Abstract
Objective
The objective of this study was to compare the timing of hearing aid (HA) acquisition between adult in rural and urban communities. We hypothesized that time of acquisition of HA after onset of hearing loss is greater in rural adults compared with urban adults. Secondary objectives included assessment of socioeconomic/educational status and impact of hearing loss and hearing rehabilitation of urban and rural HA recipients.
Study Design
Cross-sectional questionnaire survey
Methods
We assessed demographics, timing of HA fitting from onset of hearing loss, and impact of hearing impairment in 336 adult HA recipients (273 urban, 63 rural) from a tertiary referral center. Amplification benefit was assessed using the International Outcome Inventory for Hearing Aids (IOI).
Results
The time to HA acquisition was greater for rural participants compared to urban participants (19.1 versus 25.7 years, p=0.024) for those with untreated hearing loss for at least 8 years. Age at hearing loss onset was correlated with time to HA acquisition (ρ=−0.54, p<0.001). Rural HA participants experienced longer commutes to hearing specialists (68 versus 32 minutes, p<0.001), were less likely to achieve a degree beyond high school (p<0.001), and were more likely to possess Medicaid coverage (p=0.012) compared to urban participants. Hearing impairment caused job performance difficulty in 60% of all participants.
Conclusions
Rural adults are at risk for delayed HA acquisition, which may be related to distance to hearing specialists. Further research is indicated to investigate barriers to care and expand access for vulnerable populations.
Level of Evidence
4
Keywords: Rural Health, Adult hearing loss, Hearing aids, Hearing healthcare disparities, Socioeconomic factors, Health Disparities
INTRODUCTION
Hearing loss affects 21.7% of U.S. adults1 and, like many healthcare disparities, untreated hearing loss is more prevalent in rural areas—twice as common by one estimate.2 Moreover, hearing impairment prevalence is positively correlated with poverty, reduced educational attainment, and manual labor occupations3 — characteristics more prominent in rural communities. This public health issue is of economic importance to the 46 million residents of rural counties in the United States.4 Adults with hearing loss are more than twice as likely to be unemployed or partly unemployed, and they experience a 25% decrease in wages compared to those without hearing loss.5 Severe to profound hearing loss is estimated to cost an individual $410,000 over their lifetime, chiefly due to decreased work productivity.6 This disability and economic impact may adversely affect rural communities already facing higher poverty rates and unemployment.7 Untreated hearing loss also causes a measurable impact to the mental and emotional well being of adults. Those experiencing hearing problems are more likely to have mood disorders and to experience feelings of social inferiority.8 Poorer quality of life is also linked with hearing impairment.9 Cognitive decline in an aging population with hearing loss is linked to failure in obtaining treatment.10
Hearing aids are a well-known and effective treatment for unilateral and bilateral hearing loss. However, hearing aid uptake remains low, 21–48%, among those with hearing loss.11–13 There are many factors that may lead to the delayed diagnosis and treatment of adult hearing loss. Awareness of the benefits of timely hearing loss diagnosis and treatment is low among the general population and among health-care professionals.14,15 Screening for hearing loss among adults is uncommon in the primary care setting and there is poor adherence to recommended treatment.16,17 Of adults that undergo hearing screening, 72% are in the precontemplation or contemplation stages with no plan to take action regarding their hearing loss.18 This may account for the finding that adults typically wait 10 years to seek assistance after first experiencing hearing loss.19 There is also a shortage of hearing healthcare specialists in rural regions.1,5,20 The presence of disparities in diagnostic and intervention services result in rural patients being at a high risk of delayed treatment for a variety of health conditions.21–23 Patients in rural areas face limited access to specialty care that compounds these concerns in the hearing loss field. There is evidence that rural pediatric patients with severe hearing loss are delayed in cochlear implantation when compared to patients from urban areas.24 In order to mitigate the effects of untreated hearing loss in vulnerable populations and understand factors that serve as barriers to adult hearing healthcare, it is paramount to investigate the timing of hearing aid amplification after hearing loss onset in rural adults compared with urban adults. The primary objective of this study was to compare the timing of hearing aid acquisition between adult hearing aid recipients in rural and urban communities. Additionally, we sought to compare the two populations in regards to socioeconomic characteristics, the impact of hearing loss on occupation and education, and the usage and self-assessed benefits of hearing aids.
