Abstract
Background and objectives
Arterial stiffness plays a significant role in the development and progression of adverse cardiovascular events and all-cause mortality. This observational study aims to explore the relationship between six acute phase proteins namely, ceruloplasmin, alpha-1-antitrypsin, orosomucoid, haptoglobin, complement C3 and C-reactive protein (CRP), and carotid-femoral pulse wave velocity (c-f PWV) in a population-based cohort, and to also explore the effect of low-grade inflammation on the relationship between diabetes and c-f PWV.
Method
The study consisted of participants from the Malmö Diet and Cancer study with data from baseline examinations (1991–1994) and follow-up examinations (2007–2012). Arterial stiffness was measured at follow-up by determining c-f PWV. After excluding participants with missing data, the total study population included 2338 subjects. General linear models were used to assess the relationship between baseline acute phase proteins and c-f PWV.
Results
After adjusting for traditional risk factors the participants in the 4th quartile vs 1st quartile of alpha-1-antitrypsin (geometric mean: 10.32 m/s vs 10.04 m/s) (p<0.05), C3 (10.35 m/s vs 10.06 m/s) (p<0.05) and CRP (10.37 m/s vs 9.96 m/s) (p<0.001) showed significant association with c-f PWV. Diabetes at follow-up was also associated with high c-f PWV, however, this relationship was independent of low grade inflammation.
Conclusion
Alpha-1-antitrypsin, C3 and CRP are associated with arterial stiffness. The results indicate that low grade inflammation is associated with arterial stiffness in addition to established cardiovascular risk factors.
Introduction
Arterial stiffness is an important risk determinant for adverse cardiovascular events and all-cause mortality [1, 2]. Various studies have shown aortic stiffness to be an independent predictor for all-cause mortality and morbidity in subjects with hypertension, end stage renal disease, type 2 diabetes and the elderly [3–6]. Pulse wave velocity (PWV) has been widely accepted as gold standard for measurement of arterial stiffness [7]. A higher PWV specifies a stiffer aorta, resulting in increased afterload and the subsequent cardiac remodeling and failure [8–10]. Carotid femoral PWV (c-f PWV) measures along the aortic and aorto-iliac pathway and is representative of arterial stiffness [7].
There are multiple risk factors that affect arterial stiffness. Age and blood pressure have been shown to be associated with arterial stiffness [11, 12]. Additionally, many other environmental and genetic factors including dyslipidemia, diabetes [13], elevated heart rate [14], obesity [15] and smoking [16] are often associated with increased arterial stiffness.
There is evidence supporting the fact that inflammation is associated with adverse cardiovascular events, as shown by previous studies [17–19]. It has been demonstrated that acute phase proteins are associated with incidence of myocardial infarction [17], future development of hypertension [18, 19] and incidence of diabetes [20]. Systemic inflammation has also been associated with arterial stiffness [19]. Many studies have explored the association between arterial stiffness and inflammation in subjects with chronic inflammatory conditions such as rheumatoid arthritis [21], systemic lupus erythematosus [22], inflammatory bowel disease [23] and systemic sclerosis [24]. C-reactive protein (CRP) has been shown to be associated with arterial stiffness in an apparently healthy cohort [25] and in subjects with end stage renal disease (ESRD) [26].
A recent cross-sectional study from the Malmö Diet and Cancer study (MDC) reported that waist circumference, raised fasting glucose, insulin resistance and diabetes, and dyslipidemia were associated with increased c-f PWV [27]. Whether the relationship between diabetes and c-f PWV could be modified by low-grade inflammation is unclear. Because of the emerging importance of arterial stiffness in predicting cardiovascular disease risk, a better understanding of the role of inflammatory biomarkers as additional predictors is warranted.
The aim of this observational study is to investigate the association between six acute phase proteins namely, ceruloplasmin, alpha-1-antitrypsin, orosomucoid, haptoglobin, complement C3 and CRP on the one hand and c-f PWV on the other hand in a population-based cohort, followed up for 17 years. Another aim was to study whether the relationship between diabetes and c-f PWV is modified by low-grade inflammation.
Materials and methods
Study population
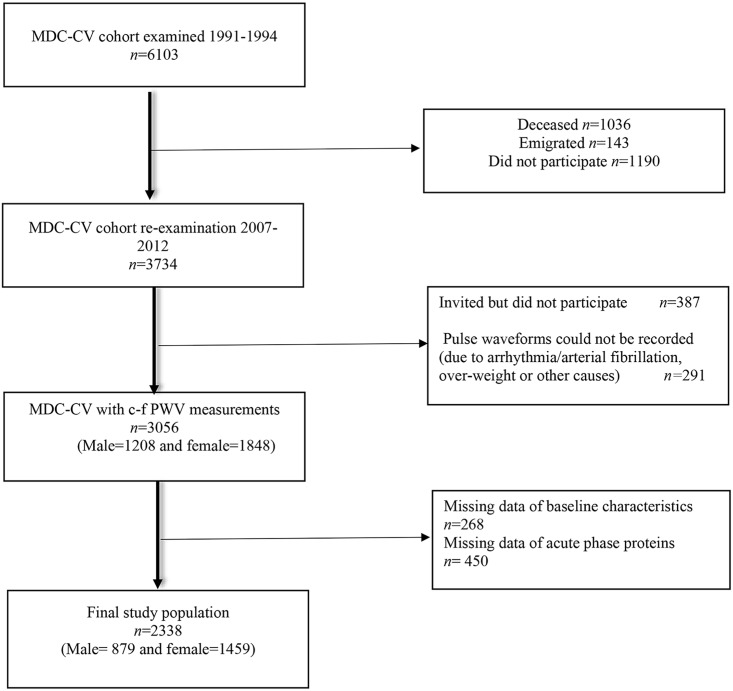
The Malmö Diet and Cancer (MDC) study is a large prospective cohort, compromising of men and women from the city of Malmö, Sweden [28]. A random sample of participants from this cohort was invited between November 1991 and February 1994 to investigate the epidemiology of carotid artery abnormalities, constituting the cardiovascular sub-cohort (n = 6103, 2572 men and 3531 women) [29]. A re-examination of participants from the sub-cohort, who were alive and had not emigrated, was carried out between May 2007 and January 2012. Follow-up data from 3734 participants who attended the re-examination was obtained (76% participation rate). The characteristics of non-attendees of the re-examination have been described elsewhere [30]. Measurements of c-f PWV were available for 3056 participants (Fig 1). Individuals with missing values for baseline characteristics (n = 268), and lacking lab data for one or more acute phase proteins (n = 450) were excluded from the study. The resulting final study population consisted of 2338 participants (879 men and 1459 women). The study population flow chart is illustrated in Fig 1.
