Abstract
Purpose
The preoperative diagnosis of acute appendicitis is often challenging. Sometimes, pathologic results of the appendix embarrass or confuse surgeons. Therefore, more and more imaging studies are being performed to increase the accuracy of appendicitis diagnoses preoperatively. However, data on the effect of this increase in preoperative imaging studies on diagnostic accuracy are limited. We performed this study to explore unexpected appendiceal pathologies and to delineate the role of preoperative imaging studies in the diagnosis of acute appendicitis.
Methods
The medical records of 4,673 patients who underwent an appendectomy for assumed appendicitis between 1997 and 2012 were reviewed retrospectively. Pathological results and preoperative imaging studies were surveyed, and the frequencies of pathological results and preoperative imaging studies were investigated.
Results
The overall rate of pathology compatible with acute appendicitis was 84.4%. Unexpected pathological findings, such as normal histology, specific inflammations other than acute appendicitis, neoplastic lesions, and other pathologies, comprised 9.6%, 3.3%, 1.2%, and 1.5%, respectively. The rate of unexpected pathological results was significantly reduced because of the increase in preoperative imaging studies. The decrease in normal appendices contributed the most to the reduction while other unexpected pathologies did not change significantly despite the increased use of imaging studies. This decrease in normal appendices was significant in both male and female patients under the age of 60 years, but the differences in females were more prominent.
Conclusion
Unexpected appendiceal pathologies comprised 15.6% of the cases. Preoperative imaging studies reduced them by decreasing the negative appendectomy rate of patients with normal appendices.
Keywords: Appendicitis, Appendectomy, Diagnosis, Pathology
INTRODUCTION
Acute appendicitis is one of the most common emergency surgeries; however, the preoperative diagnosis of acute appendicitis is frequently challenging [1,2] and the negative appendectomy rate has not changed for decades [3]. In addition, the pathogenesis of acute appendicitis has been the subject of debate. The conventionally accepted pathogenesis—obstruction of the appendiceal lumen causes bacterial growth, induces progressive inflammation, and results in perforation—has been criticized for its limited clinical relevance [4,5]. Some reports on the differences in the early courses between perforated and nonperforated appendicitis have suggested that the conventionally accepted mechanism should be revised [6,7].
The pathological results of an appendectomy in patients with right lower quadrant abdominal pain and imaging findings suggesting acute appendicitis can show various pathologies and even appendiceal tumors in about 3% of the appendectomy specimens [8]. These indicate that surgeons should be not only qualified in the accurate preoperative diagnosis of acute appendicitis but also aware of all appendix-related diseases and the postoperative care for those diseases after emergent appendectomy.
Unexpected appendiceal pathological results after appendectomies in patients with suspected acute appendicitis are not rare. These cases may require additional postoperative therapies, disturb the positive rapport between surgeons and patients, and create medico-legal problems [8]. Thus, surgeons are relying on imaging studies for more and more cases to increase the diagnostic accuracy preoperatively [2,8]. However, few studies have examined whether preoperative imaging studies are always helpful for all patients with suspected acute appendicitis. Thus, this study was designed to explore the unexpected appendiceal pathologies of patients who had undergone an appendectomy after a clinical diagnosis of acute appendicitis and to evaluate the effects of imaging studies on the frequency of unexpected appendiceal pathologies.
METHODS
We enrolled patients who had undergone an appendectomy with a preoperative diagnosis of acute appendicitis between January 1997 and December 2012 at Seoul Metropolitan Government - Seoul National University Boramae Medical Center, Seoul, Korea. Patients with incidental appendectomies during other intra-abdominal surgeries, with simultaneous resection of other organs due to other surgical diseases, or with lost pathological results were excluded. The medical records were reviewed retrospectively for clinical and pathological data, as were imaging studies. Computed tomography (CT) or ultrasonography (US) was performed for the preoperative imaging studies.
