Abstract
Takotsubo cardiomyopathy (TCM) is a relatively recently recognised clinical entity. It frequently mimics acute coronary syndrome and is accompanied by reversible left ventricular apical ballooning in the absence of angiographically significant coronary artery stenosis. TCM is a reversible condition, and the prognosis is usually well. However, in rare instances, it can be associated with life-threatening arrhythmic complications. Herein, we report the case of a patient with TCM who developed complete atrioventricular block followed by QT prolongation and torsades de pointes. Furthermore, we undertook a literature review of this rare complication of TCM and discussed the formidable therapeutic challenge encountered in such patients.
Keywords: arrhythmias, pacing and electrophysiology
Background
Takotsubo cardiomyopathy (TCM) is also known as broken heart syndrome or stress-induced non-ischaemic cardiomyopathy that commonly represents transient left ventricular systolic dysfunction with akinesis of the apical wall. It affects about 1.2%–2.2% people in Japan, and almost 1.7%–2.2% myocardial infarctions in western countries can be attributed to TCM.1 More than 90% cases of TCM are reported in postmenopausal women, possibly due to oestrogen-induced glucocorticoid and catecholamine release in response to stress.2–4 Mimicking ST-segment elevation myocardial infarction (STEMI) in clinical presentation and electrocardiographic changes, its course is reversible with good prognosis. TCM can be associated with sinus bradycardia, ventricular tachycardia, atrial fibrillation and ventricular fibrillation.5–9 However, the simultaneous presence of complete heart block and torsades de pointes in a patient with TCM is quite rare.
Case presentation
A 59-year-old female tourist from Japan was brought to the emergency department with altered sensorium and slurred speech, after an episode of dizziness. She did not reportedly experience similar symptoms in the past. The patient was complaining of mild fatigue before her current presentation, which her daughter attributed to travelling. Family history was negative for sudden cardiac death and coronary artery disease. At baseline, she had a very good exercise tolerance. She denied any preceding symptoms of aura, tinnitus or hallucinations however endorsed stress from her recent travel. Medical history was non-significant, and she was not taking any medications at home. This episode of altered sensorium lasted for 30 min, and it resolved while the patient was in the resuscitation room.
The patient was afebrile with an initial blood pressure of 195/117 mm Hg, heart rate of 91 beats per minute and a respiratory rate 20 per min. Rest of the systemic examination was unremarkable; however, the neurological exam was inconclusive. Initial ECG showed normal sinus rhythm with an incomplete right bundle branch block (RBBB) and many premature ventricular complexes (PVCs) with corrected QT (QTc) of 470 ms (figure 1).
Figure 1.
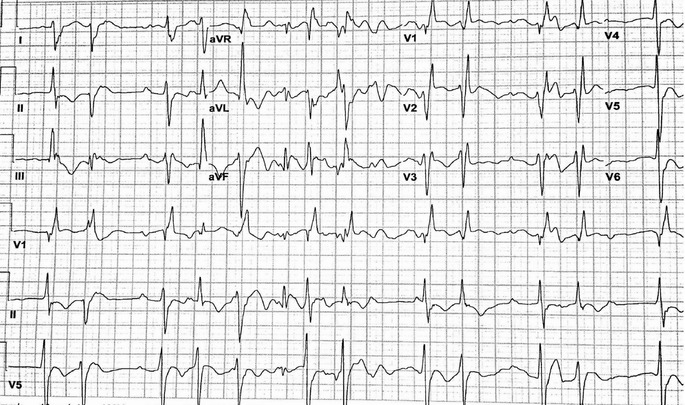
Initial ECG showing normal sinus rhythm with incomplete right bundle branch block and many premature complexes.
