Abstract
Context: Patients with complete quadriplegia after high cervical spinal cord injury are fully dependent with activities of daily living. Assistive technology can improve their quality of life. We examined the use of a hybrid assistive limb for single joints (HAL-SJ) in a 19-year-old man with complete C4 quadriplegia due to chronic spinal cord injury to restore function of active elbow flexion. This is the first report on the use of the HAL-SJ in a patient with spinal cord injury.
Findings: The HAL-SJ intervention for each elbow was administered in 10 sessions. Clinical assessment using surface EMG was conducted to evaluate muscle activity of the trapezius, biceps brachii, infraspinatus, and triceps brachii muscle before, and during the 2nd, 3rd, 6th, and 9th interventions. Surface electromyography (EMG) before intervention showed no contraction in the upper arms, but in the bilateral trapezius. The HAL-SJ used motion intention from the right trapezius for activation. After the 6th and 7th session, respectively, biceps EMG showed that voluntary contraction and right elbow flexion could be performed by motion intention from the right biceps. After the 10th session, voluntary bicep contraction was possible. HAL-SJ treatment on the left elbow was performed using the same protocol with a similar outcome. After completing treatment on both upper extremities, both biceps contracted voluntarily, and he could operate a standard wheelchair for a short distance independently.
Conclusion: HAL-SJ intervention is feasible and effective in restoring elbow flexor function in a patient with C4 chronic spinal cord injury and complete quadriplegia.
Keywords: Hybrid assistive limb for single joint, Spinal cord injury, Complete quadriplegia, Active elbow flexion, Surface electromyography
Introduction
Individuals with complete quadriplegia from high cervical (around the level of C4) spinal cord injury (SCI) have extensive paralysis and are dependent for all aspects of their care, including activities of daily living (ADLs).1 Neurological recovery, especially for patients with complete SCI, is rare.2,3 Therefore, these patients’ rehabilitation plan should include environmental control systems to compensate for ADL loss.4,5
Regaining limb function is consistently reported as high priority by patients with SCI.6–8 Recently, assistive technology such as functional electrical stimulation (FES)9–11 and brain computer interface (BCI) technology7,8,12–18 has been developed. The aim of FES is to activate individual paralyzed muscles. BCI enables patients to control assistive devices, such as robotic limbs, by using neural signals recorded directly from the brain. However, those two technologies are still in the research stage. Some types of FES require invasive medical procedures to implant electrodes necessary to activate deep muscle. Large systems are often needed.
Exoskeleton robots are available for therapeutic use, including the InMotion ARM,19 WOTAS20 and ReoGo.21 The In-Motion ARM is a clinical version of MIT-MANUS.22 However, these are large systems and therefore may be challenging for the user to physically manage. For application in a clinical setting, portable devices are preferable. The Myomo e10023,24 is a portable upper limb therapeutic robot that has been used for patients with stroke.
The Hybrid Assistive Limb (HAL®) is a portable wearable robot that allows users to produce motion based on their voluntary drive and provides motion support to the lower limbs, of which we have previously reported experiences of its use on the lower extremity.25–30 The HAL® Single Joint type (HAL®-SJ; Cyberdyne Inc., Ibaraki, Japan) is developed for elbow or knee joint motion support (Fig. 1). A small power unit on the lateral side of the joint consists of angular sensors and actuators, and the primary control system consists of a cybernic voluntary control (CVC), based on the motion intention using the bioelectric signals generated by the patient's muscle activities.25 To the best of our knowledge, the HAL-SJ has been utilized in 2 cases: a patient with acute stroke,31 and postoperatively in a patient with total knee arthroplasty.32 This is the first report on the use of HAL-SJ for a patient with chronic SCI.
Figure 1.