Fig 1. Flow chart of study population (n = 2338).
The study conforms to the ethical guidelines of the 1975 Declaration of Helsinki. It was approved by the Lund University Ethical Committee (LU 51–90 and LU 532–2006). All the participants provided written informed consent.
Baseline examinations
Data from baseline examination was collected by means of a self-administered questionnaire, physical examination and collection of blood samples [28]. Information about medical history, smoking habits, use of anti-hypertensive, anti-lipid medication, use of anti-inflammatory medications such as aspirin and steroids was obtained from the questionnaire. Smokers were classified into two categories: non-smokers (i.e., former smokers and never smokers) and current smokers. Blood pressure (mmHg) was measured once, after ten minutes of rest while the subject was in supine position using a mercury-column sphygmomanometer. Waist circumference (in cm) measurements were taken midway between the lowest rib margin and iliac crest. Blood samples were collected after an overnight fast [30]. High-density lipoprotein (HDL) was measured according to standard procedures at laboratory of the University Hospital. Low-density lipoprotein cholesterol (LDL) concentration was calculated according to Friedewald’s formula [31].
Diabetes was defined based on a self-reported physician’s diagnosis of diabetes, use of anti-diabetic medication, or fasting whole blood glucose ≥ 6.1 mmol/L (corresponding to a plasma glucose of 7.0 mmol/L) [32]. Information regarding individuals with rheumatic disease was obtained through a questionnaire. Participants with prevalent cardiovascular disease at baseline were determined according to the questionnaire and hospital registers.
The plasma levels of ceruloplasmin, orosomucoid, haptoglobin, alpha-1-antitrypsin and C3 were analyzed using Cobas c-systems (Roche Diagnostics GmbH, Germany) and have been explained elsewhere [20]. High-sensitive CRP in plasma was analyzed using the Tina-quant® CRP latex assay (Roche Diagnostics, Basel, Switzerland) on an ADVIA®1650 Chemistry System (Bayer Healthcare, NY, USA).
Follow-up examinations
The follow-up examinations were carried out between 2007 and 2012 and comprised of a self-administered questionnaire, blood samples collection and physical examinations. Blood pressure was measured after 5 min rest in supine position using the OMRON M5-1 IntelliSense device. Fasting blood samples were collected for measurement of plasma glucose (p-glucose) using HemoCue (HemoCue AB, Ängelholm, Sweden). Oral glucose tolerance test (OGTT) was conducted following an overnight fast after intake of 75 g of glucose and plasma glucose measurements were done before intake and after 120 min. Fasting plasma glucose of at least 7.0 mmol/L or 2 hour glucose of at least 11.0 mmol/L, verified subsequently by a fasting plasma glucose, was diagnosed as diabetes.
Diabetic cases at follow-up were defined on the basis of six different national and regional diabetes registers. These have been described in detail elsewhere [33]. Additionally, new onset diabetes verified though fasting plasma glucose or OGTT at the rescreening were also included if the date of onset was before the date of measurement of c-f PWV.
Carotid-femoral pulse wave velocity measurement
The measurements for the c-f PWV were carried out on average 261 days after the first visit in the follow-up examination. They were conducted by using applanation tonometry (SphygmoCor, Atcor Medical, Australia) following a specific study protocol. The measurements were done with the patients in supine position after 5 minutes resting. Pulse curves from the carotid and femoral arteries were obtained with a pressure sensitive probe. For the purpose of calculation, the distance was measured from the suprasternal notch to the umbilicus and the umbilicus to the measuring point at the femoral artery subtracting the suprasternal notch to the measuring point at the carotid artery. ECG was registered simultaneously and the time from the peak of the R-wave on ECG to the foot of the pulse wave at the carotid and femoral arteries was automatically calculated. Each participant had varying number of successful measurements, ranging between one and five. The aim was to obtain three measurements each, which was possible in 86.7% of the cases. Mean c-f PWV was determined from these measurements [27]. Heart rate was described as average heart rate (beats/min) at registration of carotid artery. Blood pressure measurements were also performed just before measuring the c-f PWV using the OMRON M5-1 IntelliSense device. Mean arterial pressure (MAP) was determined by the formula (2 × diastolic pressure + systolic pressure)/3.
Inter-observer variability was determined twice by two technicians in 17 and 13 participants, respectively. Inter-observer difference was 5.0% (± SD4.0) and 7.2% (±SD9.9), respectively.
Statistical analysis
All statistical analyses were performed using IBM SPSS Statistics version 22 (IBM Corp., Armonk, New York, USA). Variables such as c-f PWV, ceruloplasmin, C3 and CRP were natural log (ln) transformed due to their skewed distribution. Sex-specific quartiles of the acute phase proteins were created, i.e., four quartiles with the same proportion of men and women in each quartile. The baseline and follow-up characteristics of the study population were presented as means ± standard deviation (SD), median (25th -75th percentiles) or percentages. The 2007 European Society of Hypertension-European society of Cardiology (ESH-ESC) guidelines for the management of hypertension proposed a cut off value of c-f PWV of 12 m/s [34]. This value was suggested as a threshold for sub-clinical organ damage. The present study population was categorized into three groups according to their c-f PWV; those with c-f PWV ≥ 12m/s, with c-f PWV <12 and ≥ 8m/s and those with c-f PWV < 8m/s. Comparison between these groups was done for the baseline and follow-up characteristics. To test the differences between these groups, analysis of covariance (ANCOVA) and logistic regression were used for continuous and categorical variables respectively, adjusting for age, sex, heart rate and MAP at follow-up.