She underwent an emergent CT scan and then MRI of the head, which ruled out acute stroke. On her way back to the emergency department, she complained of dizziness. The patient was haemodynamically stable but repeat ECG showed wide ventricular escape with RBBB morphology, bradycardia of 48, multiple PVCs, prolonged QTc of 643 ms, third-degree heart block and deep T-wave inversions (TWIs) in limb leads (figure 2). Physical examination was significant for cannon A waves in right jugular vein. Stroke and cardiology services were consulted. First troponin level was 0.087 ng/mL (normal <0.031 ng/mL), which peaked to 0.349 ng/mL, while other laboratory values were within the normal limits. Bedside transthoracic echocardiography showed basal hyperkinesia and apical hypokinesis with a left ventricle ejection fraction of ~35%–40%. She was transferred to cardiac care unit for further management on continuous telemetry.
Figure 2.
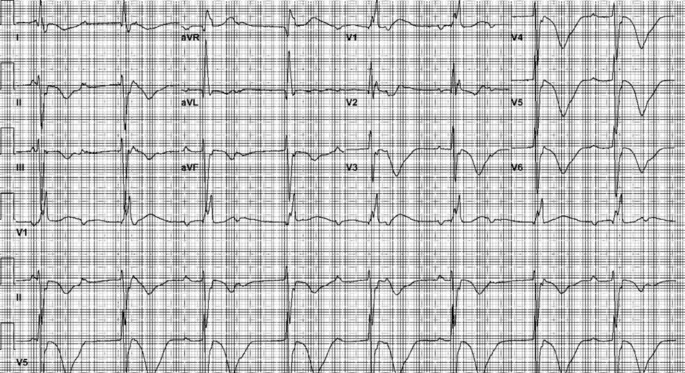
Repeat ECG demonstrating wide ventricular escape with RBBB morphology, bradycardia, multiple PVC, prolonged QTc, third-degree heart block and deep T-wave inversions in limb leads. PVC, premature ventricular complex; RBBB, right bundle branch block.
On day 2, the patient was complaining of worsening dyspnoea, palpitations and dizziness. An immediate telemetry demonstrated that she was having runs of torsades de pointes (figure 3), while her electrolytes were in normal range. She was given 2g of intravenous magnesium. Because of her symptoms, an intravenous isoproterenol infusion was started, and a temporary transvenous pacemaker was placed. Her ECG showed ventricular paced rhythm at a rate of 70 beats per min (figure 4).
Figure 3.
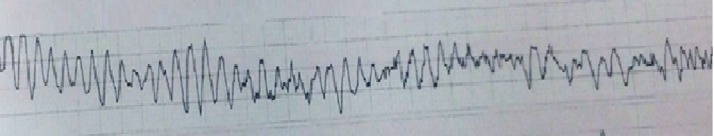
Torsades de pointes on telemetry.
Figure 4.

ECG after a temporary transvenous pacemaker placement demonstrating ventricular paced rhythm with a rate of 70 beats per min.
On day 3, left heart catheterisation was performed to identify narrowing of coronary vessels for the possible ischaemic cause of heart block, which showed no evidence of atherosclerosis in coronaries with apical ballooning on left ventriculogram. These findings were consistent with TCM. She was started on heart failure medications; however, her ECG still showed complete heart block, and repeat echocardiography showed no improvement of her left ventricular function.
Differential diagnosis
On presentation, our suspicion was acute stroke and myocardial infarction; however, negative imaging studies and normal angiography ruled out these possibilities. Sarcoidosis was ruled out based on lack of extracardiac clinical features, an absence of lymphadenopathy on chest X-ray, normal serum levels of calcium, 1, 25-dihydroxyvitamin D level, ACE and serum amyloid A. Cardiac MRI would have been diagnostic, but it was not performed due to its incompatibility following the pacemaker implantation.
Treatment
Eventually, biventricular implantable cardioverter-defibrillator (BiV-ICD) was placed on day 6 without any complications, and postimplantation ECG showed atrial-sensed ventricular paced rhythm (figure 5).
Figure 5.