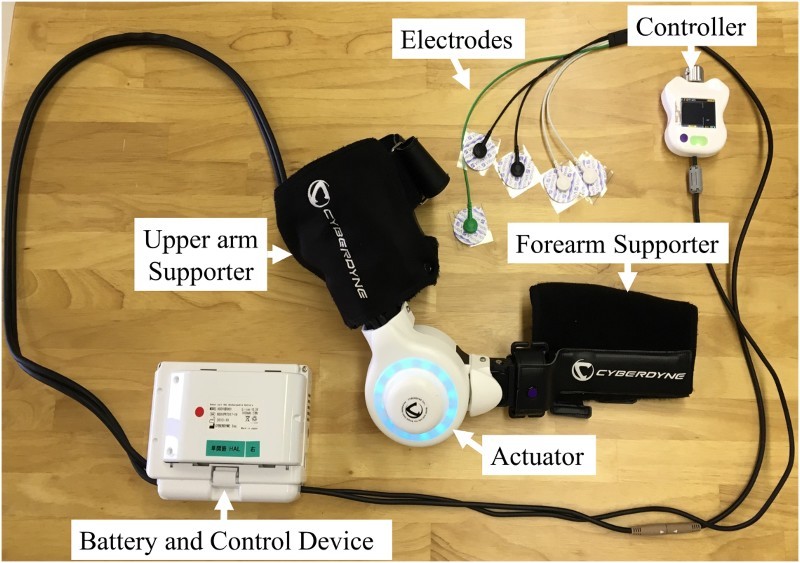
Hybrid assistive limb for single joint (HAL®-SJ). The HAL-SJ for the upper extremity is fitted with an upper arm supporter, forearm supporter, and small power unit placed laterally to the elbow. The power unit consists of angular sensor and an actuator. The controller is handheld and enables visual identification of bioelectric signals of the wearer. The whole system including electrodes for flexion, extension, and reference, and a control unit and battery.
Here, we used functional therapy to restore active elbow flexion using HAL-SJ in a patient with chronic SCI and C4 quadriplegia. We have also reported gait training in the same case using HAL for the lower limb.30 This is another study on the same patient. This study was conducted with the approval of the Ethics Committee of the Tsukuba University Faculty of Medicine.
Case presentation
Patient characteristics
A 19-year-old man with chronic SCI due to cervical vertebral fracture-dislocation (C3/4) had complete quadriplegia. He presented to our hospital 3 years and 8 months after injury for HAL intervention. His neurological examination before intervention revealed muscle weakness with a manual muscle testing (MMT) score of 5/5 in the trapezius muscle and an MMT score of 0/5 in the deltoid muscle, biceps brachii, supraspinatus muscle, infraspinatus muscle (C5 level), and below. Several months prior, at a previous hospital, FES was performed; motor paralysis was unchanged following FES.
He also had severe sensory disturbances below the neck. A slight sense of pressure remained in his right upper extremity and lower extremities, but no sensation remained in other areas. Articular contracture was not present. No urinary bladder or bowel function remained. Results of the blood and urine tests were normal. He seldom experienced orthostatic hypotension in a sitting position. He had taken antispasmogenic and anticholinergic medications for 3 years after the injury. He required comprehensive care, including feeding, changing clothes, bathing, and egestion. He used a head-controlled electric wheelchair to move independently. Magnetic resonance imaging (MRI) before intervention showed a signal change (high signal at T2WI, low signal at T1WI) of the spinal cord at the level of C3/4 (Fig. 2).
Figure 2.
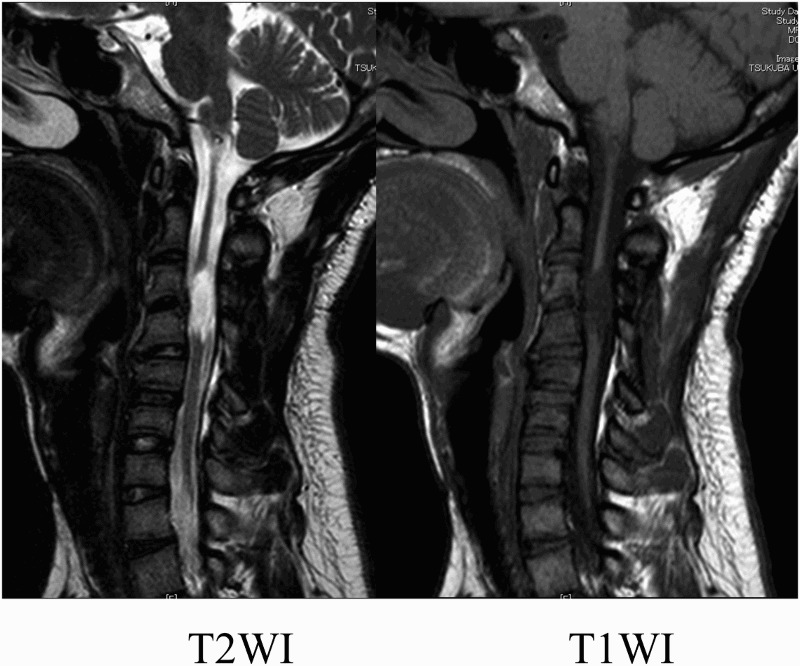
MRI findings before HAL-SJ intervention. Mid-sagittal section of T2-weighted and T1-weighted MR images before HAL intervention. The MR images show the signal changes in the spinal cord at the C3/4 level.
