Figure 3. The late immunosuppressive effects of sepsis.
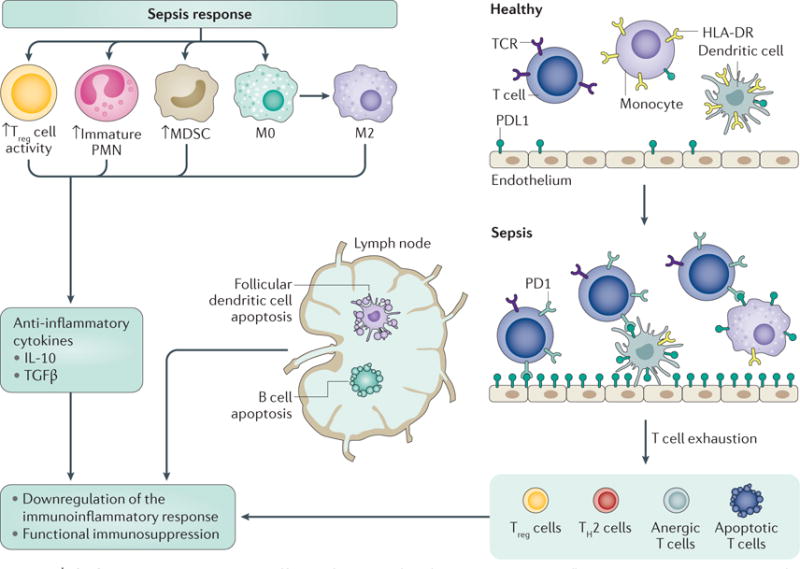
After the transitory acute inflammatory response, sepsis results in an immunocompromised state. Immunosuppressive immature polymorphonuclear leukocytes (PMNs) and myeloid-derived suppressor cells (MDSCs) mobilize from the bone marrow and monocyte differentiation skews to the production of M2 macrophages (which decrease inflammation and promote tissue repair). Although these responses can be considered normal, if the source of infection is not controlled, the continued responses rapidly become pathological and lead to chronic immune suppression. Together, immature PMNs, MDSCs and M2 macrophages produce anti-inflammatory cytokines, such as IL-10 and transforming growth factor-β (TGFβ). Professional antigen-presenting cells, including dendritic cells and macrophages, reduce the expression of the activating major histocompatibility complex (MHC) class II molecule human leukocyte antigen-antigen D related (HLA-DR). T cells and stromal cells upregulate negative co-stimulatory molecules, including programmed death protein 1 (PD1) and programmed death ligand 1 (PDL1), respectively, to drive the expansion of regulatory T (Treg) cells and anergic (unresponsive) T cells. Follicular dendritic cells, B cells and T cells undergo apoptosis, further abrogating the immune response. TCR, T cell receptor; TH2, T helper 2.