Univariate General linear models were used, with c-f PWV as the dependent variable, to assess the association between c-f PWV and quartiles of acute phase proteins. For Model 1, the analysis was adjusted for age, sex, heart rate and MAP at follow-up examination. For Model 2, further adjustments were done for baseline age, smoking habits, systolic blood pressure, HDL, LDL, waist circumference, presence of diabetes, use of anti-hypertensive medication and use of lipid lowering medication. Interaction terms were introduced to assess any interaction between sex and the acute phase proteins. Univariate general linear model was also used to evaluate the effect of inflammation on the relationship between diabetes at follow-up and c-f PWV by adjusting for the six acute phase proteins and other covariates i.e age, sex, heart rate and MAP at follow-up examination and baseline age, smoking habits, systolic blood pressure, HDL, LDL, waist circumference, use of anti-hypertensive medication and use of lipid lowering medication. For the purpose of these analyses, ln transformed values were used and were transformed back to geometric means to facilitate interpretation of results. A p-value of less than 0.05 was regarded as statistically significant.
Results
Baseline and follow-up characteristics
The mean follow-up period from the baseline examinations to the c-f PWV measurements was 16.9 ± 1.5 years. The mean age of the study population was 56.0±5.7 and 72.1±5.6 years at the baseline and follow-up examinations, respectively.
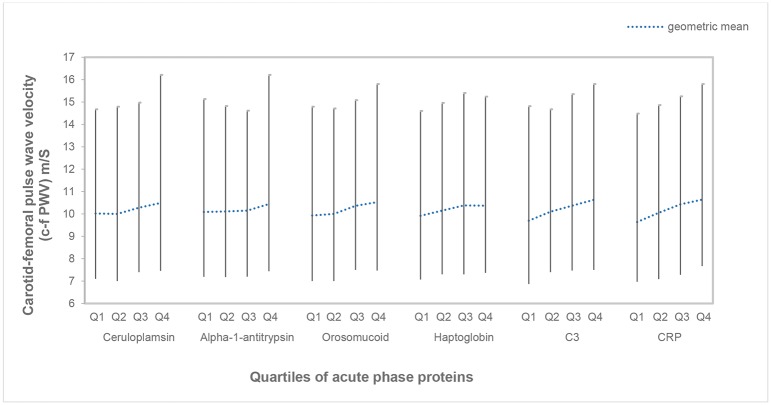
The characteristics of the study population have been presented in Table 1. The table also displays the comparisons of characteristics between participants with high, intermediate and low arterial stiffness. Those with high arterial stiffness exhibited higher cardiovascular risk, except for smoking, than those with low arterial stiffness. Plasma levels of all the acute phase proteins were higher in those with high arterial stiffness. The geometric means with 5th to 95th percentile of c-f PWV in the different quartiles of the acute phase proteins are presented in Fig 2.
Table 1. Follow-up and baseline characteristics of the whole study population (n = 2338) and comparisons of characteristics of participants with high, intermediate and low arterial stiffness.
| Whole study population (n = 2338) | High arterial stiffness (n = 515) | Intermediate arterial stiffness (n = 1525) | Low arterial stiffness (n = 298) | p value** | |
|---|---|---|---|---|---|
| Follow-up | |||||
| c-f PWV* (m/s) | 10.03[8.80–11.73] | 13.53[12.67–14.83] | 9.8[8.97–10.70] | 7.4[6.97–7.77] | |
| Age (years) | 72.08(±5.56) | 75.25(±5.10) | 71.68(±5.36) | 68.70(±4.53) | |
| Heart rate (beats/min) | 62.76(±9.91) | 65.27(±10.04) | 62.64(±9.96) | 59.04(±8.01) | |
| Mean arterial pressure (mmHg) | 95.56(±10.49) | 100.02(±10.62) | 95.44(±9.95) | 88.50(±8.89) | |
| Baseline | |||||
| Age (years) | 55.97(±5.65) | 59.21(±5.27) | 55.56(±5.44) | 52.50(±4.53) | 0.112 |
| Smoking {current smokers [n (%)]} | 398(17) | 63(12.2) | 273(17.9) | 62(20.8) | 0.230 |
| Systolic blood pressure (mmHg) | 137.58(±17.64) | 145.48(±17.67) | 136.33(±16.89) | 130.28(±16.55) | <0.001 |
| Waist (cm) | 81.25(±11.60) | 84.99(±12.29) | 80.55(±11.31) | 78.41(±10.32) | <0.001 |
| HDL cholesterol(mmol/L) | 1.43(±0.37) | 1.38(±0.38) | 1.44(±0.36) | 1.46(±0.35) | 0.002 |
| LDL cholesterol (mmol/L) | 4.09(±0.96) | 4.30(±0.99) | 4.05(±0.94) | 3.91(±0.95) | 0.015 |
| Diabetes [n (%)] | 121(5.2) | 60(11.7) | 55(3.6) | 6(2) | <0.001 |
| Lipid lowering drug medication [n (%)] | 43(1.8) | 17(3.3) | 20(1.3) | 6(2) | 0.234 |
| Anti- hypertensive medication [n (%)] | 272(11.6) | 95(18.4) | 158(10.4) | 19(6.4) | <0.001 |
| Ceruloplasmin* (g/L) | 0.49[0.43–0.56] | 0.50[0.43–0.57] | 0.48[0.43–0.56] | 0.48[0.42–0.55] | 0.009 |
| Alpha-1-antitrypsin(g/L) | 1.18(±0.25) | 1.18(0.25) | 1.18(0.24) | 1.16(0.27) | 0.321 |
| Orosomucoid(g/L) | 0.68(±0.20) | 0.71(0.20) | 0.67(0.19) | 0.64(0.19) | <0.001 |
| Haptoglobin(g/L) | 1.25(±0.51) | 1.31(0.51) | 1.23(0.50) | 1.20(0.52) | 0.025 |
| Complement C3*(g/L) | 1.45[1.28–1.64] | 1.54[1.35–1.72] | 1.43[1.28–1.62] | 1.37[1.19–1.58] | <0.001 |
| CRP* (mg/L) | 1.10 [0.60–2.30] | 1.50[0.70–2.80] | 1.10[0.60–2.20] | 0.80[0.50–1.60] | <0.001 |
Values are expressed as means (±SD) or percentages unless specified elsewise. High arterial stiffness: c-f PWV ≥12 m/s; intermediate arterial stiffness: ≥8 m/s and <12m/s; Low arterial stiffness: c-f PWV <8 m/s
*median [25th–75th percentile].