Clinical evaluation before intervention showed the following: grade A (complete motor lesion) on the American Spinal Injury Association (ASIA) impairment scale (AIS), an ASIA motor score (upper and lower limb total) of 0 points, an ASIA sensory score for light touch of 62 points (right: 31 points; left: 31 points), a Barthel Index of 5/100 points, and a Total Functional Independence Measure score of 53/126 points (motor for wheelchair, 18/91 points; cognitive, 35/35 points).
HAL-SJ intervention
The patient received HAL-SJ intervention (Fig. 3) for the right upper arm 2 times per week for 5 weeks (10 sessions) in addition to standard physical and occupational therapy in the hospital. Physical therapy consisted of range of motion exercise for spasticity and standing exercises for orthostatic hypotension. Occupational therapy consisted of exercise with a portable spring balancer for maintaining a good upper arm position, and neck muscle training. He had undergone similar standard therapy for about 3 years prior to HAL intervention. Each session with the HAL lasted 50 minutes, including rest and the time required to attach and detach the device (5 minutes to attach and 5 minutes to detach). The remaining time was allocated as follows: about 20 minutes for elbow flexion and extension exercise, about 10 minutes for resting, and 10 minutes for evaluation before and after HAL intervention. A medical doctor was on staff and present in case of an emergency, a therapist and a co-operator attached and detached the HAL, and an engineer implemented motion analysis.
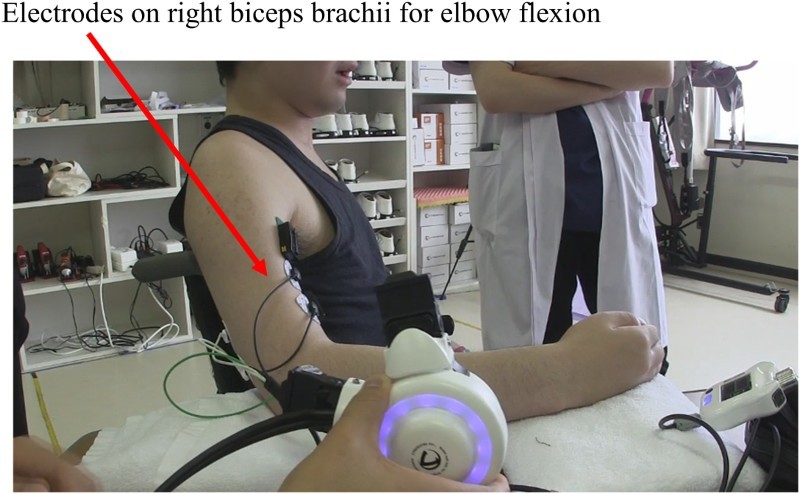
Figure 3.