METHODS
Institutional review board approval was obtained prior to initiation of this study (protocol 14-0854-F1V). Study participants were derived from all adult hearing aid patients who were fit with aids at age 18 or older between 2011 and 2014 at clinics associated with a single university. The hearing aid fittings occurred either at the main university otolaryngology clinic in a major metropolitan area or at a university-associated rural, otolaryngology satellite clinic approximately 70 miles away. The operation of the 2 clinics is identical regarding staffing and appointment access. To assess the timing of hearing healthcare access and occupational and educational impact of hearing loss, we developed a 25-item questionnaire (Appendix). We consulted the prior literature, patients, and providers in the development of this novel instrument. Prior to utilizing the questionnaire, the document was piloted with patients with hearing loss and modifications were made to improve clarity and brevity. The International Outcomes Inventory for Hearing Aids (IOI-HA)—a 7-item standardized and validated instrument assessing the use and efficacy of hearing aids—was also included with the newly developed questionnaire.25 The survey was sent with a cover letter and a stamped return envelope to eligible patients.
The questionnaire included fill in the blanks, open-ended semi-structured, multiple choice, and yes/no questions. Questions with 4-point Likert-type scale answers were also utilized. Data collected included county of residence and demographic factors such as gender, race, age, marital status, educational level, household income, and insurance coverage. Participants then indicated whether hearing aids were used in one or both ears. We assessed duration of hearing loss and the time interval between onset of hearing loss and acquisition of hearing aids. These intervals were computed from self-reported responses of how long ago hearing loss and other events—disruption of daily activities, seeking care, and the acquisition of hearing aids—occurred. Participants also recorded their travel time to their audiologist. The impact of hearing loss on educational and occupational factors was explored with 4-point Likert-style questions. Participants were asked about hearing problems causing difficulty in the following: performing one’s job, achieving a promotion, obtaining a job, retaining a job, and completing education in the past. Discrimination in the workplace and the desire to have completed a higher level of education were similarly assessed. The survey concluded with the IOI-HA instrument.
Returned questionnaires were collected and entered electronically into Research Electronic Data Capture database (REDCap) (Vanderbilt University, Nashville, TN). Survey data were managed using an Excel spreadsheet (Microsoft, Redmond, WA, USA) and statistical analysis was performed with SAS software (SAS Institute Inc., Cary, NC, USA). Surveys were separated, based on patient-reported county of residence, to an urban or rural group based on each county’s Beale code (US Department of Agriculture Rural-Urban Continuum Coding system).26 This system is a numerical scale from 1 to 9, with the most urban county being 1 with a metro population of 1 million or more, and the most rural county scored as 9, meaning one with less than 2,500 urban residents and no adjacency to a metro area. Beale codes 1 through 6 are considered urban-suburban and 7 through 9 are considered rural counties. The literature indicates a delay of 10 years from onset of hearing loss to acquiring hearing aid amplification and was used to perform a power analysis.19 Based on this literature and an estimated standard deviation of 10 years, we selected a goal sample size of 360 patients in order to detect a difference of 3 years between the urban and rural groups and in order to have 80% power to detect this difference using a 2 sample t-test (at the 0.05 significance level).
Survey responses between these two groups were compared using Student’s t-test for continuous data, the Mann Whitney U test for ordinal and non-normally distributed data, and Chi-Squared analysis or Fisher’s exact test for categorical data. Correlation analysis was conducted between select variables and the primary outcome: the time to hearing aid acquisition. Pearson correlation coefficients were calculated for continuous variables, Spearman correlation coefficients were used for ordinal variables, and analysis of variance testing was employed for categorical variables. P-values less than 0.05 were considered statistically significant.
RESULTS
A summary of demographic and socioeconomic data is found in Table 1. Of the 953 questionnaires sent, 40 questionnaires could not be completed by the intended participant for reasons such as death of the recipient or undeliverable addresses. Three hundred thirty six participants returned questionnaires (36% overall response rate), 273 urban participants (38% response rate) and 63 rural participants (31% response rate). There was a significant difference between the two groups for household income (p<0.001). Rural participants experienced longer commutes to hearing specialists (p<0.001), were less likely to receive education beyond high school (66% vs 90%, p<0.001) and were more likely to possess Medicaid coverage (p=0.012) compared to urban participants.