** p—values for differences between groups with high, intermediate and low arterial stiffness after adjustment for age, sex heart rate and mean arterial pressure (MAP).
Fig 2. Geometric means and 5th to 95th percentiles of c-f PWV in different quartiles of acute phase proteins.
Relationship between acute phase proteins and c-f PWV
When the different quartiles of the acute phase proteins were compared, the association between all the acute phase proteins and c-f PWV were significant for the participants in the 4th quartile vs the 1st quartile in Model 1 as shown in Table 2. After further adjustments in Model 2, the c-f PWV remained significantly higher for participants in the 4th quartile vs 1st quartile of alpha-1-antitrypsin (geometric mean: 10.32 m/s vs 10.04 m/s) (p<0.05), C3 (10.35 m/s vs 10.06 m/s) (p<0.05) and CRP (10.37 m/s vs 9.96 m/s) (p<0.001). The p-values for trend across quartiles of acute phase proteins are shown in Table 2. The interaction terms between sex and the acute phase proteins were not significant.
Table 2. Relationships between the acute-phase proteins and c-f PWV.
| Model 1 | |||||
| Geometric means (n) | Geometric means (n) | Geometric means (n) | Geometric means (n) | ||
| Q1 | Q2 | Q3 | Q4 | p for trend | |
| Ceruloplasmin | 10.13 (558) | 10.04 (606) | 10.22 (597) | 10.40* (577) | 0.004 |
| Alpha-1-antitrypsin | 10.05 (595) | 10.12 (505) | 10.26 (673) | 10.34** (565) | 0.004 |
| Orosomucoid | 10.05 (645) | 10.00 (531) | 10.21 (577) | 10.52*** (585) | <0.001 |
| Haptoglobin | 10.04 (633) | 10.20 (562) | 10.21 (559) | 10.35** (584) | 0.006 |
| Complement-C3 | 9.89 (577) | 10.08 (595) | 10.27*** (586) | 10.55*** (580) | <0.001 |
| CRP | 9.84 (534) | 10.04 (610) | 10.36*** (607) | 10.52*** (587) | <0.001 |
| Model 2 | |||||
| Q1 | Q2 | Q3 | Q4 | p for trend | |
| Ceruloplasmin | 10.18 | 10.05 | 10.21 | 10.36 | 0.035 |
| Alpha-1-antitrypsin | 10.04 | 10.16 | 10.27* | 10.32* | 0.007 |
| Orosomucoid | 10.20 | 10.03 | 10.18 | 10.37 | 0.058 |
| Haptoglobin | 10.12 | 10.26 | 10.17 | 10.25 | 0.440 |
| Complement-C3 | 10.06 | 10.14 | 10.24 | 10.35* | 0.012 |
| CRP | 9.96 | 10.10 | 10.33** | 10.37*** | <0.001 |
* p<0.05
** p<0.01
***p<0.001
Ln transformed values were used to calculate the p-values with Q1 as the reference group. Model 1: Adjusted for age, sex, heart rate, mean arterial pressure (MAP) at follow-up. Model 2: Adjusted for age, sex, heart rate, mean arterial pressure (MAP) at follow-up, and baseline age, smoking habits, systolic blood pressure, HDL, LDL, waist circumference, diabetes, use of anti-hypertensive medication and use of lipid lowering medication
C-f PWV was also compared in individuals with and without diabetes at the follow-up examination. At the re-examination, 305 individuals had diabetes and 2033 were non-diabetic. As expected, diabetes was significantly associated with c-f PWV (geometric means: 11.16 m/s vs 10.06 m/s) (p<0.001). After adjusting for the acute phase proteins and other covariates the c-f PWV remained significantly higher for individuals with diabetes vs those without diabetes (geometric means: 10.61 m/s vs 10.14 m/s) (p<0.001).
As arterial stiffening increases in individuals with rheumatic and cardiovascular disease, a sensitivity analysis was performed after excluding those with prevalent rheumatic and cardiovascular disease at re-examination. A total of 48 individuals had rheumatic disease (according to questionnaire) and 27 had prevalent cardiovascular disease (according to questionnaire and hospital registers) at baseline. At re-examination, the number of participants with rheumatic and cardiovascular disease was 88 and 171 respectively.
Regarding anti-inflammatory medication, 0.3% (n = 7) and 3.5% (n = 82) of the subjects were taking steroids and aspirin respectively at baseline. These were also excluded for the purpose of the sensitivity analysis. The results showed that the association was still significant between alpha-1-antitrypsin, C3, CRP and arterial stiffness.
Discussion
The results from this large, observational, population-based study show that acute phase proteins alpha-1-antitrypsin, C3 and CRP are associated with future c-f PWV, even after controlling for traditional cardiovascular risk factors. This suggests that low grade inflammation may play a role in the pathogenesis of arterial stiffening, hence contributing to increased cardiovascular risk. Since inflammation is associated with increased incidence of diabetes, we also hypothesized that inflammation could modify the relationship between diabetes and arterial stiffness. We could confirm that diabetes at follow-up was strongly associated with c-f PWV, however, this relationship was independent of baseline low-grade inflammation in this study.
The mechanism as to how these inflammatory biomarkers modify arterial stiffness is unclear. Numerous studies have looked at the link between inflammation and arterial stiffness, but these have consisted mostly of study populations with chronic inflammatory diseases [21–24]. It should be noted that inflammatory markers are associated with other traditional risk factors of arterial stiffness such as obesity and diabetes [13, 15]. However, as adjustment for these risk markers was done in the analyses, it can be postulated that inflammation effects arterial stiffness through a mechanism besides the one linked to these established risk markers. It is interesting to note that one study comprising of another chronic condition associated with systemic inflammation, namely chronic obstructive pulmonary disease (COPD), demonstrated that arterial stiffness in COPD was not related to systemic inflammation [35]. This is in contrast to the above mentioned studies. Although this is interesting, low grade inflammation could still have a role in arterial stiffness. One explanation could be that levels of inflammatory markers are more variable in patients with COPD than in healthy volunteers.