For the classification of the pathological results, acute appendicitis was defined as the finding of pathological changes of the appendix with obstructive inflammation, intraluminal distention, and mucosal ischemia. The pathological descriptions of the acute appendicitis group were as follows: acute appendicitis, acute suppurative appendicitis, suppurative appendicitis with microperforation, gangrenous appendicitis, gangrenous appendicitis with periappendiceal abscess, etc. [4,9]. The other findings were categorized into unexpected appendiceal pathologies, which were subdivided into the normal appendix group, the specific inflammatory pathology group, the neoplasm group, and the others group. We investigated the proportions of these subgroups according to age and the presence of preoperative imaging studies. Additionally, we explored whether the imaging studies had different effects on the rates of unexpected pathological results in different genders and in various age groups. To do so, we compared 2 groups of patients: a group in which less than 30% had undergone preoperative imaging studies (patients between 1997 and 2001) and a group in which more than 90% had undergone preoperative imaging studies (patients between 2006 and 2012).
The chi-square test was used to analyze the proportional differences between acute appendicitis and unexpected appendiceal pathologies according to whether preoperative imaging studies had been conducted or not. Bonferroni correction was applied to the multiple comparisons among subgroups of the unexpected pathology subgroup. The Cochran-Mantel-Haenszel chi-square trend test was used to evaluate the changes in the subgroups of unexpected appendiceal pathologies associated with the proportions of preoperative imaging studies. IBM SPSS Statistics ver. 20.0 (IBM Co., Armonk, NY, USA) was used for the statistical analyses. This study was approved by the Institutional Review Board of Seoul Metropolitan Government - Seoul National University Boramae Medical Center (approval number: 16-2014-160).
RESULTS
The number of patients enrolled in this study was 4,673. The average age was 33.0 ± 18.4 years, with those in their twenties occupying the largest proportion (26.3%). Of the patients 2,585 (55.3%) were men.
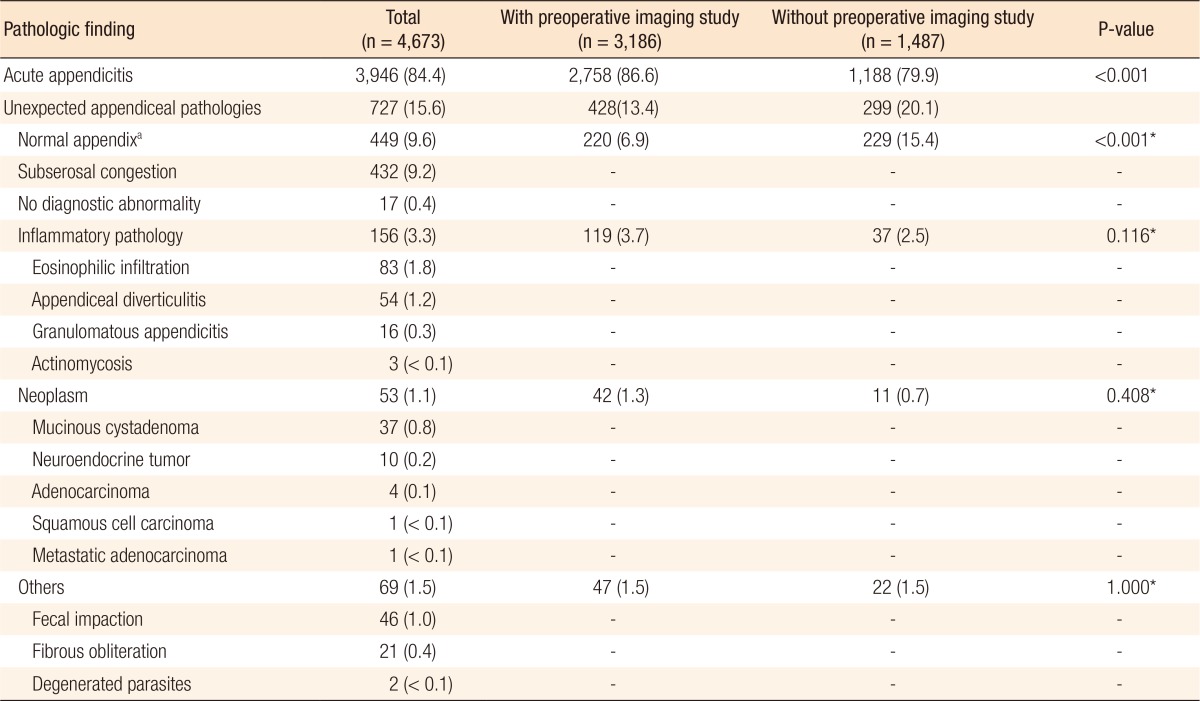
Unexpected appendiceal pathologies other than acute appendicitis were found in 15.6% of the cases. A histologically normal appendix, which was reported as “subserosal congestion without inflammatory cells” or “no diagnostic abnormality,” was found in the majority of unexpected pathologies (449 cases, 9.6%). “Specific inflammatory pathology,” which could not be diagnosed as acute appendicitis under the definition of acute appendicitis, was found in 156 cases (3.3%) and included actinomycosis, diverticulitis, and granulomatous appendicitis. Neoplastic lesions were found in 1.1% (53) of the cases. Other pathological results, such as fecal impaction and degenerative parasites, were found in 1.5% (69) of the cases (Table 1).