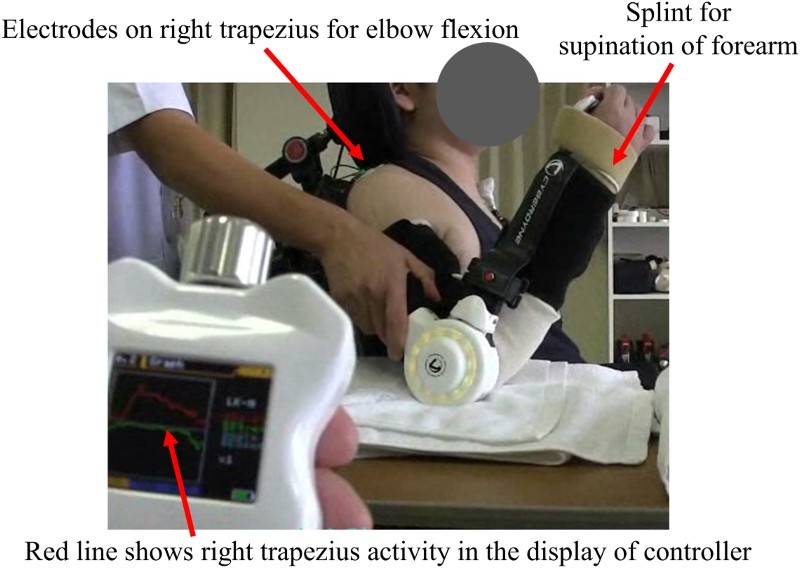
At the first HAL-SJ intervention. During the session, a therapist supported the patient's arm. A cock-up splint was used for maintaining the forearm in supination to align elbow flexion motion with the axis of the biceps muscle contraction. The display of the controller shows bioelectric signals from the right trapezius for elbow flexion as a red line.
A cock-up splint was used to keep the forearm supinated to fit the motion of the HAL-SJ to the axis of the biceps movement.
Twenty weeks after HAL-SJ intervention for the right upper extremity, intervention for the left upper extremity was performed for 12 weeks, once per 1 to 2 weeks (10 sessions) in the outpatient setting.
Clinical Assessment
Clinical assessments were conducted before and after intervention. A Trigno Lab wireless EMG system (Delsys, Massachusetts, USA) was used to evaluate muscle activity of the trapezius, biceps brachii, infraspinatus (ISP), and triceps brachii muscle before and during the 2nd, 3rd, 6th, and 9th intervention. Each muscle's activity was evaluated by the EMG which was collected at 2000Hz and filtered with a 30–400 Hz bandwidth passing filter; an activation envelop was computed by a 200 ms moving window average, using scripts on MATLAB 8.2 (Mathworks, Natick, MA, USA).
Results
Surface EMG before intervention showed no voluntary contraction in the bilateral upper arm, but in the bilateral trapezius (Fig. 4A). Elbow flexion could not be performed using HAL-SJ by placing the electrodes on the right biceps. Therefore, the electrodes for flexion were placed on the right trapezius and, for extension, on the left trapezius. Initially, voluntary right elbow flexion with HAL-SJ was performed by motion intention from the right trapezius in accordance with shoulder elevation. Over time, isometric contraction of the trapezius was performed; therefore, only elbow flexion was performed without shoulder elevation.
Figure 4.
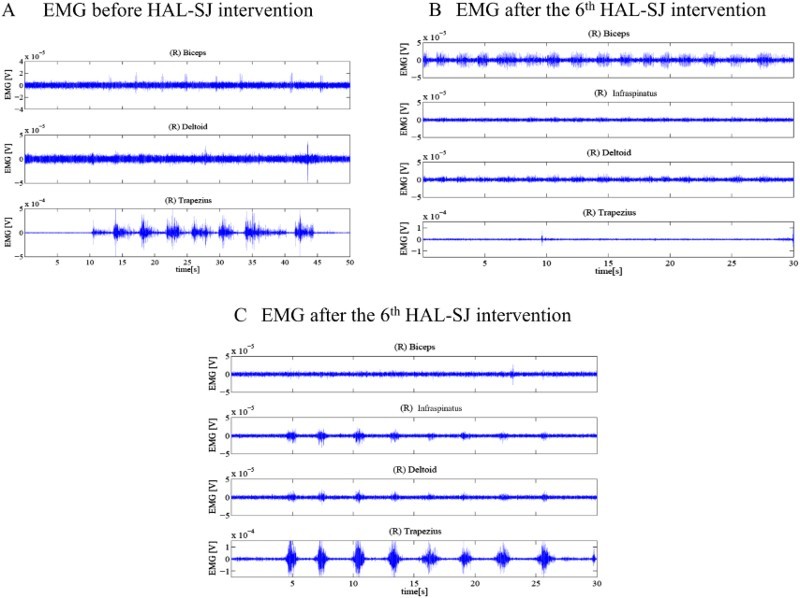
EMG in the right arm before and in the 6th HAL intervention. (A) EMG in the right arm before HAL-SJ intervention on the right side. There were voluntary contractions of the trapezius only. (B) EMG in the right arm after the 6th HAL-SJ intervention on the right side. There were voluntary contractions of the biceps brachii. (C) EMG in the right arm after the 6th HAL-SJ intervention on the right side. There was voluntary contraction of the infraspinatus and trapezius separate from biceps after the 6th HAL-SJ intervention on the right side.