Alpha-1-antitrypsin is a proteinase inhibitor with the primary function of inhibiting proteolytic enzymes like neutrophil elastase. Hence, it plays a role in maintaining the vascular structure. Our results show that there is association between alpha-1-antitrypsin and arterial stiffness after adjustment for the traditional risk factors. This is an interesting finding as previous studies have assessed the relationship between alpha-1-antitrypsin and various cardiovascular diseases with conflicting results [36, 37]. Most of these findings are, however, related to associations with decreased levels of alpha-1-antitrypsin. Ducker et al. demonstrated that a group of patients with alpha-1–antitrypsin deficiency and related chronic obstructive pulmonary disease had increased aortic stiffness [36]. Looking at the different alleles for the of the alpha-1 antitrypsin (SERPINA1) gene, a study undertaken by Dahl et al. concluded that alpha-1-antitrypsin deficiency in ZZ and MZ genotypes is associated with reduced blood pressure in individuals with ischemic heart disease (IHD) as compared to MM/MS genotypes. Additionally, MZ heterozygosity was associated with reduced risk of ischemic cerebrovascular and IHD [37]. One plausible explanation could be that raised alpha-1-antitrypsin levels reflect a compensatory mechanism which reduces the adverse effects of an ongoing proteolytic activity and degradation of elastin. As loss of elastin is central to the stiffening process [38], the proteolytic activity could cause decreased elasticity of the vessel wall and hence, leading to increased arterial stiffness.
It has also been observed in the present study that C3 is associated with c-f PWV. To our knowledge only one previous study has looked at the association between C3 and c-f PWV. The study included middle aged women with Systemic Lupus Erythematosus (SLE) and demonstrated positive association between C3 and CRP on the one hand with aortic stiffness on the other [39]. This is in accordance with our results. C3 has been known to play a role in cardiovascular disease development and hypertension [40, 41]. However, the association between C3 and arterial stiffness has not been widely explored. Shields at al. proposed a mechanism to explain the association between C3 and arterial stiffness [42]. Their study suggested that complement factors C3 and C4, in the absence of plaque formation, target the adventitia and bind to the elastin and collagen fibers in the vascular wall, hence contributing to the progression of arterial stiffness.
The results from the present study show that CRP levels and c-f PWV are associated. These findings are supported by studies that have shown association of CRP with arterial stiffness in apparently healthy individuals [25, 43]. Still further yet, in the Rotterdam study, Mattace et al. demonstrated that there is an association between CRP and arterial stiffness in older adults [44]. Results from cross-sectional studies have been varying, but two large prospective studies have shown the association of inflammation and aortic stiffness. The Whitehall II study and the Caerphilly prospective study showed that there is association between CRP and aortic stiffness [45, 46]. In contrast, a study by Amar et al. showed that although CRP and peripheral pulse pressure were associated, this was not seen with aortic stiffness [47]. It has been proposed that CRP can impact on vascular stiffness by means of its role in endothelial dysfunction and thereby lead to disruption of structural regulation of arteries and consequently arterial stiffness [48]. However, Schumacher et al. explored the association between circulating CRP levels, the CRP genotype and PWV. Interestingly, the study concluded that although there exists an association between circulating levels of CRP and c-f PWV, there is no causal relationship between CRP and arterial stiffness [49].
There is substantial evidence suggesting association between diabetes and arterial stiffness [13, 50, 51]. Arterial stiffness has also been shown to increase during the pre-diabetes stage [52]. Inflammation is commonly linked to both diabetes and arterial stiffness. It has recently been demonstrated in the present cohort that high levels of acute phase proteins are associated with the development of diabetes [20]. The results of the present study showed that those with diabetes had higher c-f PWV regardless the presence of inflammation. This implies that the effect of diabetes, and factors linked to the diabetes state, is substantial in the progression of arterial stiffness.
One of the strengths of this study is that it is a large population-based cohort with a long follow-up period. Although it can be argued that the final study population was health-selected as many individuals with poor health died before the re-examination, it has been demonstrated that the study cohort was representative of the population in terms of baseline characteristics, when examined through a mailed health survey (participation rate 75%) [28]. Another strength of the study is that the analysis was adjusted for majority of major risk factors at baseline and follow-up. Hence, the results indicate that systemic inflammation is a potential determinant for arterial stiffness. However, one of the limitations of the study is that the c-f PWV and plasma levels for acute phase proteins were measured only once and separated in time. No further measurements were carried out at follow-up examination to evaluate the change in plasma levels over this period. It has been shown that levels of inflammatory markers are quite stable over time in healthy individuals [53, 54]. It has been reported that the variability of CRP over a one-year period is comparable to that of cholesterol [53]. Nevertheless, it can be assumed that a random misclassification would reduce the associations between c-f PWV and inflammation.
Even though c-f PWV is a valid measure of the arterial stiffness in the aortic and aorto-iliac vascular tree, it should be acknowledged that c-f PWV does not reflect the heterogeneity which occurs in various primary and secondary branches. A recent study by Weir-McCall et al. demonstrated differences in carotid-femoral measured PWV and MRI measured aortic PWV, which can be for the most part be explained by use of simple surface measurements [55]. Nevertheless, distance estimation has been performed in a standardized way in this study. It should also be acknowledged that the statistical power was limited when comparing patients with diabetes, and it is possible that a larger sample would result in significant differences. It should also be noted that these patients with diabetes were mostly treated by a number of drugs (also anti-diabetic drugs) and this could have reduced the prediction of acute phase reactants.
In conclusion, this prospective population-based cohort study shows that alpha-1-antitrypsin, C3 and CRP are associated with c-f PWV and, therefore, arterial stiffness. This observation suggests that inflammation may be involved in the pathogenesis of arterial stiffening. The results also indicated that individuals with diabetes had increased c-f PWV. However, this relationship was not explained by raised inflammatory proteins. A better understanding of the underlying mechanism of association between low grade inflammation and arterial stiffness is necessary, due to its important implications on future diagnosis, risk stratification, and potential therapeutic approach of cardiovascular diseases.
Acknowledgments
We thank the staff at the Clinical Research Unit for conducting the technical examinations.
Data Availability
The authors do not own the data underlying this study. The data are owned by Lund University, and the approval for research from this database is obtained through the Malmö Diet and Cancer Study (MDCS) steering committee. The data cannot be made publicly available without ethical approval. Data are available upon request for interested researchers by applying to MDCS steering committee. Please email (Anders.Dahlin@med.lu.se) with requests for the data.