Table 1.
Comparison of demographics in urban and rural adult hearing aid recipients
| Characteristic | Urban | Rural | p-value |
|---|---|---|---|
| Population Size | 273 | 63 | |
| Mean age (years) | 66.3 | 66.7 | 0.864 |
| Mean commute time to audiologist (min) | 32 | 68 | <.0001 |
| Male sex (%) | 51% | 49% | 0.807 |
| Race/Ethnicity* | |||
| White | 96% | 100% | 0.090 |
| African American | 3% | 0% | 0.355f |
| Hispanic | 0.7% | 0% | 1.000f |
| Native American | 1% | 0% | 1.000f |
| Other | 0.7% | 0% | 1.000f |
| Education (%) | <0.001 | ||
| No degree | 1% | 10% | 0.002f |
| High School or Equivalent | 9% | 24% | 0.001 |
| Post-secondary education | 22% | 24% | 0.753 |
| College graduate | 26% | 15% | 0.055 |
| Graduate degree | 42% | 27% | 0.030 |
| Income (%) | <0.001 | ||
| Less than $10,000 | 2% | 5% | 0.174f |
| $10,000–20,000 | 7% | 11% | 0.416 |
| $20,000–30,000 | 7% | 11% | 0.416 |
| $30,000–60,000 | 25% | 39% | 0.080 |
| More than $60,000 | 59% | 34% | <0.001 |
| Insurance (%)* | |||
| Medicaid | 4% | 13% | 0.012 |
| Medicare | 51% | 57% | 0.345 |
| Private | 63% | 51% | 0.065 |
| Other | 24% | 37% | 0.046 |
| Hearing Aid Use (%) | 0.426 | ||
| Unilateral | 17% | 11% | |
| Bilateral | 80% | 87% | |
Percentages do not add to 100% due to multiple selections possible.
Fisher’s Exact test used due to anticipated frequency < 5 in one of the categories.
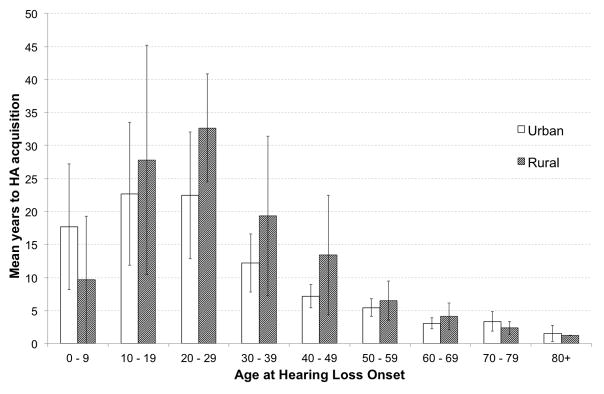
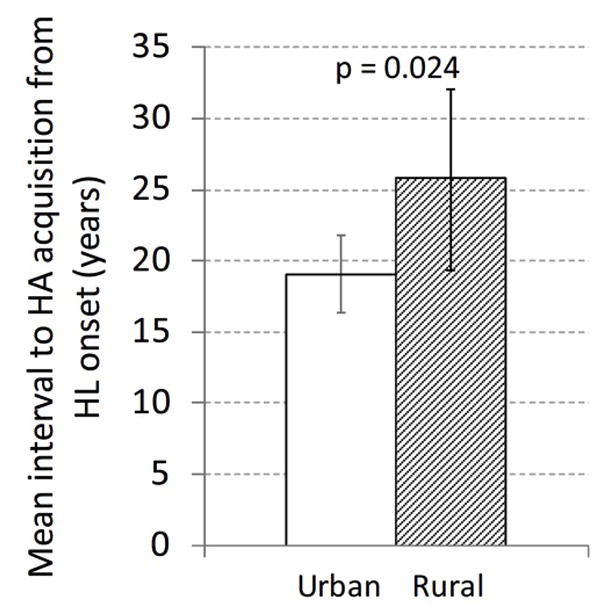
Overall, rural participants reported an average time interval of 10.9 years between onset of hearing loss and acquisition of hearing aids compared with 7.9 years in urban/suburban participants (p=0.218). For patients with at least 8 years of untreated hearing loss (N=107), we found that rural adults had a greater time interval between onset of hearing loss until acquisition of hearing aids (25.7 years versus 19.1 years, p=0.024, Figure 1). Time to hearing aid acquisition was found to have a moderate negative correlation to age at hearing loss onset (Pearson r = −0.539, p<0.001, Figure 2). Additionally, time to hearing aid acquisition was also found to have a weak positive correlation with travel time to the audiologist (Pearson r = 0.191, p<0.001) and a weak negative correlation with the self-reported impact of hearing impairment on job performance (Spearman ρ = −0.193, p<0.001). The time to hearing aid acquisition was not significantly correlated with income, age at hearing aid acquisition, frequency of primary care physician visits, nor self-reported difficulty in seeing an audiologist. Other categorical variables—insurance status, education level, and whether hearing impairment ever interfered with daily activities—were not statistically significant.