After the 6th session, an EMG of the biceps showed voluntary contraction (Fig. 4B). At the same time, the right ISP displayed voluntary contraction separately from the right biceps (Fig. 4C). We placed the elbow flexion and extension electrodes on the right biceps and right triceps brachii, respectively, separately from the main HAL-SJ unit, to watch the movement of the HAL-SJ arm; this was done after a routine evaluation to confirm if the HAL could be triggered by the biceps muscle contraction to produce movement (see the linked video).
Right elbow flexion was observed through right biceps brachii contraction (Fig. 5). During the 7th session, voluntary right elbow flexion with HAL-SJ could be performed by placing the flexion electrodes for flexion on the right biceps. After the 10th intervention, he was able to contract the biceps voluntarily.
Figure 5.
After the 6th HAL-SJ intervention. Electrodes for flexion were placed on the biceps. Elbow flexion was triggered by the right biceps.
Following intervention on the right side, he was admitted to the hospital and continued to undergo standard physical and occupational therapy once every 1–2 weeks.
Twenty weeks after beginning intervention on the right side, intervention on the left side was started. At that time, it was difficult for him to voluntarily contract both biceps.
Muscle activity before intervention showed bilateral trapezius and left ISP voluntary contraction. During the first session, motion intention for left elbow flexion was taken from the left trapezius. After the 1st session, the muscle activity revealed voluntary contraction of the right biceps, despite only treating the left side.
Before the 2nd session, muscle activity showed voluntary contraction of the left biceps; therefore, the electrodes for flexion were placed on the left biceps. Before the 3rd session, there was no voluntary contraction of the left biceps, and the electrodes for flexion was placed on the left trapezius; however, after the intervention, the left biceps contracted voluntarily. After that, motion intention from the left biceps was used for left elbow flexion in all interventions. While there was only a slight voluntary contraction on the left side after each intervention, voluntary contraction on the right side became stable after each intervention on the left side. The session progression is summarized in Fig. 6. No adverse events associated with HAL-SJ intervention occurred.
Figure 6.

A summary of the HAL-SJ intervention. There were stained Red words for the first findings in EMG, or changes in the place of electrodes. *ISP, infraspinatus.
On clinical evaluation, Barthel Index and FIM scores remained unchanged. However, an increase in ASIA upper limb score from 0 to 2 was observed, along with an increase in MMT score of the bilateral biceps and bilateral ISP from 0 to 1.
Four months after completion of HAL intervention (1 year after HAL intervention initiation), the patient was able to voluntarily contract the bilateral biceps with right-sided dominance. After completion of HAL intervention, he underwent standard physical and occupational therapy once every 1 to 2 weeks, similar to the second (for the left side) intervention. He drove a standard wheelchair 10 meters by himself using elbow flexion during the clinical evaluation. This was done in the physical therapy room on a slightly uneven surface for about 2 minutes. We considered that this was not a practical setting; however, his progression of elbow flexion was evident.
Discussion
In this study, the HAL-SJ was used to produce active elbow flexion for a patient with complete quadriplegia from chronic SCI. The HAL is a wearable robotic device that can assist with movement according to the wearer's voluntary drive.26 The HAL- SJ is a portable device, which is convenient for clinical setting use, even for bedridden patients.
The present case used motion intention from the trapezius to produce elbow joint motion; the trapezius is a valuable muscle that remains neurologically intact in a patient with high cervical chronic SCI. He could contract the bilateral biceps voluntarily after HAL-SJ intervention. Voluntary elbow flexion using the HAL-SJ might provide systematic feedback and is considered to have motor learning effects.
Dally and Ruff12 describe the critical principles of motor learning for central nervous system plasticity as requiring five characteristics: near-normal movements, muscle activation driving movement practice, focused attention, repetition of desired movements, and training specificity. The motion using HAL-SJ, which is derived from volitional contraction of residual neurologically intact muscle, may allow plasticity to occur within the central nervous system.