Funding Statement
This MDC Re-exam study was supported by the Medical Research Council of Sweden (grant K2011-65X-20752-04-6; 2014-2265), the Region Skåne County Council (ALF), the Swedish Heart and Lung foundation (grant 20150469) and Ernhold Lundstrom Foundation. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Vlachopoulos C, Aznaouridis K, Stefanadis C. Prediction of cardiovascular events and all-cause mortality with arterial stiffness: a systematic review and meta-analysis. J Am Coll Cardiol 2010. March 30;55(13):1318–1327. [DOI] [PubMed] [Google Scholar]
- 2.Ben-Shlomo Y, Spears M, Boustred C, May M, Anderson SG, Benjamin EJ, et al. Aortic Pulse Wave Velocity Improves Cardiovascular Event Prediction: An Individual Participant Meta-Analysis of Prospective Observational Data From 17,635 Subjects. J Am Coll Cardiol 2014. February/25;63(7):636–646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Meaume S, Benetos A, Henry OF, Rudnichi A, Safar ME. Aortic pulse wave velocity predicts cardiovascular mortality in subjects >70 years of age. Arterioscler Thromb Vasc Biol 2001. December;21(12):2046–2050. [DOI] [PubMed] [Google Scholar]
- 4.Cruickshank K, Riste L, Anderson SG, Wright JS, Dunn G, Gosling RG. Aortic pulse-wave velocity and its relationship to mortality in diabetes and glucose intolerance: an integrated index of vascular function? Circulation 2002. October 15;106(16):2085–2090. [DOI] [PubMed] [Google Scholar]
- 5.Laurent S, Boutouyrie P, Asmar R, Gautier I, Laloux B, Guize L, et al. Aortic stiffness is an independent predictor of all-cause and cardiovascular mortality in hypertensive patients. Hypertension 2001. May;37(5):1236–1241. [DOI] [PubMed] [Google Scholar]
- 6.Blacher J, Guerin AP, Pannier B, Marchais SJ, Safar ME, London GM. Impact of aortic stiffness on survival in end-stage renal disease. Circulation 1999. May 11;99(18):2434–2439. [DOI] [PubMed] [Google Scholar]
- 7.Laurent S, Cockcroft J, Van Bortel L, Boutouyrie P, Giannattasio C, Hayoz D, et al. Expert consensus document on arterial stiffness: methodological issues and clinical applications. Eur Heart J 2006. November;27(21):2588–2605. doi: 10.1093/eurheartj/ehl254 [DOI] [PubMed] [Google Scholar]
- 8.Townsend RR, Black HR, Chirinos JA, Feig PU, Ferdinand KC, Germain M, et al. Clinical Use of Pulse Wave Analysis: Proceedings From a Symposium Sponsored by North American Artery. J Clin Hypertens (Greenwich) 2015. July;17(7):503–513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kelly RP, Tunin R, Kass DA. Effect of reduced aortic compliance on cardiac efficiency and contractile function of in situ canine left ventricle. Circ Res 1992. September;71(3):490–502. [DOI] [PubMed] [Google Scholar]
- 10.Nitta K, Akiba T, Uchida K, Otsubo S, Otsubo Y, Takei T, et al. Left ventricular hypertrophy is associated with arterial stiffness and vascular calcification in hemodialysis patients. Hypertens Res 2004. January;27(1):47–52. [DOI] [PubMed] [Google Scholar]
- 11.McEniery CM, Yasmin, Hall IR, Qasem A, Wilkinson IB, Cockcroft JR. Normal Vascular Aging: Differential Effects on Wave Reflection and Aortic Pulse Wave Velocity: The Anglo-Cardiff Collaborative Trial (ACCT). J Am Coll Cardiol 2005. November/1;46(9):1753–1760. doi: 10.1016/j.jacc.2005.07.037 [DOI] [PubMed] [Google Scholar]
- 12.Cecelja M, Chowienczyk P. Dissociation of aortic pulse wave velocity with risk factors for cardiovascular disease other than hypertension: a systematic review. Hypertension 2009. December;54(6):1328–1336. doi: 10.1161/HYPERTENSIONAHA.109.137653 [DOI] [PubMed] [Google Scholar]
- 13.Prenner SB, Chirinos JA. Arterial stiffness in diabetes mellitus. Atherosclerosis 2015. February;238(2):370–379. doi: 10.1016/j.atherosclerosis.2014.12.023 [DOI] [PubMed] [Google Scholar]
- 14.Sa Cunha R, Pannier B, Benetos A, Siche JP, London GM, Mallion JM, et al. Association between high heart rate and high arterial rigidity in normotensive and hypertensive subjects. J Hypertens 1997. December;15(12 Pt 1):1423–1430. [DOI] [PubMed] [Google Scholar]
- 15.Strasser B, Arvandi M, Pasha EP, Haley AP, Stanforth P, Tanaka H. Abdominal obesity is associated with arterial stiffness in middle-aged adults. Nutr Metab Cardiovasc Dis 2015. May;25(5):495–502. doi: 10.1016/j.numecd.2015.01.002 [DOI] [PubMed] [Google Scholar]
- 16.Benetos A, Adamopoulos C, Bureau JM, Temmar M, Labat C, Bean K, et al. Determinants of accelerated progression of arterial stiffness in normotensive subjects and in treated hypertensive subjects over a 6-year period. Circulation 2002. March 12;105(10):1202–1207. [DOI] [PubMed] [Google Scholar]
- 17.Engstrom G, Stavenow L, Hedblad B, Lind P, Tyden P, Janzon L, et al. Inflammation-sensitive plasma proteins and incidence of myocardial infarction in men with low cardiovascular risk. Arterioscler Thromb Vasc Biol 2003. December;23(12):2247–2251. doi: 10.1161/01.ATV.0000102924.11767.8D [DOI] [PubMed] [Google Scholar]
- 18.Engstrom G, Janzon L, Berglund G, Lind P, Stavenow L, Hedblad B, et al. Blood pressure increase and incidence of hypertension in relation to inflammation-sensitive plasma proteins. Arterioscler Thromb Vasc Biol 2002. December 1;22(12):2054–2058. [DOI] [PubMed] [Google Scholar]