Figure 1.
Mean time interval from hearing loss onset until hearing aid acquisition in urban and rural subjects with at least 8 years of untreated hearing loss.
Figure 2.
Mean interval from hearing loss onset to hearing aid acquisition by age at hearing loss onset. Error bars represent 95% confidence intervals.
Self-reported data regarding impact of hearing loss on employment and education revealed some pertinent findings (Table 2). Few participants reported difficulty in hiring or promotion or discrimination in the workplace related to their hearing loss and approximately 1% or less reported job loss related to their hearing loss. However, participants reported job performance difficulty related to hearing impairment in 61% of urban residents and 57% of rural residents. A higher percentage of rural adult hearing aid recipients wish that they had achieved a higher level of education (p=0.019) and identified their hearing loss as an educational barrier (p=0.048) compared with urban residents. In spite of the impact of hearing loss on employment and education attainment, substantial and consistent benefits from hearing aid use were observed from both groups on the IOI-HA (Figure 3). On average, participants reported using their hearing aids at least 4 to 8 hours a day and that those hearing aids made their quality of life “quite a lot better.” All participants reported amplification benefit with a non-statistically significant trend toward greater benefit in rural participants.
Table 2.
Comparison of education and job-related effects of hearing loss in urban and rural hearing aid recipients.
| Self-Reported Impact of HL on Job & Education (% agree or strongly agree) | Urban | Rural | p-value |
|---|---|---|---|
| Difficulty performing job | 61% | 56% | 0.471 |
| Prevented hiring | 5% | 11% | 0.166 |
| Caused loss of job | 1% | 0% | 1.000f |
| Prevented promotion | 5% | 11% | 0.251f |
| Caused discrimination in workplace | 8% | 3% | 0.312f |
| Wish had completed higher education in past | 36% | 54% | 0.019 |
| Prevented from completing education in past | 4% | 12% | 0.048 |
Fisher’s Exact test used due to anticipated frequency < 5 in one of the categories.
Figure 3.
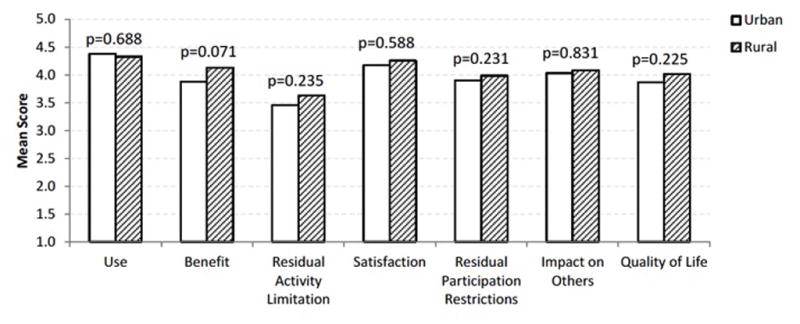
IOI-HA mean scores for urban and rural hearing aid recipients. P-values listed are derived from Mann Whitney U testing.