FES is a type of assistive technology used for rehabilitation.9–11 This mode was used in the biceps at the previous hospital in our patient; however, there was no effect on active elbow flexion. Elbow flexion using the HAL-SJ had both visual and performance feedback, which were reported to be effective for motor learning.14
Mateo et al.33 reviewed studies on motor imagery training, mainly grasping, for patients with tetraplegia due to cervical SCI. They state that change in motor performance and brain plasticity reflect functional and structural changes within the central nervous system, enabling the improvement of compensated movements.
In the present case, HAL-SJ intervention resulted in active biceps contraction and might cause functional changes in the central nervous system. Interestingly, after HAL-SJ intervention for the right upper extremity, the bilateral infraspinatus (a shoulder rotator) could be voluntarily contracted and, after intervention for the left upper extremity, the right biceps could be voluntarily contracted. This volitional control of C5 level muscles, paralyzed before HAL-SJ intervention, was substantial to suggest that plasticity occurs within the central nervous system.
There are some limitations in our study. We only evaluated muscle activity through surface EMG and did not measure brain activity. In the future, we intend to evaluate changes in the central nervous system by using near-infrared spectroscopy during HAL intervention or functional MRI before and after HAL intervention.
In this case, we investigated the feasibility of rehabilitation using the HAL-SJ in an individual with C4 quadriplegia, and confirmed that HAL-SJ intervention could be implemented safely and result in positive outcomes. No HAL-SJ intervention-related adverse events occurred.
To our knowledge, there is no report regarding HAL-SJ intervention for patients with SCI. In the current case, voluntary control of the bilateral biceps emerged after HAL-SJ intervention. He had been fully dependent with the exception of locomotion through a head-controlled electric wheelchair before HAL intervention. After the intervention, he was able to actively contract bilateral elbow flexors and drive a standard wheelchair for a short distance; this was not practical ambulation, but did indicate functional improvement.
Conclusion
The HAL-SJ enabled a patient with complete quadriplegia after chronic high cervical SCI to voluntarily contract the bilateral biceps. The HAL-SJ is feasible and effective in restoring elbow flexion allowing for functional enhancement in patients with chronic SCI.
Supplementary Material
Acknowledgements
We thank Mayuko Sakamaki and Yumiko Ito, Center for Innovative Medicine and Engineering (CIME), University of Tsukuba Hospital, for their excellent technical assistance.
Disclaimer statements
Declaration of Interest None.
Funding This study was supported by the Industrial Disease Clinical Research Grants of the Ministry of Health Labour and Welfare, Japan (14060101-01).
Ethics approval This study was conducted with approval from the Ethics Committee of the Tsukuba University Faculty of Medicine.
Informed consent Written informed consent was obtained from the patient for publication of this case report and accompanying images.
Supplementary material
Supplementary Material for this article available here: 10.1080/10790268.2017.1313931
ORCID
Yukiyo Shimizu http://orcid.org/0000-0001-7491-4516
Akira Ikumi http://orcid.org/0000-0001-6034-1593
Akira Matsushita http://orcid.org/0000-0003-2335-674X
References
- 1.Memberg WD, Polasek KH, Hart RL, Bryden AM, Kilgore KL, Nemunaitis GA, et al. Implanted neuroprosthesis for restoring arm and hand function in people with high level tetraplegia. Arch Phys Med Rehabil 2014;95(6):1201–11.e1 doi: 10.1016/j.apmr.2014.01.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kirshblum S, Millis S, McKinley W, Tulsky D.. Late neurologic recovery after traumatic spinal cord injury. Arch Phys Med Rehabil 2004;85(11):1811–7. doi: 10.1016/j.apmr.2004.03.015 [DOI] [PubMed] [Google Scholar]