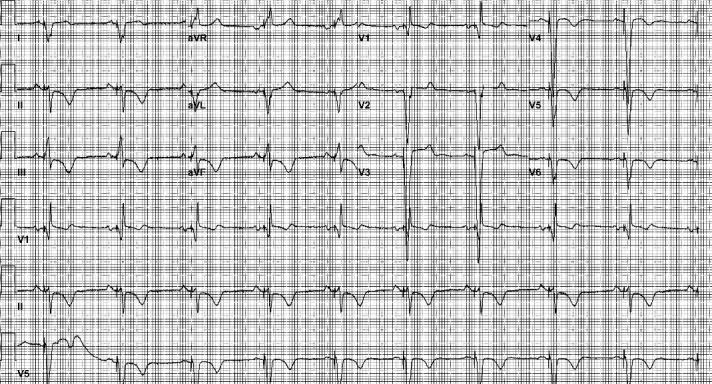
ECG showing atrial-sensed ventricular-paced rhythm after an uneventful implantation of biventricular implantable cardioverter defibrillator.
Outcome and follow-up
BiV-ICD device interrogation showed appropriate parameters, and postimplant chest radiograph showed the appropriate lead position and no pneumothorax. Except for mild local tenderness at the implant site, rest of her hospital course was uneventful. On day 5, the patient was discharged from the hospital on ACE inhibitors, beta-blockers and diuretics and was encouraged regular follow-up with her physician in Japan. On follow-up with her cardiologist after 6 months, she only had one inappropriate shock (no appropriate shocks). Her repeat echocardiography showed EF ~50%, and her baseline rhythm remained complete heart block. Clinically, she was asymptomatic.
Discussion
TCM has gained worldwide recognition since its first description in Japan in 1990.2 However, after over two decades of extensive research towards a better understanding of this disorder, current knowledge remains limited. TCM is characterised by transient left ventricular dysfunction in the absence of significant coronary artery disease on cardiac catheterisation.3 It predominantly affects elderly women and is often preceded by an emotional or physical trigger.3 4 In most cases, TCM mostly presents with acute substernal chest pain, but some patients may present with dyspnoea or syncope. In the acute phase, clinical features, electrocardiographic findings and biomarker profile are often in line with those of an acute coronary syndrome.2–4
Previously, various arrhythmic complications have been associated with TCM. It includes a whole spectrum from benign tachyarrhythmia to acquired long QT syndrome leading to ventricular fibrillation, and in some cases, sudden cardiac death.5 However, QT interval rarely prolongs to the extent to cause torsades de pointes.6 7 In literature, there are several case reports of complete heart block secondary to TCM.6–9 However, a comprehensive literature search of the PubMed database identified only one case of TCM in a 77-year-old postmenopausal woman who also presented with dizziness, and her hospital course was complicated with a complete heart block and torsades de pointes.6 Hence, the present report is only the second of its kind in which an unusual constellation of cardiological findings is reported in a relatively young patient.
