acting opioids and short-acting opioids: appropriate use in chronic pain management. Pain Med. 2009;10(Suppl 2):S79–S88. doi: 10.1111/j.1526-4637.2009.00666.x. [DOI] [PubMed] [Google Scholar]
- 10.Agency Medical Directors’ Group (AMDG) Interagency guideline on prescribing opioids for pain. 2015. [Accessed December 16, 2016]. Available from: http://www.agencymeddirectors.wa.gov.
- 11.American Pain Society in conjunction with the American Academy of Pain Medicine (APS-AAPM) Guideline for the use of chronic opioid therapy in chronic noncancer pain: evidence review. 2009. [Accessed December 16, 2016]. Available from: http://americanpainsociety.org/uploads/education/guidelines/chronic-opioid-therapy-cncp.pdf.
- 12.Califf RM, Woodcock J, Ostroff S. A proactive response to prescription opioid abuse. N Engl J Med. 2016;374(15):1480–1485. doi: 10.1056/NEJMsr1601307. [DOI] [PubMed] [Google Scholar]
- 13.Chou R, Fanciullo GJ, Fine PG, et al. Clinical guidelines for the use of chronic opioid therapy in chronic noncancer pain. J Pain. 2009;10(2):113–130. doi: 10.1016/j.jpain.2008.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Franklin GM, American Academy of Neurology Opioids for chronic noncancer pain: a position paper of the American Academy of Neurology. Neurology. 2014;83(14):1277–1284. doi: 10.1212/WNL.0000000000000839. [DOI] [PubMed] [Google Scholar]
- 15.Hegmann KT, Weiss MS, Bowden K, et al. ACOEM practice guidelines: opioids for treatment of acute, subacute, chronic, and postoperative pain. J Occup Environ Med. 2014;56(12):e143–e159. doi: 10.1097/JOM.0000000000000352. [DOI] [PubMed] [Google Scholar]
- 16.Kahan M, Mailis-Gagnon A, Wilson L, Srivastava A, National Opioid Use Guideline Group Canadian guideline for safe and effective use of opioids for chronic noncancer pain: clinical summary for family physicians. Part 1: general population. Can Fam Physician. 2011;57(11):1257–1266. e407–e418. [PMC free article] [PubMed] [Google Scholar]
- 17.The Federation of State Medical Boards (FSMB) of the United States I Model guidelines for the use of controlled substance for the treatment of pain. 1998. [Accessed December 16, 2016]. Available from: http://www.painpolicy.wisc.edu/sites/www.painpolicy.wisc.edu/files/model_0.pdf.
- 18.Pedersen L, Borchgrevink PC, Riphagen II, Fredheim OM. Long- or short-acting opioids for chronic non-malignant pain? A qualitative systematic review. Acta Anaesthesiol Scand. 2014;58(4):390–401. doi: 10.1111/aas.12279. [DOI] [PubMed] [Google Scholar]
- 19.Kozma CM, Provenzano DA, Slaton TL, Patel AA, Benson CJ. Complexity of pain management among patients with nociceptive or neuropathic neck, back, or osteoarthritis diagnoses. J Manag Care Spec Pharm. 2014;20(5):455b–466b. doi: 10.18553/jmcp.2014.20.5.455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Leider HL, Dhaliwal J, Davis EJ, Kulakodlu M, Buikema AR. Healthcare costs and nonadherence among chronic opioid users. Am J Manag Care. 2011;17(1):32–40. [PubMed] [Google Scholar]
- 21.United States Food and Drug Administration (FDA) FDA announces safety labeling changes and postmarket study requirements for extended-release and long-acting opioid analgesics. 2013. [Accessed December 16, 2016]. Available from: http://www.fda.gov/newsevents/newsroom/pressannouncements/ucm3,67,726.htm.
- 22.Von Korff M, Merrill JO, Rutter CM, Sullivan M, Campbell CI, Weisner C. Time-scheduled vs. pain-contingent opioid dosing in chronic opioid therapy. Pain. 2011;152(6):1256–1262. doi: 10.1016/j.pain.2011.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hudson TJ, Edlund MJ, Steffick DE, Tripathi SP, Sullivan MD. Epidemiology of regular prescribed opioid use: results from a national, population-based survey. J Pain Symptom Manag. 2008;36(3):280–288. doi: 10.1016/j.jpainsymman.2007.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gore M, Sadosky A, Stacey BR, Tai KS, Leslie D. The burden of chronic low back pain: clinical comorbidities, treatment patterns, and health care costs in usual care settings. Spine. 2012;37(11):E668–E677. doi: 10.1097/BRS.0b013e318241e5de. [DOI] [PubMed] [Google Scholar]
- 25.Anastassopoulos KP, Chow W, Tapia CI, et al. Economic study on the impact of side effects in patients taking oxycodone controlled-release for noncancer pain. J Manag Care Pharm. 2012;18(8):615–626. doi: 10.18553/jmcp.2012.18.8.615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Berger A, Sadosky A, Dukes EM, Edelsberg J, Zlateva G, Oster G. Patterns of healthcare utilization and cost in patients with newly diagnosed fibromyalgia. Am J Manag Care. 2010;16(Suppl 5):S126–S137. [PubMed] [Google Scholar]
- 27.Ivanova JI, Birnbaum HG, Yushkina Y, Sorg RA, Reed J, Merchant S. The prevalence and economic impact of prescription opioid-related side effects among patients with chronic noncancer pain. J Opioid Manag. 2013;9(4):239–254. doi: 10.5055/jom.2013.0165. [DOI] [PubMed] [Google Scholar]
- 28.Mosher HJ, Jiang L, Vaughan Sarrazin MS, Cram P, Kaboli PJ, Vander Weg MW. Prevalence and characteristics of hospitalized adults on chronic opioid therapy. J Hosp Med. 2014;9(2):82–87. doi: 10.1002/jhm.2113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Breuer B, Cruciani R, Portenoy RK. Pain management by primary care physicians, pain physicians, chiropractors, and acupuncturists: a national survey. South Med J. 2010;103(8):738–747. doi: 10.1097/SMJ.0b013e3181e74ede. [DOI] [PubMed] [Google Scholar]
- 30.Volkow N, McLellan TA, Cotto JH, Karithanom M, Weiss SR. Characteristics of opioid prescriptions in 2009. JAMA. 2011;305(13):1299–1301. doi: 10.1001/jama.2011.401. [DOI] [PMC free article] [PubMed] [Google Scholar]