Table 1. Characteristics of 4,673 patients with appendiceal pathologic findings.
Values are presented as number (%).
aBonferroni corrected P-value for multiple comparisons.
The proportions of unexpected appendiceal pathologies in patients with and without preoperative imaging were 13.4% and 20.1%, respectively, and this difference was statistically significant (P < 0.001). In the subgroup analyses, the “normal appendix” occupied a lower proportion (6.9%) when preoperative imaging studies had been performed than when they had not been performed (15.4%; P < 0.001, Bonferroni corrected); however, no significant differences were found in the other subgroups (Table 1).
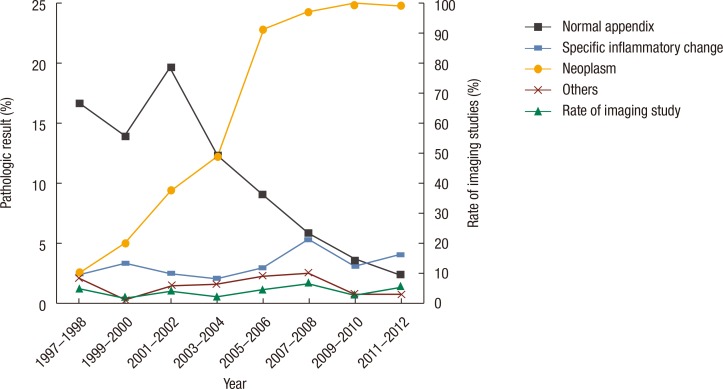
During the study period, the rate of preoperative imaging studies continuously increased, and the proportion of “normal appendix” continuously decreased. However, the rates of the other subgroups did not show significant changes. That is, the increase in preoperative imaging studies decreased appendectomies of normal appendices but did not decrease appendectomies of other pathologies. Therefore, the decrease of “normal appendix” explained the reduction in unexpected appendiceal pathologies (Fig. 1).
Fig. 1. Changes in the pathologic results and the rate of preoperative imaging studies from 1997 to 2012.
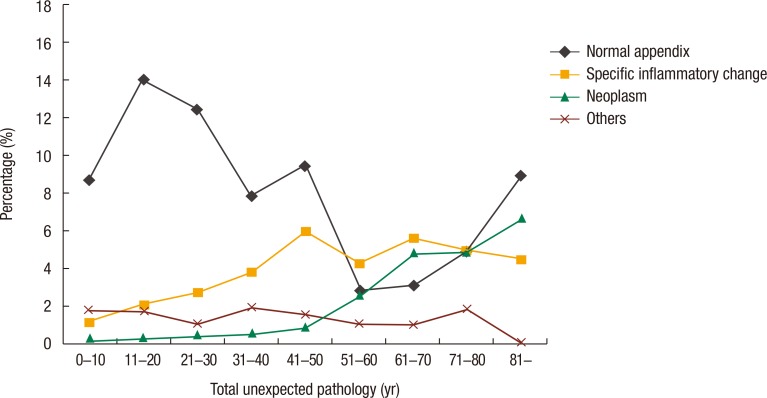
The proportions of total unexpected appendiceal pathologies were found not to differ according to age (data not shown). However, in the subgroup analyses, “normal appendix” showed a higher proportion in younger patients (under 50 years old) while “specific inflammatory pathology” increased after the fourth decade. “Neoplasm” reached higher and higher proportions as the age increased (Fig. 2).