Current Mayo Clinic Criteria is the gold standard for the diagnosis of TCM.10 11 It is defined as: (1) transient hypokinesia, akinesia or dyskinesia in the left ventricular midsegments with/without apical involvement; regional wall motion abnormalities that usually extend beyond a single epicardial vascular distribution and frequently, but not always, a physical or emotional trigger; (2) absence of obstructive coronary disease or angiographic evidence of acute plaque rupture; (3) new ECG abnormalities (ST-segment elevations or TWI) or modest elevation in cardiac troponin; and (4) absence of pheochromocytoma and myocarditis. Atypical variants are described in literature including midventricular type (~14.6% cases) and basal type (~2.2% cases). Basal type, also known as reverse type of TCM, primarily affects basal segment of left ventricle, sparing apex and mid ventricle. In our patient, the ECG and transthoracic echocardiogram findings were consistent with above-mentioned criterion for differentiating TCM from an acute myocardial infarction. Early confirmation of the accurate diagnosis holds paramount importance in view of the evidence that in TCM patients, the underlying critical illness is the main driver of the mortality rates.12
Several mechanisms have been proposed to explain the pathogenesis of TCM. Ibañez et al noted a correlation between TCM and aberrant left anterior descending (LAD) artery, in which the LAD artery wraps around the apex of the heart and supplies the inferior wall of the heart along with the apex.13 However, in our case, it does not explain the involvement of the basal part of the heart. It has also been suggested that a midventricular wall thickening with outflow obstruction plays important role in the pathophysiology of TCM.14 Other researchers suggested that simultaneous vasospasm of multiple coronary arteries and microvascular dysfunction as the possible causes of TCM. Recently, it is believed that the coalescence of several factors like coronary vasospasm, an abnormal response to epinephrine and norepinephrine, released in response to stress and dysfunction of the microvasculature leads to TCM.15
In our patient, physical stress of continuous travelling was the probable trigger for TCM. Since her initial ECG showed deep TWIs that usually occur in subacute phase (days 1–3 following acute phase characterised by STEMI like ECG changes), there is equal number of chances that either we might have missed the acute phase or she had silent acute phase in which she was complaining of excessive tiredness. Although normal coronary angiography ruled out the possibility of acute coronary syndrome, we could not exclude the hypothesis of microvascular dysfunction. The possible mechanism of atrioventricular heart block and torsades de pointes in the setting of TCM can be explained by the continual ischaemic status due to the microvascular dysfunction leading to atrioventricular conduction disorder. This conduction disorder was expected to improve rapidly; however, due to the worsening condition of the patient, pacemaker placement became necessary.
Generally, it is very uncommon for a patient to present with conduction abnormality as the first presentation of sarcoidosis or any infiltrative disorder, but it has happened in rare cases in relatively young patients.16 The patient in present report was 59 years old, on the borderline between the young and the old age groups. Also when she presented in emergency department, her initial ECG showed normal sinus rhythm and few PVCs, so we assumed safely that the trigger for conduction abnormality was not ongoing infiltrative or infectious but most likely TCM. Therefore, TCM should be considered while excluding other causes of complete heart block in a young patient.
TCM is a reversible cause of severe systolic dysfunction with much better prognosis as compared to other cardiomyopathies.17 The literature on evidence-based data regarding drug therapy to treat or prevent arrhythmias in patients with TCM is scarce.18 Generally, antiarrhythmic drugs should be employed cautiously in such patients. It is important to avoid QT interval-prolonging drugs in view of the high prevalence of QT interval prolongation in the acute and subacute phases of TCM.19 β-Blockers are used frequently in patients with TCM on the basis of the assumption of enhanced sympathetic activity. Nevertheless, the risk of conduction disorders resulting in relevant bradyarrhythmias as well as bradycardia-induced ventricular tachyarrhythmias should always be considered.
The time course of improvement in left ventricular systolic function is unpredictable and does not necessarily correlate with the resolution of the block in the conduction system.5–9 17 Previously, the TCM cases with complete heart block underwent the permanent pacemaker implantation because of the lack of the conduction improvement.20 21 In rare instances, the atrioventricular (AV) conduction disorder was transient and recovered in a time period ranging from 2 days to 2 years.21–23 To the best of our knowledge, there were only three TCM cases reported so far in the published literature with the transient AV conduction disorder.
Although it is very challenging to decide the appropriate time to implant a pacemaker, electrophysiology service advocated for placing BiV-ICD in the present case. Indications for BiV-ICD were QRS duration of >150 ms (190 ms in our case), non-left bundle branch block pattern, ejection fraction (EF) <35% with non-sustained ventricular tachycardia despite pacing. Also, the time course of improvement in left ventricular systolic function is unpredictable and does not necessarily correlate with resolution of conduction system defects.20–24 In contrast, polymorphic ventricular arrhythmias might be managed with a temporary approach (eg, wearable cardioverter-defibrillators) until recovery of repolarisation time and left ventricular function.25 26 However, population-based clinical studies are warranted to broaden the scope of our knowledge on this association and to frame guidelines to standardise the care of TCM patients with complete heart block and torsades de pointes.