DISCUSSION
This study demonstrates a delay in the timing of hearing aid acquisition in rural adult with hearing loss compared with urban adults. These findings are important because approximately 20% of the U.S. population reside in rural areas,27 and adults within these areas represent a vulnerable population with barriers to accessing hearing healthcare. Rural barriers to care is not unique to the United States as a similar trend in delayed access to hearing healthcare in remote regions has been reported by Brennan-Jones et al in Australia.2 This study demonstrates that distance from hearing healthcare services was associated with the timing of acquisition of hearing aids. Rural participants in this study reported an average travel time of over 1 hour to obtain audiological services (compared with 32 minutes in the urban sample). A prior study by Arcury et al28 involving a rural population found that the number of regular check-ups in a primary care setting was inversely related to distance to the provider. This type of rural healthcare disparity has been similarly documented for specialty healthcare services, such as Optometry.29 Primary care providers in rural settings are less likely to consult a visual specialist due to the reality that few specialists are available to meet the specialty healthcare needs.30 The lack of local resources may prevent timely diagnostic testing and may decrease the likelihood of obtaining hearing aids.31,32 Limited appointment times and increased travel time to audiologists negatively affect hearing healthcare seeking behavior.31,33,34 There is a concerning shortage of audiologists to meet expanding clinical demands20 and there is a need to explore different models of service delivery such as that which has been reported by visual healthcare services.29
Financial constraints and lack of or inadequate insurance coverage have been demonstrated in other studies to be significant barriers for healthcare for rural and other vulnerable populations.35,36 Positive social support and gainful employment may help mitigate these economic barriers to hearing healthcare.35 This study did not identify an association between the timing of access to hearing healthcare and income or insurance status. The lack of a relationship between of timing of amplification and income level could be due to incorrect or incomplete reporting of income on this self-reported questionnaire. Additionally, state-funded programs (such as vocational rehabilitation) have provided hearing aids for working adults at low or no cost, regardless of insurance status. Eligibility for these programs are partially dependent on income and lower income working adults would have a higher likelihood of qualifying for this type of assistance and this factor could have decreased the time to amplification.
Access to care may be complicated by a variety of interacting patient and cultural factors within vulnerable populations. Overall health of rural adults is poorer than urban adults37 and those with competing health conditions are less likely to receive timely hearing healthcare.34,38 Lack of social support limits seeking of hearing healthcare.31 Rural adults may have different cultural perceptions, such as a fear of compromised confidentiality in the receipt of care, which can affect rural patients’ healthcare seeking behavior.39 Additionally, a negative social stigma within rural cultures related to hearing aid use and fear of compromised social identity may prevent some adults from seeking hearing healthcare.40,41,31
The impact of the hearing healthcare access delay in rural residents on auditory outcomes and quality of life is unknown and the key determinants in timely access to care are undefined. Thus far, substantial research has demonstrated the mental health, financial, and occupational impact of hearing impairment in the general adult population.1,5,6 Significant in our analysis was the inverse correlation between age at hearing loss and time to hearing aid acquisition. When hearing loss onset occurs in adolescents and young adults (age 10–29), hearing aids are not acquired until, on average, 25 years later. When hearing loss onset occurs later in life (>60 years) the average time to obtain amplification is 3 years. While variance in the progression of this acquired hearing loss may explain some of these differences, this discrepancy highlights the importance of access to hearing healthcare for these communities as it relates to educational and occupational opportunities. Our survey has shown that 60% of our subjects experienced difficulty in performing their job because of hearing impairment, and over half of rural subjects wish they had completed more education. With the consistently positive usage demonstrated on the IOI, it will be critical to continue investigating how to improve access to hearing aids in this affected population.
This study is limited by recall bias. We relied on participants’ recall of their hearing healthcare milestones from the past. While objective records of hearing loss onset and the subsequent events would be preferable, such analysis would require retrospective review, which is also limited by reporting errors. The response rate for this study is modest but is reasonable considering the nature of this research. The response rates are similar among the rural and urban participants (31% vs 38%). Participation by hearing aid recipients may also be hindered by literacy rates and other socioeconomic factors, potentially introducing selection bias. It must also be noted that conclusions from this study are derived from those that have succeeded in acquiring hearing aids; thus, adults that have not received hearing aids may have different characteristics and barriers to care. The rural participants reported receiving at least equal, if not more benefit from hearing aids than their urban counterparts. Hypothetically, a selection bias may account for this finding, in that, adults that are delayed in access could have more severe hearing loss at the time of fitting and even modest improvement of hearing function could translate into high satisfaction. Hearing loss severity was not assessed in this study sample. The participants of this study were from one geographical region and results may not be generalizable to other regions.