Fig. 2. Unexpected appendiceal pathology subgroups according to the age groups.
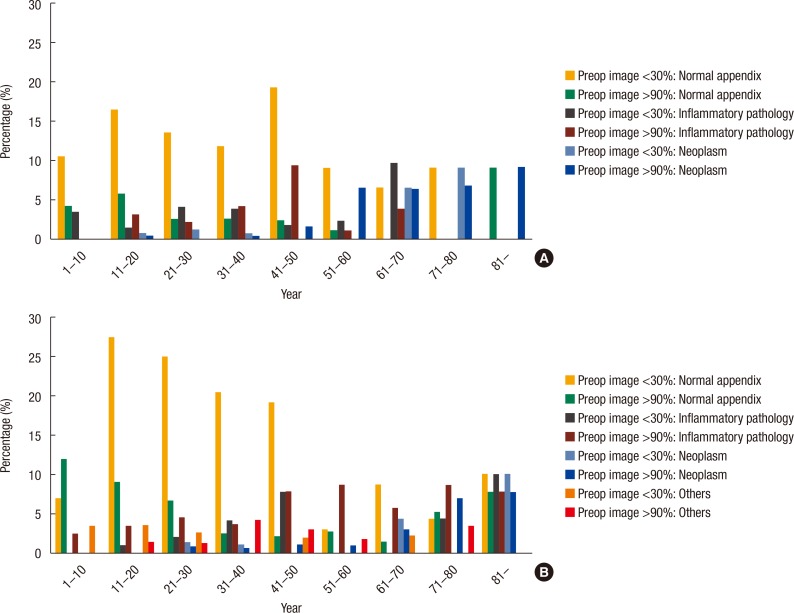
To examine the role of imaging studies in male and female patients of various ages, we compared two groups of patients: a group in which less than 30% underwent preoperative imaging studies and another group in which more than 90% underwent preoperative imaging studies. Both male and female patients under 60 years old showed a significantly lower proportion of unexpected appendiceal pathologies in the group with more than 90% imaging than those in the group with less than 30% imaging did (data not shown). As for the subgroups of unexpected pathologies, only “normal appendix” showed a significantly lower proportion in the group with a high preoperative imaging rate, showing more prominent differences in female patients (P < 0.001, Cochran-Mantel-Haenszel method) (Fig. 3).
Fig. 3. The trends of unexpected appendiceal pathology subgroups according to the age groups and sex with the use of preoperative image studies: male (A) and female patients (B).
DISCUSSION
Many studies have categorized appendiceal pathologies. Blair et al. [10] and Choi et al. [11] showed various pathological findings regarding the appendix without specific groupings. Gupta et al. [12] classified pathological results into 5 groups: normal, inflammatory lesions, tubercular appendicitis, parasitic infestations, and tumorous conditions. In this study, we set the grouping based on not only pathology but also clinical demands, such as additional treatment after an appendectomy or prognosis, to facilitate clinical use. This grouping can be useful when surgeons give information to patients or when doctors or medical personnel are educated on unexpected pathological findings. Surgeons should be aware of further evaluation and treatment strategies after an appendectomy for patients with the pathologies of neoplastic lesions, tuberculosis, actinomycosis, and so on [8,13,14,15]. In this study, we explored more specific data on the distribution of unexpected appendiceal pathologies according to age and gender.