- 19.Jain S, Khera R, Corrales-Medina VF, Townsend RR, Chirinos JA. "Inflammation and arterial stiffness in humans". Atherosclerosis 2014. December;237(2):381–390. doi: 10.1016/j.atherosclerosis.2014.09.011 [DOI] [PubMed] [Google Scholar]
- 20.Muhammad IF, Borne Y, Hedblad B, Nilsson PM, Persson M, Engstrom G. Acute-phase proteins and incidence of diabetes: a population-based cohort study. Acta Diabetol. 2016. December;53(6):981–989. doi: 10.1007/s00592-016-0903-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Maki-Petaja KM, Hall FC, Booth AD, Wallace SM, Yasmin, Bearcroft PW, et al. Rheumatoid arthritis is associated with increased aortic pulse-wave velocity, which is reduced by anti-tumor necrosis factor-alpha therapy. Circulation 2006. September 12;114(11):1185–1192. doi: 10.1161/CIRCULATIONAHA.105.601641 [DOI] [PubMed] [Google Scholar]
- 22.Sacre K, Escoubet B, Pasquet B, Chauveheid MP, Zennaro MC, Tubach F, et al. Increased arterial stiffness in systemic lupus erythematosus (SLE) patients at low risk for cardiovascular disease: a cross-sectional controlled study. PLoS One 2014. April 10;9(4):e94511 doi: 10.1371/journal.pone.0094511 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zanoli L, Cannavo M, Rastelli S, Di Pino L, Monte I, Di Gangi M, et al. Arterial stiffness is increased in patients with inflammatory bowel disease. J Hypertens 2012. September;30(9):1775–1781. doi: 10.1097/HJH.0b013e3283568abd [DOI] [PubMed] [Google Scholar]
- 24.Moyssakis I, Gialafos E, Vassiliou V, Taktikou E, Katsiari C, Papadopoulos DP, et al. Aortic stiffness in systemic sclerosis is increased independently of the extent of skin involvement. Rheumatology (Oxford) 2005. February;44(2):251–254. [DOI] [PubMed] [Google Scholar]
- 25.Yasmin, McEniery CM, Wallace S, Mackenzie IS, Cockcroft JR, Wilkinson IB. C-reactive protein is associated with arterial stiffness in apparently healthy individuals. Arterioscler Thromb Vasc Biol 2004. May;24(5):969–974. doi: 10.1161/01.ATV.zhq0504.0173 [DOI] [PubMed] [Google Scholar]
- 26.London GM, Marchais SJ, Guerin AP, Metivier F, Adda H, Pannier B. Inflammation, arteriosclerosis, and cardiovascular therapy in hemodialysis patients. Kidney Int Suppl 2003. May;(84)(84):S88–93. doi: 10.1046/j.1523-1755.63.s84.25.x [DOI] [PubMed] [Google Scholar]
- 27.Gottsater M, Ostling G, Persson M, Engstrom G, Melander O, Nilsson PM. Non-hemodynamic predictors of arterial stiffness after 17 years of follow-up: the Malmo Diet and Cancer study. J Hypertens 2015. May;33(5):957–965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Manjer J, Carlsson S, Elmstahl S, Gullberg B, Janzon L, Lindstrom M, et al. The Malmo Diet and Cancer Study: representativity, cancer incidence and mortality in participants and non-participants. Eur J Cancer Prev 2001. December;10(6):489–499. [DOI] [PubMed] [Google Scholar]
- 29.Hedblad B, Nilsson P, Janzon L, Berglund G. Relation between insulin resistance and carotid intima-media thickness and stenosis in non-diabetic subjects. Results from a cross-sectional study in Malmo, Sweden. Diabet Med 2000. April;17(4):299–307. [DOI] [PubMed] [Google Scholar]
- 30.Rosvall M, Persson M, Ostling G, Nilsson PM, Melander O, Hedblad B, et al. Risk factors for the progression of carotid intima-media thickness over a 16-year follow-up period: the Malmo Diet and Cancer Study. Atherosclerosis 2015. April;239(2):615–621. doi: 10.1016/j.atherosclerosis.2015.01.030 [DOI] [PubMed] [Google Scholar]
- 31.Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem 1972. June;18(6):499–502. [PubMed] [Google Scholar]
- 32.Alberti KG, Zimmet PZ. Definition, diagnosis and classification of diabetes mellitus and its complications. Part 1: diagnosis and classification of diabetes mellitus provisional report of a WHO consultation. Diabet Med 1998. July;15(7):539–553. doi: 10.1002/(SICI)1096-9136(199807)15:7<539::AID-DIA668>3.0.CO;2-S [DOI] [PubMed] [Google Scholar]
- 33.Enhorning S, Sjogren M, Hedblad B, Nilsson PM, Struck J, Melander O. Genetic vasopressin 1b receptor variance in overweight and diabetes mellitus. Eur J Endocrinol 2016. January;174(1):69–75. doi: 10.1530/EJE-15-0781 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mancia G, De Backer G, Dominiczak A, Cifkova R, Fagard R, Germano G, et al. 2007 Guidelines for the management of arterial hypertension: The Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur Heart J 2007. June;28(12):1462–1536. doi: 10.1093/eurheartj/ehm236 [DOI] [PubMed] [Google Scholar]
- 35.Vanfleteren LE, Spruit MA, Groenen MT, Bruijnzeel PL, Taib Z, Rutten EP, et al. Arterial stiffness in patients with COPD: the role of systemic inflammation and the effects of pulmonary rehabilitation. Eur Respir J 2014. May;43(5):1306–1315. doi: 10.1183/09031936.00169313 [DOI] [PubMed] [Google Scholar]
- 36.Duckers JM, Shale DJ, Stockley RA, Gale NS, Evans BA, Cockcroft JR, et al. Cardiovascular and musculskeletal co-morbidities in patients with alpha 1 antitrypsin deficiency. Respir Res 2010. December 7;11:173-9921-11-173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Dahl M, Tybjaerg-Hansen A, Sillesen H, Jensen G, Steffensen R, Nordestgaard BG. Blood pressure, risk of ischemic cerebrovascular and ischemic heart disease, and longevity in alpha(1)-antitrypsin deficiency: the Copenhagen City Heart Study. Circulation 2003. February 11;107(5):747–752. [DOI] [PubMed] [Google Scholar]