- 3.Lim PA, Tow AM.. Recovery and regeneration after spinal cord injury: a review and summary of recent literature. Ann Acad Med Singapore 2007;36(1):49–57. [PubMed] [Google Scholar]
- 4.McDonald DW, Boyle MA, Schumann TL.. Environmental control unit utilization by high-level spinal cord injured patients. Arch Phys Med Rehabil 1989;70(8):621–3. [PubMed] [Google Scholar]
- 5.Craig A, Tran Y, McIsaac P, Boord P.. The efficacy and benefits of environmental control systems for the severely disabled. Med Sci Monit 2005;11(1):Ra32–9. [PubMed] [Google Scholar]
- 6.Anderson KD. Targeting recovery: priorities of the spinal cord-injured population. J Neurotrauma 2004;21(10):1371–83. doi: 10.1089/neu.2004.21.1371 [DOI] [PubMed] [Google Scholar]
- 7.Jackson A, Zimmermann JB.. Neural interfaces for the brain and spinal cord--restoring motor function. Nat Rev Neurol 2012;8(12):690–9. doi: 10.1038/nrneurol.2012.219 [DOI] [PubMed] [Google Scholar]
- 8.Collinger JL, Boninger ML, Bruns TM, Curley K, Wang W, Weber DJ.. Functional priorities, assistive technology, and brain-computer interfaces after spinal cord injury. J Rehabil Res Dev 2013;50(2):145. doi: 10.1682/JRRD.2011.11.0213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hara Y, Obayashi S, Tsujiuchi K, Muraoka Y.. The effects of electromyography-controlled functional electrical stimulation on upper extremity function and cortical perfusion in stroke patients. Clin Neurophysiol 2013;124(10):2008–15. doi: 10.1016/j.clinph.2013.03.030 [DOI] [PubMed] [Google Scholar]
- 10.Naito A, Shimizu Y, Handa Y, Ichie M, Hoshimiya N.. Functional anatomical studies of the elbow movements. I. Electromyographic (EMG) analysis. Okajimas Folia Anat Jpn 1991;68(5):283–8. doi: 10.2535/ofaj1936.68.5_283 [DOI] [PubMed] [Google Scholar]
- 11.Shimada Y, Sato K, Kagaya H, Konishi N, Miyamoto S, Matsunaga T.. Clinical use of percutaneous intramuscular electrodes for functional electrical stimulation. Arch Phys Med Rehabil 1996;77(10):1014–8. doi: 10.1016/S0003-9993(96)90061-1 [DOI] [PubMed] [Google Scholar]
- 12.Daly JJ, Ruff RL.. Construction of efficacious gait and upper limb functional interventions based on brain plasticity evidence and model-based measures for stroke patients. ScientificWorldJournal 2007;7:2031–45. doi: 10.1100/tsw.2007.299 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Birbaumer N, Cohen LG.. Brain-computer interfaces: communication and restoration of movement in paralysis. J Physiol 2007;579(Pt 3):621–36. doi: 10.1113/jphysiol.2006.125633 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Buch E, Weber C, Cohen LG, Braun C, Dimyan MA, Ard T, et al. Think to move: a neuromagnetic brain-computer interface (BCI) system for chronic stroke. Stroke 2008;39(3):910–7. doi: 10.1161/STROKEAHA.107.505313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Courtine G, Micera S, DiGiovanna J, del R Millán J.. Brain–machine interface: closer to therapeutic reality?. Lancet 2013;381(9866):515–7. doi: 10.1016/S0140-6736(12)62164-3 [DOI] [PubMed] [Google Scholar]
- 16.Daly JJ, Wolpaw JR.. Brain-computer interfaces in neurological rehabilitation. Lancet Neurol 2008;7(11):1032–43. doi: 10.1016/S1474-4422(08)70223-0 [DOI] [PubMed] [Google Scholar]
- 17.Dobkin BH. Brain-computer interface technology as a tool to augment plasticity and outcomes for neurological rehabilitation. J Physiol 2007;579(Pt 3):637–42. doi: 10.1113/jphysiol.2006.123067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cincotti F, Mattia D, Aloise F, Bufalari S, Schalk G, Oriolo G, et al. Non-invasive brain–computer interface system: Towards its application as assistive technology. Brain Res Bull 2008;75(6):796–803. doi: 10.1016/j.brainresbull.2008.01.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Duret C, Courtial O, Grosmaire AG, Hutin E.. Use of a robotic device for the rehabilitation of severe upper limb paresis in subacute stroke: exploration of patient/robot interactions and the motor recovery process. BioMed Res Int 2015;2015:482389. doi: 10.1155/2015/482389 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rocon E, Belda-Lois JM, Ruiz AF, Manto M, Moreno JC, Pons JL.. Design and validation of a rehabilitation robotic exoskeleton for tremor assessment and suppression. IEEE Trans Neural Syst Rehabil Eng 2007;15(3):367–78. doi: 10.1109/TNSRE.2007.903917 [DOI] [PubMed] [Google Scholar]