Pelvic inflammatory disease and ovarian disease in women of childbearing age are frequently confused with acute appendicitis [16]; however, their negative appendectomy rates were significantly decreased with the introduction of preoperative abdominal CT [17,18]. This study also showed a significant decrease in the negative appendectomy rate with preoperative imaging studies in patients aged under 60 years, especially in young female patients (although this was not statistically significant) (Fig. 3B). Before imaging studies became popular for patients with abdominal pain, patients sometimes underwent an appendectomy with exploration of the intra-abdominal cavity to rule out appendicitis as compared to other diseases, such as pelvic inflammatory disease causing right lower quadrant abdominal pain [4]. However, with preoperative imaging studies now being performed in most patients, this procedure has almost disappeared from clinical practice, and initial nonsurgical therapy with follow-up imaging, rather than immediate surgery, tends to be the standard management strategy in patients with mild symptoms or an ambiguous diagnosis [14]. These changes have probably contributed, at least to some extent, to the decrease in the negative appendectomy rate, especially in women.
Although CT scanning and US are very helpful imaging techniques in the diagnosis of intraabdominal conditions, the proportions of subgroups of unexpected appendiceal pathologies (except for “normal appendix”) did not change. This implies that imaging techniques have inevitable limitations for differentiating acute appendicitis from other diseases, such as appendiceal diverticulitis or granulomatous inflammation [17,19]. In other words, an appendectomy cannot be avoided when enlargement of the appendix and periappendiceal infiltration are revealed in spite of the absence of a typical clinical history, such as initial periumbilical or epigastric pain and subsequent migration to the right lower quadrant. Thus, in some patients, imaging studies serve to detect the surgical condition of the appendix rather than discriminate acute appendicitis from a normal appendix. Friedlich et al. [20] and Lee et al. [21] reported that appendiceal diverticulitis could be detected with high sensitivity by thin-section CT scanning, but considering the incidence of appendiceal diverticulitis, the application of thin-section CT scans in selective patients is not practical and the consequences of excessive radiation exposure should be taken into account [22]. Regarding the diagnostic accuracy, those of CT and US were 88.3% and 76%, respectively (P < 0.001). However, CT and US were not performed independently. Most of the ultrasonographies were performed when the patient was pregnant or possibly pregnant, when the quality of CT images were not satisfactory, or when the CT was not available. Therefore, in this retrospective study, a comparison of the diagnostic accuracies between CT and US was not appropriate.
In this study, both male and female members of the “normal appendix” group still comprised 2% to 5%, even after 2007 when over 90% of patients underwent preoperative imaging studies. This phenomenon was noticeable. Further studies are needed to investigate whether this phenomenon was caused by the limitations of imaging tools or individual characteristics. This limitation suggests that the evaluation of the clinical index, which was recently discredited due to the development and easy accessibility of imaging tools, should be stressed again. Therefore, recent trials to reduce imaging studies by adopting clinical indices, such as the Alvarado score, are worthy of attention [23,24,25]. The scoring system proposed by Atema et al. [26], which uses simpler and more distinguishable imaging features, showed high predictability for uncomplicated acute appendicitis, and this system is expected to aid the diagnosis of uncomplicated acute appendicitis, as well as atypical appendiceal pathologies in which nonoperative management would be preferred. Further studies are needed to develop an adequate algorithm to implement CT scans with a high cost-effectiveness ratio to reduce unnecessary imaging studies as well as negative appendectomies.
This retrospective study has some limitations. Firstly, we could show neither the pathological spectrum of patients with right lower quadrant abdominal pain nor the rate of patients who underwent procedures other than an appendectomy. Secondly, because this is a retrospective study, there was no uniform standard indication for the imaging study in patients with assumed appendicitis. In the early study period, preoperative imaging studies were performed in cases only where ruling out a diagnosis other than appendicitis was difficult due to high cost and the low quality of imaging studies. During the late period, the cost was covered by national health insurance, the quality of the CT scan was improved, and most importantly, the first doctors who examined the patients were not surgeons, but physicians in the Department of Emergency Medicine. That is why almost all patients underwent an imaging study in the late period. Therefore, we could not delineate a more detailed role of imaging studies according to the clinical situation.
In conclusion, this study revealed various pathologies of the appendix and their proportions in cases of appendectomies with suspected acute appendicitis. Preoperative imaging studies decreased the negative appendectomy rate in men and women under the age of 60 years. However, preoperative imaging studies did not reduce unexpected appendiceal pathologies other than normal appendix findings. Surgeons should be aware of these efficacies and limitations of imaging studies in the diagnosis of acute appendicitis.