This study assesses hearing impairment and access to hearing healthcare in rural and urban communities. Further research is needed to improve access to care in vulnerable populations. Furthermore, improving access to care in working adults, especially those at high risk of hearing loss, is critical. There is existing evidence demonstrating improved hearing aid use and better rehabilitation outcomes among adults treated at pre-retirement ages.9,42 Although provider density may be relatively fixed, the provision of remote diagnostic and hearing aid fitting services (either through satellite clinics or telemedicine) may be able to mitigate regional differences in timing of healthcare.
CONCLUSION
Rural adults are at risk for delayed hearing aid acquisition compared to urban adults. This delay may be related to distance to hearing specialists and limited hearing healthcare specialists. Hearing aid recipients in rural communities have lower socioeconomic status than their urban counterparts. The timing of hearing aid acquisition is moderately inversely associated with the age at hearing loss onset. Rural adults reported that hearing loss was a significant barrier to completing education. Future research is warranted to assess key factors related to access of hearing healthcare.
Acknowledgments
Source of Funding: This work was supported by National Center for Advancing Translational Sciences and the University of Kentucky Center for Clinical and Translational Science (UL1TR000117) (SC), Triological Society Career Development Award (MLB), and National Institute of Deafness and Other Communication Disorders (1K23DC014074)(MLB). MLB is a member of the Surgical Advisory Board of Med El Corporation.
Footnotes
Conflicts of Interest The authors have no other financial relationships or conflicts of interest to disclose pertaining to the manuscript.
This research was presented at the American Otological Society Annual Meeting, Chicago, IL, USA, May 20–21, 2016.
SUPPLEMENTARY MATERIAL
Appendix: Hearing Healthcare Access Questionnaire and International Outcomes Inventory for Hearing Aids Questionnaire.
BIBLIOGRAPHY
- 1.Li CM, et al. Hearing impairment associated with depression in US adults, National Health and Nutrition Examination Survey 2005–2010. JAMA Otolaryngol Head Neck Surg. 2014;140(4):293–302. doi: 10.1001/jamaoto.2014.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Brennan-Jones CG, et al. Self-reported hearing loss and manual audiometry: A rural versus urban comparison. Aust J Rural Health. 2015 doi: 10.1111/ajr.12227. [DOI] [PubMed] [Google Scholar]
- 3.Chou C, et al. Association of socioeconomic position with sensory impairment among US working-aged adults. American Journal of Public Health. 2015;105(6):1262–1268. doi: 10.2105/AJPH.2014.302475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Service, U.-E.R. Rural-Urban Continuum Codes. 2013 5/10/2013 1/3/2016. ]; Available from: http://www.ers.usda.gov/data-products/rural-urban-continuum-codes.aspx.
- 5.Jung D, Bhattacharyya N. Association of Hearing Loss with Decreased Employment and Income Among Adults in the United States. Annals of Otology, Rhinology & Laryngology. 2012;121(12):771–775. doi: 10.1177/000348941212101201. [DOI] [PubMed] [Google Scholar]
- 6.Hjalte F, Brannstrom J, Gerdtham UG. Societal costs of hearing disorders: a systematic and critical review of literature. Int J Audiol. 2012;51(9):655–62. doi: 10.3109/14992027.2012.690077. [DOI] [PubMed] [Google Scholar]
- 7.Service, U.S.D.o.A.E.R. Rural America at a Glance: 2015 Edition. 2016 Jan; 3/6/2016]; Available from: http://www.ers.usda.gov/publications/eib-economic-information-bulletin/eib-145.aspx.