Learning points.
A rare association of Takotsubo cardiomyopathy (TCM) with third-degree heart block and torsades de pointes due to prolonged QT interval has been reported.
The management of TCM associated with the high-degree atrioventricular block is still unclear and challenging. Critical decision making holds a pivotal role in saving the lives of patients with such severe arrhythmic complications.
More cases need to be reported to better understand the pathophysiology, which will eventually lead to a remarkable improvement in the clinical management in patients with TCM-related heart block.
Footnotes
Contributors: FI and WU did the literature review and wrote the discussion; IR and HUHV wrote the background and case presentation.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Gianni M, Dentali F, Grandi AM, et al. Apical ballooning syndrome or takotsubo cardiomyopathy: a systematic review. Eur Heart J 2006;27:1523–9. 10.1093/eurheartj/ehl032 [DOI] [PubMed] [Google Scholar]
- 2.Sato H. Tako-tsubo-like left ventricular dysfunction due to multivessel coronary spasm Clinical aspect of myocardial injury: from ischemia to heart failure 1990:56–64. [Google Scholar]
- 3.Templin C, Ghadri JR, Diekmann J, et al. Clinical features and outcomes of takotsubo (stress) cardiomyopathy. N Engl J Med 2015;373:929–38. 10.1056/NEJMoa1406761 [DOI] [PubMed] [Google Scholar]
- 4.Virk HU, Inayat F. Clostridium difficile infection and Takotsubo cardiomyopathy: is there a relation? N Am J Med Sci 2016;8:316–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Migliore F, Zorzi A, Marra MP, et al. Myocardial edema underlies dynamic T-wave inversion (Wellens' ECG pattern) in patients with reversible left ventricular dysfunction. Heart Rhythm 2011;8:1629–34. 10.1016/j.hrthm.2011.04.035 [DOI] [PubMed] [Google Scholar]
- 6.Oshima T, Ikutomi M, Ishiwata J, et al. Takotsubo cardiomyopathy associated with complete atrioventricular block and Torsades de pointes. Int J Cardiol 2015;181:357–9. 10.1016/j.ijcard.2014.12.076 [DOI] [PubMed] [Google Scholar]
- 7.Sacha J, Wester A, Hordynski G, et al. QT interval prolongation during ECG evolution in takotsubo cardiomyopathy poses a threat of torsade de pointes to predisposed patients. Case report of a female patient with congenital AV block. Herz 2013;38:790–5. 10.1007/s00059-013-3756-8 [DOI] [PubMed] [Google Scholar]
- 8.Inoue M, Kanaya H, Matsubara T, et al. Complete atrioventricular block associated with takotsubo cardiomyopathy. Circ J 2009;73:589–92. 10.1253/circj.CJ-08-0219 [DOI] [PubMed] [Google Scholar]
- 9.Kodama S, Miyoshi K, Shiga Y, et al. Takotsubo cardiomyopathy complicated by high-grade atrioventricular block: a report of two cases. Exp Clin Cardiol 2009;14:e35–8. [PMC free article] [PubMed] [Google Scholar]
- 10.Sharkey SW, Lesser JR, Maron MS, et al. Why not just call it tako-tsubo cardiomyopathy: a discussion of nomenclature. J Am Coll Cardiol 2011;57:1496–7. 10.1016/j.jacc.2010.11.029 [DOI] [PubMed] [Google Scholar]
- 11.Prasad A, Lerman A, Rihal CS. Apical ballooning syndrome (Tako-Tsubo or stress cardiomyopathy): a mimic of acute myocardial infarction. Am Heart J 2008;155:408–17. 10.1016/j.ahj.2007.11.008 [DOI] [PubMed] [Google Scholar]