- 21.Bovolenta F, Goldoni M, Clerici P, Agosti M, Franceschini M.. Robot therapy for functional recovery of the upper limbs: a pilot study on patients after stroke. J Rehabil Med 2009;41(12):971–5. doi: 10.2340/16501977-0402 [DOI] [PubMed] [Google Scholar]
- 22.Krebs HI, Volpe BT, Aisen ML, Hogan N.. Increasing productivity and quality of care: robot-aided neuro-rehabilitation. J Rehabil Res Dev 2000;37(6):639–52. [PubMed] [Google Scholar]
- 23.Stein J. e100 NeuroRobotic system. Expert Rev Med Devices. 2009;6(1):15–9. doi: 10.1586/17434440.6.1.15 [DOI] [PubMed] [Google Scholar]
- 24.Page SJ, Hill V, White S.. Portable upper extremity robotics is as efficacious as upper extremity rehabilitative therapy: a randomized controlled pilot trial. Clin Rehabil 2013;27(6):494–503. doi: 10.1177/0269215512464795 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kawamoto H, Sankai Y.. Power assist method based on Phase Sequence and muscle force condition for HAL. Advanced Robotics. 2005;19(7):717–34. doi: 10.1163/1568553054455103 [DOI] [Google Scholar]
- 26.Kawamoto H, Kamibayashi K, Nakata Y, Yamawaki K, Ariyasu R, Sankai Y, et al. Pilot study of locomotion improvement using hybrid assistive limb in chronic stroke patients. BMC Neurol 2013;13:141. doi: 10.1186/1471-2377-13-141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kubota S, Nakata Y, Eguchi K, Kawamoto H, Kamibayashi K, Sakane M, et al. Feasibility of rehabilitation training with a newly developed wearable robot for patients with limited mobility. Arch Phys Med Rehabil 2013;94(6):1080–7. doi: 10.1016/j.apmr.2012.12.020 [DOI] [PubMed] [Google Scholar]
- 28.Fujii K, Abe T, Kubota S, Marushima A, Kawamoto H, Ueno T, et al. The voluntary driven exoskeleton Hybrid Assistive Limb (HAL) for postoperative training of thoracic ossification of the posterior longitudinal ligament: a case report. J Spinal Cord Med 2016:1–7. doi: 10.1080/10790268.2016.1142056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Fujii K, Abe T, Kubota S, Marushima A, Kawamoto H, Ueno T, Matsushita A, et al. The voluntary driven exoskeleton Hybrid Assistive Limb (HAL) for postoperative training of thoracic ossification of the posterior longitudinal ligament: a case report. J Spinal Cord Med 2016:1–7. doi: 10.1080/10790268.2016.1142056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ikumi A, Kubota S, Shimizu Y, Kadone H, Marushima A, Ueno T, et al. Decrease of spasticity after hybrid assistive limb® training for a chronic spinal cord injury patient with C4 quadriplegia. J Spinal Cord Med 2016: 1–6. doi: 10.1080/10790268.2016.1225913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Fukuda H, Morishita T, Ogata T, Saita K, Hyakutake K, Watanabe J, et al. Tailor-made rehabilitation approach using multiple types of hybrid assistive limb robots for acute stroke patients: A pilot study. Assist Technol 2016;28(1):53–6. doi: 10.1080/10400435.2015.1080768 [DOI] [PubMed] [Google Scholar]
- 32.Yoshioka T, Sugaya H, Kubota S, Onishi M, Kanamori A, Sankai Y, et al. Knee-Extension Training with a Single-Joint Hybrid Assistive Limb during the Early Postoperative Period after Total Knee Arthroplasty in a Patient with Osteoarthritis. Case Rep Orthop 2016;2016:9610745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mateo S, Di Rienzo F, Bergeron V, Guillot A, Collet C, Rode G.. Motor imageryreinforces brain compensation of reach-to-grasp movement after cervical spinalcord injury. Front Behav Neurosci 2015;9:234. doi: 10.3389/fnbeh.2015.00234 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