- 8.Monzani D1, Galeazzi GM, Genovese E, Marrara A, Martini A. Psychological profile and social behaviour of working adults with mild or moderate hearing loss. Acta Otorhinolaryngol Ital. 2008 Apr;28(2):61–6. [PMC free article] [PubMed] [Google Scholar]
- 9.Dalton DS, Cruickshanks KJ, Klein BE, Klein R, et al. The impact of hearing loss on quality of life in older adults. Gerontologist. 2003 Oct;43(5):661–8. doi: 10.1093/geront/43.5.661. [DOI] [PubMed] [Google Scholar]
- 10.Deal JA, Sharrett AR, Albert MS, Coresh J, et al. Hearing impairment and cognitive decline: a pilot study conducted within the atherosclerosis risk in communities neurocognitive study. Am J Epidemiol. 2015 May 1;181(9):680–90. doi: 10.1093/aje/kwu333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Smits C, Kramer SE, Houtgast T. Speech reception thresholds in noise and self-reported hearing disability in a general adult population. Ear & Hearing. 2006;27(5):538–549. doi: 10.1097/01.aud.0000233917.72551.cf. [DOI] [PubMed] [Google Scholar]
- 12.Smeeth L, et al. Reduced hearing, ownership, and use of hearing aids in elderly people in the UK–the MRC Trial of the Assessment and Management of Older People in the Community: a cross-sectional survey. The Lancet. 2002;359(9316):1466–1470. doi: 10.1016/s0140-6736(02)08433-7. [DOI] [PubMed] [Google Scholar]
- 13.Popelka M, et al. Low prevalence of hearing aid use among older adults with hearing loss: the epidemiology of hearing loss study. J of American Geriatric Society. 1998;46:1075–1078. doi: 10.1111/j.1532-5415.1998.tb06643.x. [DOI] [PubMed] [Google Scholar]
- 14.Bush M, Alexander D, Noblitt B, Lester C, Shinn J. Pediatric Hearing Healthcare in Kentucky’s Appalachian Primary Care Setting. J Community Health. 2015;40(4):762–8. doi: 10.1007/s10900-015-9997-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bush M, Hardin B, Rayle C, Lester C, Studts C, Shinn J. Rural Barriers to Early Diagnosis and Treatment of Infant Hearing Loss in Appalachia. Otology & Neurotology. 2015;36(1):93–98. doi: 10.1097/MAO.0000000000000636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cohen SM, Labadie RF, Haynes DS. Primary care approach to hearing loss: the hidden disability. Ear Nose Throat J. 2005;84(1):26, 29–31, 44. [PubMed] [Google Scholar]
- 17.Chou R, Dana T, Bougatsos C, Fleming C, Beil T. Screening adults aged 50 years or older for hearing loss: a review of the evidence for the US Preventive Services Task Force. Ann Intern Med. 2011;154(5):347–355. doi: 10.7326/0003-4819-154-5-201103010-00009. [DOI] [PubMed] [Google Scholar]
- 18.Milstein D, Weinstein BE. Effects of information sharing on follow-up after hearing screening for older adults. J Acad Rehab Audiol. 2002;(25):43–58. [Google Scholar]
- 19.Davis A, Smith P, Ferguson M, et al. Acceptability, benefit and costs of early screening for hearing disability: A study of potential screening tests and models. Health Technol Assess. 2007;(11):1–294. doi: 10.3310/hta11420. [DOI] [PubMed] [Google Scholar]
- 20.Windmill I, Freeman B. Demand for audiology services: 30-yr projections and impact on academic programs. J Am Acad Audiol. 2013;24(5):407–16. doi: 10.3766/jaaa.24.5.7. [DOI] [PubMed] [Google Scholar]
- 21.Brach C, Lewit EM, VanLandeghem K, Bronstein J, et al. Who’s enrolled in the State Children’s Health Insurance Program (SCHIP)? An overview of findings from the Child Health Insurance Research Initiative (CHIRI) Pediatrics. 2003;112:e499. [PubMed] [Google Scholar]
- 22.Liu CL, Zaslavsky AM, Ganz ML, Perrin J, et al. Continuity of health insurance coverage for children with special health care needs. Matern Child Health J. 2005;9:363–75. doi: 10.1007/s10995-005-0019-1. [DOI] [PubMed] [Google Scholar]
- 23.Sommers BD. From Medicaid to uninsured: drop-out among children in public insurance programs. Health Serv Res. 2005;40:59–78. doi: 10.1111/j.1475-6773.2005.00342.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bush M, Osetinsky M, Shinn JB, Gal TJ, Ding X, Fardo DW, Schoenberg N. Assessment of Appalachian Region Pediatric Hearing Healthcare Disparities and Delays. Laryngoscope. 2014;124(7):1713–7. doi: 10.1002/lary.24588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cox R, Alexander G. The international outcome inventory for hearing aids (IOI-HA): psychometric properties of the English version. Int J Audiol. 2002;41(1):30–35. doi: 10.3109/14992020209101309. [DOI] [PubMed] [Google Scholar]
- 26.Rural-Urban Continuum Codes. 2013 Available from: http://www.ers.usda.gov/data-products/rural-urban-continuum-codes.aspx.