Footnotes
CONFLICT OF INTEREST: No potential conflict of interest relevant to this article was reported.
References
- 1.Bickell NA, Aufses AH, Jr, Rojas M, Bodian C. How time affects the risk of rupture in appendicitis. J Am Coll Surg. 2006;202:401–406. doi: 10.1016/j.jamcollsurg.2005.11.016. [DOI] [PubMed] [Google Scholar]
- 2.SCOAP Collaborative. Cuschieri J, Florence M, Flum DR, Jurkovich GJ, Lin P, et al. Negative appendectomy and imaging accuracy in the Washington State Surgical Care and Outcomes Assessment Program. Ann Surg. 2008;248:557–563. doi: 10.1097/SLA.0b013e318187aeca. [DOI] [PubMed] [Google Scholar]
- 3.Boonstra PA, van Veen RN, Stockmann HB. Less negative appendectomies due to imaging in patients with suspected appendicitis. Surg Endosc. 2015;29:2365–2370. doi: 10.1007/s00464-014-3963-2. [DOI] [PubMed] [Google Scholar]
- 4.Carr NJ. The pathology of acute appendicitis. Ann Diagn Pathol. 2000;4:46–58. doi: 10.1016/s1092-9134(00)90011-x. [DOI] [PubMed] [Google Scholar]
- 5.Andersson RE. The natural history and traditional management of appendicitis revisited: spontaneous resolution and predominance of prehospital perforations imply that a correct diagnosis is more important than an early diagnosis. World J Surg. 2007;31:86–92. doi: 10.1007/s00268-006-0056-y. [DOI] [PubMed] [Google Scholar]
- 6.Livingston EH, Woodward WA, Sarosi GA, Haley RW. Disconnect between incidence of nonperforated and perforated appendicitis: implications for pathophysiology and management. Ann Surg. 2007;245:886–892. doi: 10.1097/01.sla.0000256391.05233.aa. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lee KH, Lee HS, Park SH, Bajpai V, Choi YS, Kang SB, et al. Appendiceal diverticulitis: diagnosis and differentiation from usual acute appendicitis using computed tomography. J Comput Assist Tomogr. 2007;31:763–769. doi: 10.1097/RCT.0b013e3180340991. [DOI] [PubMed] [Google Scholar]
- 8.Akbulut S, Tas M, Sogutcu N, Arikanoglu Z, Basbug M, Ulku A, et al. Unusual histopathological findings in appendectomy specimens: a retrospective analysis and literature review. World J Gastroenterol. 2011;17:1961–1970. doi: 10.3748/wjg.v17.i15.1961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Prystowsky JB, Pugh CM, Nagle AP. Current problems in surgery. Appendicitis. Curr Probl Surg. 2005;42:688–742. doi: 10.1067/j.cpsurg.2005.07.005. [DOI] [PubMed] [Google Scholar]
- 10.Blair NP, Bugis SP, Turner LJ, MacLeod MM. Review of the pathologic diagnoses of 2,216 appendectomy specimens. Am J Surg. 1993;165:618–620. doi: 10.1016/s0002-9610(05)80446-5. [DOI] [PubMed] [Google Scholar]
- 11.Choi YW, Lee NH, Kim SY. Diagnostic accuracy and complications of acute appendicitis and incidence and complications of negative explorations in 3,303 cases of suspected appendicitis. J Korean Surg Soc. 1995;49:268–276. [Google Scholar]
- 12.Gupta SC, Gupta AK, Keswani NK, Singh PA, Tripathi AK, Krishna V. Pathology of tropical appendicitis. J Clin Pathol. 1989;42:1169–1172. doi: 10.1136/jcp.42.11.1169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shapiro R, Eldar S, Sadot E, Papa MZ, Zippel DB. Appendiceal carcinoid at a large tertiary center: pathologic findings and long-term follow-up evaluation. Am J Surg. 2011;201:805–808. doi: 10.1016/j.amjsurg.2010.04.016. [DOI] [PubMed] [Google Scholar]