- 12.Brinjikji W, El-Sayed AM, Salka S. In-hospital mortality among patients with takotsubo cardiomyopathy: a study of the National Inpatient Sample 2008 to 2009. Am Heart J 2012;164:215–21. 10.1016/j.ahj.2012.04.010 [DOI] [PubMed] [Google Scholar]
- 13.Ibáñez B, Navarro F, Farré J, et al. [Tako-tsubo syndrome associated with a long course of the left anterior descending coronary artery along the apical diaphragmatic surface of the left ventricle]. Rev Esp Cardiol 2004;57:209–16. [DOI] [PubMed] [Google Scholar]
- 14.Merli E, Sutcliffe S, Gori M, et al. Tako-Tsubo cardiomyopathy: new insights into the possible underlying pathophysiology. Eur J Echocardiogr 2006;7:53–61. 10.1016/j.euje.2005.08.003 [DOI] [PubMed] [Google Scholar]
- 15.Wittstein IS, Thiemann DR, Lima JA, et al. Neurohumoral features of myocardial stunning due to sudden emotional stress. N Engl J Med 2005;352:539–48. 10.1056/NEJMoa043046 [DOI] [PubMed] [Google Scholar]
- 16.Patel B, Shah M, Gelaye A, et al. A complete heart block in a young male: a case report and review of literature of cardiac sarcoidosis. Heart Fail Rev 2017;22:55–64. 10.1007/s10741-016-9585-0 [DOI] [PubMed] [Google Scholar]
- 17.Benouda L, Roule V, Foucault A, et al. Conduction disturbances in takotsubo cardiomyopathy: a cause or a consequence? Int J Cardiol 2012;159:61–2. 10.1016/j.ijcard.2012.03.164 [DOI] [PubMed] [Google Scholar]
- 18.Santoro F, Ieva R, Musaico F, et al. Lack of efficacy of drug therapy in preventing takotsubo cardiomyopathy recurrence: a meta-analysis. Clin Cardiol 2014;37:434–9. 10.1002/clc.22280 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Abe Y, Kondo M, Matsuoka R, et al. Assessment of clinical features in transient left ventricular apical ballooning J am Coll Cardiol. (2003;41:737–42. [DOI] [PubMed] [Google Scholar]
- 20.Kodama S, Miyoshi K, Shiga Y, et al. Takotsubo cardiomyopathy complicated by high-grade atrioventricular block: a report of two cases. Exp Clin Cardiol 2009;14:e35–8. [PMC free article] [PubMed] [Google Scholar]
- 21.Benouda L, Roule V, Foucault A, et al. Conduction disturbances in takotsubo cardiomyopathy: a cause or a consequence? Int J Cardiol 2012;159:61–2. 10.1016/j.ijcard.2012.03.164 [DOI] [PubMed] [Google Scholar]
- 22.Lee WL, Miao LF, Chan HW, et al. Takotsubo syndrome with transient complete atrioventricular block. Chin Med J 2006;119:73–6. [PubMed] [Google Scholar]
- 23.Nef HM, Möllmann H, Sperzel J, et al. Temporary third-degree atrioventricular block in a case of apical ballooning syndrome. Int J Cardiol 2006;113:E33–5. 10.1016/j.ijcard.2006.04.007 [DOI] [PubMed] [Google Scholar]
- 24.Nault MA, Baranchuk A, Simpson CS, et al. Takotsubo cardiomyopathy: a novel ‘proarrhythmic’ disease. Anadolu Kardiyol Derg 2007;7(Suppl 1):101–3. [PubMed] [Google Scholar]
- 25.Migliore F, Zorzi A, Peruzza F, et al. Incidence and management of life-threatening arrhythmias in Takotsubo syndrome. Int J Cardiol 2013;166:261–3. 10.1016/j.ijcard.2012.09.107 [DOI] [PubMed] [Google Scholar]
- 26.Stiermaier T, Rommel KP, Eitel C, et al. Management of arrhythmias in patients with Takotsubo cardiomyopathy: Is the implantation of permanent devices necessary? Heart Rhythm 2016;13:1979–86. 10.1016/j.hrthm.2016.06.013 [DOI] [PubMed] [Google Scholar]