- 27.Census 2000 Population Statistics. Office of Planning, Environment & Realty. United States Department of Transportation Federal Highway Administration; [Accessed April 28, 2015]. Available at: http://www.fhwa.dot.gov/planning/census_issues/archives/metropolitan_planning/cps2k.cfm. [Google Scholar]
- 28.Arcury T, et al. The Effects of Geography and Spatial Behavior on Health Care Utilization among the Residents of a Rural Region. Health Services Research. 2005;40(1):135–156. doi: 10.1111/j.1475-6773.2005.00346.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sanspree MJ, Allison C, Goldblatt SH, Pevsner D. Alabama Black Belt eye care--optometry giving back. Optometry (St Louis, Mo) 2008;79(12):724–729. doi: 10.1016/j.optm.2008.09.011. [DOI] [PubMed] [Google Scholar]
- 30.Mallow JA, Theeke LA, Long DM, Whetsel T, Theeke E, Mallow BK. Study protocol: mobile improvement of self-management ability through rural technology (mI SMART) SpringerPlus. 2015;4:423. doi: 10.1186/s40064-015-1209-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kochkin S. MarkeTrak VII: Obstacles to Adult Non-User Adoption of Hearing Aids. The Hearing Journal. 2007;60(4):24–51. [Google Scholar]
- 32.Bainbridge KE, Ramachandran V. Hearing aid use among older U.S. adults; the national health and nutrition examination survey, 2005–2006 and 2009–2010. Ear and hearing. 2014;35(3):289–294. doi: 10.1097/01.aud.0000441036.40169.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Laplante-Levesque A, Hickson L, Worrall L. Factors influencing rehabilitation decisions of adults with acquired hearing impairment. International journal of audiology. 2010;49(7):497–507. doi: 10.3109/14992021003645902. [DOI] [PubMed] [Google Scholar]
- 34.Oberg M, Marcusson J, Nagga K, Wressle E. Hearing difficulties, uptake, and outcomes of hearing aids in people 85 years of age. International journal of audiology. 2012;51(2):108–115. doi: 10.3109/14992027.2011.622301. [DOI] [PubMed] [Google Scholar]
- 35.Blazer DG, Landerman LR, Fillenbaum G, Horner R. Health services access and use among older adults in North Carolina: urban vs rural residents. American journal of public health. 1995;85(10):1384–1390. doi: 10.2105/ajph.85.10.1384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. [Accessed February 2, 2016];Health, United States, 2014. 2014 http://www.cdc.gov/nchs/data/hus/hus14.pdf#listfigures.
- 37.Eberhardt MS, Ingram DD, Makuc DM, et al. Urban and rural health chartbook: Health, United States 2001. Hyattsville, MD: National Center for Health Statistics; 2001. [Google Scholar]
- 38.Cox RM, Alexander GC, Gray GA. Hearing aid patients in private practice and public health (Veterans Affairs) clinics: are they different? Ear and hearing. 2005;26(6):513–528. doi: 10.1097/01.aud.0000188188.01311.0b. [DOI] [PubMed] [Google Scholar]
- 39.Brems C, Johnson ME, Warner TD, Roberts LW. Barriers to healthcare as reported by rural and urban interprofessional providers. Journal of interprofessional care. 2006;20(2):105–118. doi: 10.1080/13561820600622208. [DOI] [PubMed] [Google Scholar]
- 40.Van den brink R, Wit H, Kempen G, Van heuvelen M. Attitude and help-seeking for hearing impairment. British journal of audiology. 1996;30(5):313–324. doi: 10.3109/03005369609076779. [DOI] [PubMed] [Google Scholar]
- 41.Meister H, Walger M, Brehmer D, von Wedel UC, von Wedel H. The relationship between pre-fitting expectations and willingness to use hearing aids. International journal of audiology. 2008;47(4):153–159. doi: 10.1080/14992020701843111. [DOI] [PubMed] [Google Scholar]
- 42.Stephens D, et al. Hearing disability in people aged 50–65: effectiveness and acceptability of rehabilitative intervention. British Medical Journal. 1990;300(6723):508–511. doi: 10.1136/bmj.300.6723.508. [DOI] [PMC free article] [PubMed] [Google Scholar]