- 14.AbdullGaffar B. Granulomatous diseases and granulomas of the appendix. Int J Surg Pathol. 2010;18:14–20. doi: 10.1177/1066896909349246. [DOI] [PubMed] [Google Scholar]
- 15.Nissotakis C, Sakorafas GH, Koureta T, Revelos K, Kassaras G, Peros G. Actinomycosis of the appendix: diagnostic and therapeutic considerations. Int J Infect Dis. 2008;12:562–564. doi: 10.1016/j.ijid.2007.12.015. [DOI] [PubMed] [Google Scholar]
- 16.Morishita K, Gushimiyagi M, Hashiguchi M, Stein GH, Tokuda Y. Clinical prediction rule to distinguish pelvic inflammatory disease from acute appendicitis in women of childbearing age. Am J Emerg Med. 2007;25:152–157. doi: 10.1016/j.ajem.2006.06.013. [DOI] [PubMed] [Google Scholar]
- 17.Flum DR, Morris A, Koepsell T, Dellinger EP. Has misdiagnosis of appendicitis decreased over time? A population-based analysis. JAMA. 2001;286:1748–1753. doi: 10.1001/jama.286.14.1748. [DOI] [PubMed] [Google Scholar]
- 18.Terasawa T, Blackmore CC, Bent S, Kohlwes RJ. Systematic review: computed tomography and ultrasonography to detect acute appendicitis in adults and adolescents. Ann Intern Med. 2004;141:537–546. doi: 10.7326/0003-4819-141-7-200410050-00011. [DOI] [PubMed] [Google Scholar]
- 19.Chiou YY, Pitman MB, Hahn PF, Kim YH, Rhea JT, Mueller PR. Rare benign and malignant appendiceal lesions: spectrum of computed tomography findings with pathologic correlation. J Comput Assist Tomogr. 2003;27:297–306. doi: 10.1097/00004728-200305000-00001. [DOI] [PubMed] [Google Scholar]
- 20.Friedlich M, Malik N, Lecompte M, Ayroud Y. Diverticulitis of the appendix. Can J Surg. 2004;47:146–147. [PMC free article] [PubMed] [Google Scholar]
- 21.Lee KH, Kim YH, Hahn S, Lee KW, Kim TJ, Kang SB, et al. Computed tomography diagnosis of acute appendicitis: advantages of reviewing thin-section datasets using sliding slab average intensity projection technique. Invest Radiol. 2006;41:579–585. doi: 10.1097/01.rli.0000221999.22095.b7. [DOI] [PubMed] [Google Scholar]
- 22.Brenner D, Elliston C, Hall E, Berdon W. Estimated risks of radiation-induced fatal cancer from pediatric CT. AJR Am J Roentgenol. 2001;176:289–296. doi: 10.2214/ajr.176.2.1760289. [DOI] [PubMed] [Google Scholar]
- 23.Ohle R, O'Reilly F, O'Brien KK, Fahey T, Dimitrov BD. The Alvarado score for predicting acute appendicitis: a systematic review. BMC Med. 2011;9:139. doi: 10.1186/1741-7015-9-139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jones RP, Jeffrey RB, Shah BR, Desser TS, Rosenberg J, Olcott EW. Journal Club: the Alvarado score as a method for reducing the number of CT studies when appendiceal ultrasound fails to visualize the appendix in adults. AJR Am J Roentgenol. 2015;204:519–526. doi: 10.2214/AJR.14.12864. [DOI] [PubMed] [Google Scholar]
- 25.Tan WJ, Pek W, Kabir T, Goh YC, Chan WH, Wong WK, et al. Alvarado score: a guide to computed tomography utilization in appendicitis. ANZ J Surg. 2013;83:748–752. doi: 10.1111/ans.12076. [DOI] [PubMed] [Google Scholar]
- 26.Atema JJ, van Rossem CC, Leeuwenburgh MM, Stoker J, Boermeester MA. Scoring system to distinguish uncomplicated from complicated acute appendicitis. Br J Surg. 2015;102:979–990. doi: 10.1002/bjs.9835. [DOI] [PubMed] [Google Scholar]