- 38.O'Rourke MF, Safar ME, Dzau V. The Cardiovascular Continuum extended: aging effects on the aorta and microvasculature. Vasc Med 2010. December;15(6):461–468. doi: 10.1177/1358863X10382946 [DOI] [PubMed] [Google Scholar]
- 39.Bjarnegrad N, Bengtsson C, Brodszki J, Sturfelt G, Nived O, Lanne T. Increased aortic pulse wave velocity in middle aged women with systemic lupus erythematosus. Lupus 2006;15(10):644–650. doi: 10.1177/0961203306071402 [DOI] [PubMed] [Google Scholar]
- 40.Engstrom G, Hedblad B, Berglund G, Janzon L, Lindgarde F. Plasma levels of complement C3 is associated with development of hypertension: a longitudinal cohort study. J Hum Hypertens 2007. April;21(4):276–282. doi: 10.1038/sj.jhh.1002129 [DOI] [PubMed] [Google Scholar]
- 41.Muscari A, Bozzoli C, Puddu GM, Sangiorgi Z, Dormi A, Rovinetti C, et al. Association of serum C3 levels with the risk of myocardial infarction. Am J Med 1995. April;98(4):357–364. doi: 10.1016/S0002-9343(99)80314-3 [DOI] [PubMed] [Google Scholar]
- 42.Shields KJ, Stolz D, Watkins SC, Ahearn JM. Complement proteins C3 and C4 bind to collagen and elastin in the vascular wall: a potential role in vascular stiffness and atherosclerosis. Clin Transl Sci 2011. June;4(3):146–152. doi: 10.1111/j.1752-8062.2011.00304.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Duprez DA, Somasundaram PE, Sigurdsson G, Hoke L, Florea N, Cohn JN. Relationship between C-reactive protein and arterial stiffness in an asymptomatic population. J Hum Hypertens 2005. July;19(7):515–519. doi: 10.1038/sj.jhh.1001860 [DOI] [PubMed] [Google Scholar]
- 44.Mattace-Raso FU, van der Cammen TJ, van der Meer IM, Schalekamp MA, Asmar R, Hofman A, et al. C-reactive protein and arterial stiffness in older adults: the Rotterdam Study. Atherosclerosis 2004. September;176(1):111–116. doi: 10.1016/j.atherosclerosis.2004.04.014 [DOI] [PubMed] [Google Scholar]
- 45.Johansen NB, Vistisen D, Brunner EJ, Tabak AG, Shipley MJ, Wilkinson IB, et al. Determinants of aortic stiffness: 16-year follow-up of the Whitehall II study. PLoS One 2012;7(5):e37165 doi: 10.1371/journal.pone.0037165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.McEniery CM, Spratt M, Munnery M, Yarnell J, Lowe GD, Rumley A, et al. An analysis of prospective risk factors for aortic stiffness in men: 20-year follow-up from the Caerphilly prospective study. Hypertension 2010. July;56(1):36–43. doi: 10.1161/HYPERTENSIONAHA.110.150896 [DOI] [PubMed] [Google Scholar]
- 47.Amar J, Ruidavets JB, Bal Dit Sollier C, Bongard V, Boccalon H, Chamontin B, et al. Relationship between C reactive protein and pulse pressure is not mediated by atherosclerosis or aortic stiffness. J Hypertens 2004. February;22(2):349–355. [DOI] [PubMed] [Google Scholar]
- 48.Pasceri V, Willerson JT, Yeh ET. Direct proinflammatory effect of C-reactive protein on human endothelial cells. Circulation 2000. October 31;102(18):2165–2168. [DOI] [PubMed] [Google Scholar]
- 49.Schumacher W, Cockcroft J, Timpson NJ, McEniery CM, Gallacher J, Rumley A, et al. Association between C-reactive protein genotype, circulating levels, and aortic pulse wave velocity. Hypertension 2009. February;53(2):150–157. doi: 10.1161/HYPERTENSIONAHA.108.117622 [DOI] [PubMed] [Google Scholar]
- 50.Schram MT, Henry RM, van Dijk RA, Kostense PJ, Dekker JM, Nijpels G, et al. Increased central artery stiffness in impaired glucose metabolism and type 2 diabetes: the Hoorn Study. Hypertension 2004. February;43(2):176–181. doi: 10.1161/01.HYP.0000111829.46090.92 [DOI] [PubMed] [Google Scholar]
- 51.Henry RM, Kostense PJ, Spijkerman AM, Dekker JM, Nijpels G, Heine RJ, et al. Arterial stiffness increases with deteriorating glucose tolerance status: the Hoorn Study. Circulation 2003. April 29;107(16):2089–2095. doi: 10.1161/01.CIR.0000065222.34933.FC [DOI] [PubMed] [Google Scholar]
- 52.Shen L, Zhang YG, Liu M, Qiang DC, Sun XL, Liu L, et al. Increased arterial stiffness in subjects with pre-diabetes among middle aged population in Beijing, China. Biomed Environ Sci 2013. September;26(9):717–725. doi: 10.3967/0895-3988.2013.09.002 [DOI] [PubMed] [Google Scholar]
- 53.Ockene IS, Matthews CE, Rifai N, Ridker PM, Reed G, Stanek E. Variability and classification accuracy of serial high-sensitivity C-reactive protein measurements in healthy adults. Clin Chem 2001. March;47(3):444–450. [PubMed] [Google Scholar]
- 54.Sebastian-Gambaro MA, Liron-Hernandez FJ, Fuentes-Arderiu X. Intra- and inter-individual biological variability data bank. Eur J Clin Chem Clin Biochem 1997. November;35(11):845–852. [PubMed] [Google Scholar]
- 55.Weir-McCall JR, Khan F, Cassidy DB, Thakur A, Summersgill J, Matthew SZ, et al. Effects of inaccuracies in arterial path length measurement on differences in MRI and tonometry measured pulse wave velocity. BMC Cardiovasc Disord 2017. May 10;17(1):118-017-0546-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The authors do not own the data underlying this study. The data are owned by Lund University, and the approval for research from this database is obtained through the Malmö Diet and Cancer Study (MDCS) steering committee. The data cannot be made publicly available without ethical approval. Data are available upon request for interested researchers by applying to MDCS steering committee. Please email (Anders.Dahlin@med.lu.se) with requests for the data.